
Kawasaki disease with pulmonary nodules: two case reports and literature review
Introduction
Kawasaki disease is an acute systemic vasculitis syndrome in children, mainly involving the small and medium blood vessels, and is often accompanied by damage to the nervous system, digestive system, muscles, joints, and urinary system (1,2). A diagnosis of complete Kawasaki disease can be established if the child presents with a fever for ≥4 days along with four of the five other principal clinical findings. A diagnosis of incomplete (sometimes referred to as atypical) Kawasaki disease should be considered for any infant or child with prolonged unexplained fever, fewer than four of the principal clinical findings, and compatible laboratory or echocardiographic findings (3). Coronary artery abnormalities are the most severe complication, which has been reported in 25% of patients with Kawasaki disease. Echocardiography is considered positive for purposes of this algorithm if any of three conditions are met: Z-score for the left anterior descending coronary artery or the right coronary artery of ≥2.5; a coronary artery aneurysm; or the existence of ≥3 other suggestive features, including decreased left ventricular function, mitral regurgitation, pericardial effusion, or Z-scores in the left anterior descending coronary artery or the right coronary artery of 2 to 2.5 (4). The revised guidelines recommend the use of Z-scores to define coronary artery dilation. If a Z-score for an internal coronary artery diameter is ≥2.5 standard deviation (SD) units, it is defined as a coronary artery dilation. However, if an examiner faces difficulties in using a Z-score, the conventional criteria for traditional measurements (i.e., an inner diameter ≥3 mm for children <5 years old, or ≥4 mm for children ≥5 years old) can be used for the diagnosis of coronary artery dilation (3).
Patients with severe coronary artery involvement may also develop aneurysms of other medium-sized arteries, including the axillary, subclavian, brachial, femoral, iliac, splanchnic, and mesenteric arteries (4). However, concomitant lung damage is rare and has only been observed in a small number of children with Kawasaki disease and incomplete Kawasaki disease. At present, lung damage remains a challenge in diagnosing and differential diagnosis of Kawasaki disease and incomplete Kawasaki disease (5-10).
This article retrospectively analyzed the clinical manifestations, laboratory examinations, imaging characteristics, diagnosis, treatment, and prognosis of two infants with Kawasaki disease complicated with multiple pulmonary nodules. A comprehensive review of the relevant literature was also undertaken.
We present the following case in accordance with the CARE reporting checklist (available at https://dx.doi.org/10.21037/tp-21-66).
Case presentations
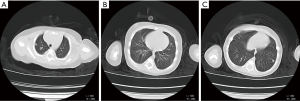
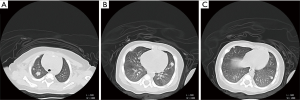
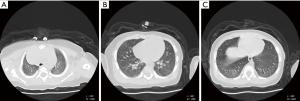
Patient 1, a previously healthy 83-day-old boy, presented with 10 days of cough and half a day of low-grade fever. At that time, his father had an upper respiratory tract infection. Initial laboratory studies revealed white blood cells (WBCs) of 13.95×109/L, a neutrophils percentage of 45.90%, a hemoglobin level of 103 g/L, platelets (PLTs) of 507×109/L, and C-reactive protein (CRP) of 33.98 mg/L. A chest computed tomography (CT) showed that the upper lobe of the patient’s bilateral lungs and the lower lobe of the left lung were nodular and patchy (see Figure 1A,B,C). The first impression was bronchopneumonia, and the initial treatment was piperacillin sodium (100 mg/kg/d) and erythromycin (15 mg/kg/d). The patient’s temperature was normal, and the cough stopped after 3 days. However, 1 week later, the laboratory tests revealed thrombocytosis (824×109/L), elevated WBCs (20.61×109/L) with neutrophil predominance, and elevated acute phase reactants, such as a CRP of 66 mg/L and an erythrocyte sedimentation rate (ESR) of 44.00 mm/h. During this period, the patient also had diarrhea. The results of cultures from his urine, blood, and stool were negative. Questions arose about his lung nodules, and