
Efficacy and safety analysis of high-flow nasal cannula in children with bronchiolitis: a systematic review and meta-analysis
Introduction
Pediatric bronchiolitis is an acute infection of the lower respiratory tract, affecting infants under 2 years of age. It usually involving the bronchioles, and causes a persistent dry cough and episodic dyspnea 2–3 days after infection of the upper respiratory tract. The most significant feature of this disease is the concomitant dry cough and dyspnea. In addition, emphysema and thoracic expansion as well as compression of the abdomen often affect the milk sucking and eating of infants and young children. Severe cases involve prominent obstructive emphysema, pallor, and cyanosis (1). Numerous factors influence the onset of bronchiolitis in infants and young children, the most important of which is viral infection. Miron et al. found that 91% of cases with acute bronchiolitis (AB) can be diagnosed from sputum or nasal wash samples. In addition, respiratory syncytial virus (RSV) was detectable in 76% of samples, and RSV was the only virus present in nearly half of the specimens (2). One of clinical studies has shown that as much as 50% of infants and young children suffering from chronic bronchiolitis experience asthma (3). However, in recent years, due to factors such as the environment and climate, the incidence of bronchiolitis in infants and young children has been increasing, becoming one of the most common causes of hospital admissions among infants worldwide, which has seriously affected the health of infants and young children and has brought an enormous burden to families and society.
The severity of bronchiolitis is the key to treatment, and oxygen therapy is the most common treatment for children with bronchiolitis. Warming and humidifying high-flow transnasal catheter oxygen therapy allows for accurate oxygen concentration (21–100%) through the air-oxygen mixing device. The heating reaches 37 ℃ and the humidification reaches 100% relative humidity, thereby providing high gas flow (4,5). A breathing support device based on the patient’s breathing flow can improve the breathing and generate positive pressure at the end of the breath. In addition, it has the advantages of having a simple operation, good tolerance, and high safety performance. A cost-utility analysis showed that the application of high-flow nasal catheter (HFNC) in emergencies can better utilize limited health resources compared to traditional treatments (1). Since its application in clinical treatment in 2000, it has received widespread attention in pediatric respiratory diseases (6-8).
However, HFNC has problems such as poor airway protection ability, high risk of aspiration, unstable hemodynamics, and the need to apply vasoactive drugs. Some scholars even found that the failure of HFNC may lead to delayed intubation and poor clinical outcomes (9). Therefore, the comparison between standard oxygen therapy and NCPAP and HFNC in children with bronchiolitis is still controversial. Based on this, this study aims to evaluate the safety and efficacy of warming, humidifying, high-flow transnasal catheter oxygen therapy on the treatment of different degrees of infant bronchiolitis through Meta-analysis. We present the following article in accordance with the PRISMA reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-73/rc).
Methods
Search strategy
We searched PubMed, Web of Science, and major Chinese biomedical databases, including CNKI, GeenMedical, Wanfang, and Weipu using the following keywords: children with respiratory diseases, infant bronchiolitis, bronchiolitis treatment, HFNCs, warming and humidifying high-flow, nasal catheter oxygen inhalation, and conventional oxygen therapy. The publication time was set from the establishment of the database to October 2021. Selected articles were randomized controlled trial (RCT) studies in which the patients were less than 16 years old and the experimental group was treated with HFNCs, and the control group was treated with nCPAP or conventional oxygen. After extracting the data, the study subjects were divided into HFNC treatment and control groups according to the different intervention methods.
Inclusion and exclusion criteria
Inclusion criteria
Study type: RCT.
Research subjects: (I) <16 years old; and (II) clinically diagnosed with bronchiolitis, SpO2 <92%.
Intervention measures: experimental group received HFNC treatment.
Outcome indicators: mainly the failure rate of HFNC treatment, respiratory rate (RR), and oxygen saturation changes.
Treatment failure: refers to sudden cardiac arrest, extreme respiratory weakness, and tracheal intubation.