we tested for the respiratory syncytial virus, adenovirus, influenza virus, Streptococcus pneumoniae, chlamydia, fungi, and other pathogenies to exclude the possibility of virus, tuberculosis, fungi, tumors, and so on. Due to the special period of the epidemic, we ruled out the possibility of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection. The SARS-CoV-2 viral nucleic acid detection and serum-specific antibody detection were also negative. As no clear pathogens were found, we stopped all antibiotics. Meanwhile, the patient was observed to have a mild, transient bilateral conjunctival redness. He had no skin rash, no lymphadenopathy, and his range of motion was normal for all joints. Additionally, a physical examination showed a clear chest, normal heart sounds, and a soft abdomen without hepatosplenomegaly. The results of his neurological examination were normal. A repeat chest CT revealed that the lung nodules had increased in number and were larger than before (see Figure 2A,B,C). Echocardiography revealed a fusiform right coronary artery (2.3 mm in diameter) (see Figure 3) and a mildly dilated left main coronary artery (4.0 mm in diameter) (see Figure 4). The patient’s diagnosis of Kawasaki disease was confirmed. He was immediately treated with intravenous immunoglobulin (IVIG) (2 g/kg/d) and aspirin (30 mg/kg/d). After 1 week, the patient’s WBCs, PLTs, and CRP were normal. He did not present with any periungual desquamation in the subacute phase. Echocardiography was taken of his right coronary artery (1.6 mm in diameter) (see Figure 5) and left main coronary artery (2.6 mm in diameter) (see Figure 6) 4 weeks later. After discharge, a follow-up appointment indicated that the lung nodules had disappeared some 2 months later (see Figure 7A,B,C).
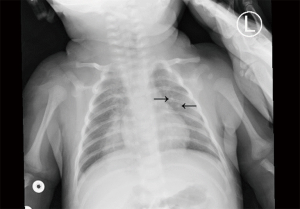
Patient 2, a 38-day-old boy, was admitted with a 2-day history of high fever and irritability. He had been physically healthy previously. He had no skin rash, no erythema, no cracking of the lips, no strawberry tongue, no erythema of oral or pharyngeal mucosa, no lymphadenopathy, no erythema and edema of the hands or feet, and/or periungual desquamation, and his range of motion was normal for all joints. A physical examination showed a clear chest, normal heart sounds, and a soft abdomen without hepatosplenomegaly. The results of the neurological examination were normal. A laboratory examination showed WBCs of 10.69×109/L, a neutrophils percentage of 35.30%, PLTs of 181×109/L, CRP of 11.49 mg/L, an ESR of 33 mm/h, and an alanine aminotransferase of 224.53 U/L. We also tested for a respiratory syncytial virus, adenovirus, influenza virus, Streptococcus pneumoniae, chlamydia, tuberculosis, fungi to exclude the possibility of infection. The SARS-CoV-2 viral nucleic acid detection and the serum-specific antibody detection were also negative. The patient’s cerebrospinal fluid was normal. The chest radiograph indicated left lung nodules (see Figure 8). There was no clinical response after 3 days of antibiotic treatment of ceftriaxone (80 mg/kg/d). The repeated laboratory data were significant for mild thrombocytosis (466×109/L), and the CRP was elevated (45.92 mg/L).
Due to the ineffective anti-infective treatment and the progressively elevated PLTs, we began to consider the possibility of incomplete Kawasaki disease. Echocardiography revealed a fusiform right coronary artery (1.8 mm in diameter) (see Figure 9) and a left fusiform coronary artery (2.5 mm in diameter) (see Figure 10). IVIG (2 g/kg) was administered along with aspirin (30 mg/kg/d). After treatment, the patient’s temperature quickly returned to normal. He did not present with any periungual desquamation in the subacute phase. As the lung symptoms were not obvious at the time, we did not perform a reexamination of the chest X-ray before he was discharged. A chest radiograph at a local hospital indicated that the lung nodules disappeared 1 month after being discharged. During the 3-month follow-up period, his coronary arteries also returned to normal (see Figures 11,12).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from both the patients’ parents.