Secondary indicators: length of hospital stay, total treatment time, HFNC treatment flow, response to HFNC treatment, mortality, and cause of death.
Exclusion criteria
The exclusion criteria were as follows: (I) non-English and non-Chinese documents or documents without full text; (II) studies with incomplete original data, the contact author has not responded, or the research cannot be extracted and utilized; (III) very low quality literature; and (IV) duplicate publications.
Paper screening and risk of bias
Based on the inclusion and exclusion criteria, two reviewers performed independent evaluations of the titles and abstracts of the articles to determine whether they could be included in this study. If both reviewers agreed that a paper satisfied the criteria, the entire essay was evaluated. Disagreements about whether an article met the inclusion criteria were resolved through discussion. If an agreement could not be reached, a third reviewer would make the final decision. The reviewers contacted the authors of the seven selected articles for additional information required for this article. The Cochrane Risk of Bias Tool was used to assess the quality and risk of bias of the included articles.
Data extraction
The articles included in this meta-analysis were RCTs. Infants who met the inclusion and exclusion criteria were randomly assigned to an experimental group (receiving HFNC treatment) and a control group. Two reviewers independently extracted the data in the article based on the pre-established datasheet, which included the first author’s name, country, year of publication, journal name, and patient demographic data. The recorded results included HFNC treatment failure rate, RR and oxygen saturation changes, hospital stay, total treatment time (PICU and PED), HFNC treatment schedule, response to HFNC treatment, mortality, and cause of death. The two reviewers exchanged data sheets and checked, discussed, and unified the differences in the extracted data.
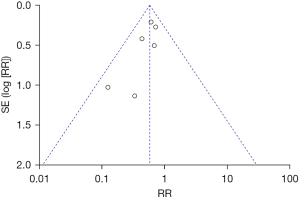
Statistical analysis
Percentages and relative risk (RR) or mean difference (MD) with 95% confidence interval (CI) were used to describe the data. The I2 test was used to assess the heterogeneity; if the heterogeneity between studies was small (P>0.1, I2<50%), the fixed-effects model was used to merge the effect sizes; however, if the heterogeneity between studies was obvious (P≤0.1, I2≥50%), the random effects was is used to merge the effect size. Statistical analysis and graphs were performed using RevMan 5.30 software provided by Cochrane Collaboration. P≤0.05 (two-sided), the difference was considered statistically significant and the test of sources of heterogeneity. A funnel plot was used to check the risk of publication bias.
Results
Search results and study characteristics
In total, 1,379 related records were initially retrieved from the databases. Before screening, 97 duplicate records were deleted, 385 unqualified records were removed. Of the 897 papers that were obtained through screening, 256 were excluded due to being low quality, leaving 641 articles, and of these, 114 failed to be retrieved. The remaining 527 items were evaluated. After the two reviewers thoroughly read the complete texts, 520 articles were excluded according to the exclusion criteria, and seven articles were finally obtained. The specific literature retrieval process is shown in Figure 1.
The seven included articles were RCTs, including four foreign studies, three domestic studies. Four were comparative studies between nasal continuous positive airway pressure (nCPAP) and HFNC treatment, and three were comparative studies between standard oxygen therapy and HFNC treatment. All of the selected articles involved an accurate diagnosis of bronchiolitis, and all met the inclusion and exclusion criteria. There were 436 cases in the HFNC treatment group and 405 cases in the control group. The essential characteristics of these articles are shown in Table 1.
Table 1
| Author | Country | Year | Journal | HFNC | Control |
|---|---|---|---|---|---|
| Mayfield S et al. (10) | Australia | 2014 | J Paediatr Child Health | 61 | 33 |
| Durand P et al. (11) | France | 2020 | Eur Respir J | 133 | 135 |
| Milési C et al. (12) | France | 2017 | Intensive Care Med | 71 | 71 |
| Ramnarayan P et al. (13) | UK | 2018 | Crit Care | 59 | 54 |
| Shi F et al. (14) | China | 2021 | Clinical Medicine | 30 | 30 |
| Li J (15) | China | 2020 | Journal of Pediatric Pharmacy | 45 | 45 |
| Li Y et al. (16) | China | 2021 | Chinese and Foreign Medical Research | 37 | 37 |
HFNC, high-flow nasal cannula.
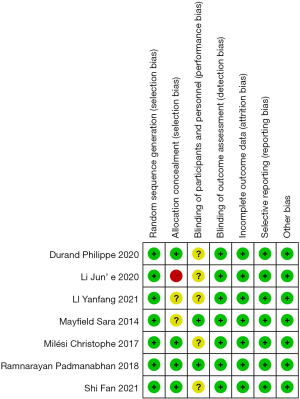
All seven articles described random sequence generation, four articles reported on allocation concealment, one article did not use allocation concealment, two studies did not report on allocation concealment, only two articles reported on the double-blind method, and five articles did not report on the double-blind process. All articles described the complete blinding of outcome evaluation bias, outcome data bias, selective reporting bias, and other risk biases. The quality evaluation results are shown in Figure 2.
Meta-analysis results
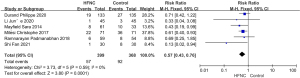
Failure rate of treatment
According to the inclusion and exclusion criteria, six articles were included to analyze the number of patients who failed treatment after nCPAP or standard oxygen therapy and HFNC therapy. These included 57 patients who failed HFNC treatment and 92 patients in the control group who failed nCPAP The analysis results showed that (P=0.59, I2=0%), indicating that the number of failed patients between the HFNC treatment group and the control group was uniform, so a fixed-effect model was used for joint analysis. The combined effect size RR was 0.57, 95% CI: 0.43–0.76, as shown in Figure 3. The complete effect size test results were Z=3.80, P=0.0001 (<0.05), and the meta-analysis results confirmed that there was a statistically significant difference in the number of patients with bronchiolitis after nCPAP or standard oxygen therapy and HFNC therapy.
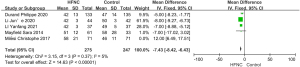
Change in respiratory rate
A total of five articles on the changes in respiratory rate (RR) were included. Bronchiolitis is characterized by wheezing during onset. There is also a significant increase in breathing when gasping, up to 60 to 80 times per minute, which is significantly reduced after treatment. Therefore, RR change is an important indicator to evaluate the therapeutic effect of bronchiolitis.
There were 275 patients treated with HFNC and 247 patients in the control group. The analysis results showed that (P=0.37, I2=5%), indicating that the RR changes between the experimental and control groups were uniform, so the fixed-effects model was used for joint analysis. The combined effect size MD was −7.43 (95% CI: −8.42 to −6.43), as shown in Figure 4. The result of the comprehensive effect size test was Z=14.63, P<0.00001; therefore, the meta-analysis results suggested that the difference in RR between the nCPAP or standard oxygen therapy group and the HFNC treatment group was statistically significant.
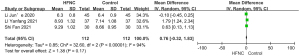
Improved arterial partial pressure of oxygen
Blood oxygen partial pressure refers to the pressure produced by physically dissolved oxygen molecules (O2) in the blood. Under normal circumstances, PaO2 ranges from 12.6 to 13.3 kPa. Patients with bronchiolitis will experience varying degrees of hypoxia, which leads to a decrease in PaO2, and thus, the degree of increase in PaO2 is also an important indicator of the treatment effect. A total of three articles with PaO2 changes were included in this study, including 112 patients treated with HFNC and 112 patients in the control group. The analysis results showed that (P<0.00001, I2=94%), indicating that the PaO2 uniformity between the experimental and control groups was not good, so the random effects model was used for joint analysis. The combined effect size MD was 0.76 (95% CI: –0.32 to 1.83), as shown in Figure 5. The results of the comprehensive effect size test were Z=1.38, P=0.17. The meta-analysis results indicated that the difference in PaO2 changes between the nCPAP or standard oxygen therapy group and the HFNC treatment group was not statistically significant.
Publication bias
The funnel chart was used to assess the publication bias of treatment failure in the two groups of patients. It contains a total of six articles. The funnel chart exhibited asymmetry, indicating that there may be publication bias, as shown in Figure 6.
Risk of bias
All seven eligible studies described the risk of random sequence generation as low. Four articles reported low risk of allocation bias (11-14), the risk of implicit bias in the allocation of two articles was not yet clear (10,16), and the risk of implicit bias in the allocation of one article was high (15). The risk of blinding participants in two articles was low (10,13), while the risk in the other five articles was unclear (11,12,14-16). All studies judged that the risk of result evaluation bias, incomplete result data bias, selective reporting domain bias and other biases was low, as shown in Figure 7.
Discussion
The warming and humidifying function of HFNC can adequately protect the respiratory mucosa, enhance the cleaning ability of mucosal cilia, keep the respiratory tract moist and unobstructed, maintain normal respiratory function, and effectively prevent other lung infections caused during treatment (17). In recent years, the use of heated and humidified HFNC to provide oxygen to treat children with different degrees of bronchiolitis or mild to moderate hypoxemia has become increasingly popular. The results of this meta-analysis showed that the failure rate of HFNC treatment for children with bronchiolitis was significantly lower than the failure rate of nCPAP or standard oxygen therapy under the same circumstances, which is consistent with the results of other studies. However, there is also one study showing that the treatment failure rate of the HFNC group is higher than that of the nCPAP group, and therefore, our results may be due to the bias caused by combining the number of failures of nCPAP treatment with the number of failures of standard oxygen therapy (18).
The analysis results of respiratory rate change showed that the effect of HFNC treatment is more effective than the control group, but the analysis results of arterial oxygen partial pressure showed that there was no difference between HFNC treatment and nCPAP or standard oxygen therapy, which is inconsistent with the previous research results (14-16). We speculate that this is due to the small number of included articles.
This article has certain limitations that should be noted. Due to the small sample size of the analysis, the results are insufficient to support the conclusion, thereby limiting the robustness of this research. The age limit of the study subjects and the differing severities of bronchiolitis resulted in certain limitations in extrapolating of the results of this study. In future, multi-center, large-sample research should be carried out, and RCTs should be used to study the effect of HFNC treatment on patients with different ages and degrees of bronchiolitis in depth.
Conclusions
In summary, although the results of this study showed that HFNC treatment does not contribute to the increase of arterial oxygen partial pressure more than positive airway pressure or standard oxygen therapy, it can significantly reduce the risk of bronchiolitis in children, the treatment failure rate, and the breathing rate. However, the study has shortcomings such as a small number of patients. In the future, multi-center, large sample size studies should be conducted to explore the effect of HFNC treatment in children with different degrees of bronchiolitis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist Available at https://tp.amegroups.com/article/view/10.21037/tp-22-73/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-73/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Buendía JA, Acuña-Cordero R, Rodriguez-Martinez CE. The cost-utility of early use of high-flow nasal cannula in bronchiolitis. Health Econ Rev 2021;11:41. [Crossref] [PubMed]
- Miron D, Srugo I, Kra-Oz Z, et al. Sole pathogen in acute bronchiolitis: is there a role for other organisms apart from respiratory syncytial virus? Pediatr Infect Dis J 2010;29:e7-e10. [Crossref] [PubMed]
- Su M, Li C. Current Perspective on Respiratory Syncytial Virus Caused Bronchiolitis and Link with Children Asthma A. Chinese Medical Association, Chinese Society of Allergology, Chinese Medical Association. Program & Abstracts of the 8th Congress of Asia Pacific Association of Pediatric Allergy Respirology & Immunology (APAPARI). Chinese Medical Association, Chinese Society of Allergology, Chinese Medical Association, 2009:2.
- Rubin S, Ghuman A, Deakers T, et al. Effort of breathing in children receiving high-flow nasal cannula. Pediatr Crit Care Med 2014;15:1-6. [Crossref] [PubMed]
- Hawkins S, Huston S, Campbell K, et al. High-Flow, Heated, Humidified Air Via Nasal Cannula Treats CPAP-Intolerant Children With Obstructive Sleep Apnea. J Clin Sleep Med 2017;13:981-9. [Crossref] [PubMed]
- Zielińska A, Jassem-Bobowicz JM, Kwiatkowska J. Oxygen therapy with high-flow nasal cannulas in children with acute bronchiolitis. Anaesthesiol Intensive Ther 2019;51:51-5. [Crossref] [PubMed]
- Sachs N, Rom E, Schonfeld T, et al. Short-Term High-Flow Nasal Cannula for Moderate to Severe Bronchiolitis Is Effective in a General Pediatric Ward. Clin Pediatr (Phila) 2019;58:1522-7. [Crossref] [PubMed]
- Horvat CM, Pelletier JH. High-Flow Nasal Cannula Use and Patient-Centered Outcomes for Pediatric Bronchiolitis. JAMA Netw Open 2021;4:e2130927. [Crossref] [PubMed]
- Metge P, Grimaldi C, Hassid S, et al. Comparison of a high-flow humidified nasal cannula to nasal continuous positive airway pressure in children with acute bronchiolitis: experience in a pediatric intensive care unit. Eur J Pediatr 2014;173:953-8. [Crossref] [PubMed]
- Mayfield S, Bogossian F, O'Malley L, et al. High-flow nasal cannula oxygen therapy for infants with bronchiolitis: pilot study. J Paediatr Child Health 2014;50:373-8. [Crossref] [PubMed]
- Durand P, Guiddir T, Kyheng C, et al. A randomised trial of high-flow nasal cannula in infants with moderate bronchiolitis. Eur Respir J 2020;56:1901926. [Crossref] [PubMed]
- Milési C, Essouri S, Pouyau R, et al. High flow nasal cannula (HFNC) versus nasal continuous positive airway pressure (nCPAP) for the initial respiratory management of acute viral bronchiolitis in young infants: a multicenter randomized controlled trial (TRAMONTANE study). Intensive Care Med 2017;43:209-16. [Crossref] [PubMed]
- Ramnarayan P, Lister P, Dominguez T, et al. FIRST-line support for Assistance in Breathing in Children (FIRST-ABC): a multicentre pilot randomised controlled trial of high-flow nasal cannula therapy versus continuous positive airway pressure in paediatric critical care. Crit Care 2018;22:144. [Crossref] [PubMed]
- Shi F, Chen M, Li Y. Application of high flow nasal catheter ventilation priority strategy in infants with severe bronchiolitis. Clinical Medicine 2021;41:11-3.
- Li J. Comparison of Application Value of High Flow Nasal Cannula and Nasal Continuous Positive Airway Pressure in Respiratory Support for Severe Bronchiolitis. Journal of Pediatric Pharmacy 2020;26:12-4.
- Li Y, Wei M, Cai Z. Application Effect of High Flow Oxygen Inhalation through Nasal Catheter in the Treatment of Children with Severe Bronchiolitis and Its Influence on Ventilation Function. Chinese and Foreign Medical Research 2021;19:18-20.
- Daverio M, Da Dalt L, Panozzo M, et al. A two-tiered high-flow nasal cannula approach to bronchiolitis was associated with low admission rate to intensive care and no adverse outcomes. Acta Paediatr 2019;108:2056-62. [Crossref] [PubMed]
- Lin Q, Bai Y, Li X, et al. Efficacy and Safety of High-Flow Nasal Cannula Oxygen Therapy in Children under Five Years Old: A Meta-Analysis. Nurs J Chin PLA 2021;38:10-5.