Discussion
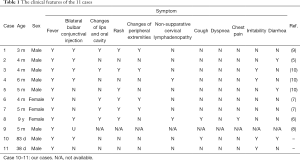
Pulmonary findings are not included in the classic diagnostic criteria for Kawasaki disease; however, chest radiograph abnormalities, including pulmonary nodules, have been observed in approximately 15% of patients, who may or may not have associated respiratory symptoms (11). In addition, pneumonia has been documented in 86% of autopsied acute stage Kawasaki disease cases (12). Pulmonary nodules are described as a sub-symptom in the American Heart Association scientific statement on the Kawasaki disease (4). Only 9 children have been reported to have pulmonary nodules associated with Kawasaki disease. We found that only 2 of 11 patients, including the 2 patients in this article, with Kawasaki disease complicated with pulmonary nodules, have had respiratory symptoms. The clinical features of the 11 cases are summarized in Table 1. Under the diagnostic guidelines for Kawasaki disease (6th revised edition), non-specific findings, such as respiratory symptoms (e.g., cough, rhinorrhea, and retropharyngeal edema), other irritability, abdominal pain, vomiting, diarrhea, and infiltrates on chest radiographs) maybe observed in Kawasaki disease and should not exclude a diagnosis (3).
Full table
A histological study of the nodules showed inflammatory cell infiltration surrounding several small and medium-sized arteries, as observed in coronary artery aneurysms in patients with Kawasaki disease (10). The pulmonary nodules of Kawasaki disease patients were inflammatory in nature, similar to the family of pseudo inflammatory tumors (IPTs). IPTs of the lung result from a benign reactive inflammatory process in which lymphocytes, plasma cells, and histiocytes infiltrate tissue, admixed with spindle-cell proliferation (13). Inflammatory pseudotumor formation is triggered by various stimuli, including infection, autoimmune illness, and trauma (14). In the previously reported cases, the lung nodules disappeared between 12 days and 1 year (5-10). The rapid involution of pulmonary nodules via standard Kawasaki disease treatment may reflect the inflammatory nature of the lesions.
Our cases illustrate that pulmonary nodules can be a feature of acute Kawasaki disease. Based on our findings and previous chest radiograph data, we speculate that pulmonary nodules may be present in acute Kawasaki disease complicated with coronary artery dilation (4-14). Thus, pulmonary nodules complicated with acute Kawasaki disease may enable the cautious observation of such lesions with serial CT scans for spontaneous resolution. Once a patient is diagnosed with Kawasaki disease and begins to show clinical improvement, follow-up CT scans will not be necessary. A biopsy should not be suggested unless the lesions do not show improvement after the acute Kawasaki disease has been treated.
Conclusions
In the 2 cases we reported, 1 of the patients presented with mild, transient bilateral conjunctival redness, and the other patient presented with a fever; thus, neither patient displayed all the typical symptoms of Kawasaki disease. Of the 9 cases previously reported, 7 (78%) presented with coronary artery involvement. The mean age of the children was 5 months (ranging from 3 months to 9 years), and 8 (89%) were infants [2–7]. We found that in these cases, not every patient had a typical manifestation of Kawasaki disease and that patients may only show 1 or 2 of the typical symptoms. However, atypical symptoms, such as a cough, irritability, and diarrhea, are more common. A high index of suspicion for the diagnosis of Kawasaki disease is particularly important in certain clinical situations. Prolonged fever or even no fever, irritability, and diarrhea may be important clinical manifestations of Kawasaki disease in infants.
Infants ≤6 months of age are the most likely patients to present without clinical symptoms for Kawasaki disease. Such infants are at particularly high risk of developing coronary artery abnormalities. In the treatment of the first patient, we were initially viewed that the patient’s irritability and loose stools complicated with thrombocytosis were manifestations of allergies. Similarly, in the treatment of the second patient, irritability and a culture-negative of cerebrospinal fluid suggestive of aseptic meningitis (treated meningitis) led to a diagnosis of Kawasaki disease being overlooked. Thus, in clinical work, if a child has a long fever that is unresponsive to anti-infective treatment or even no fever but unexplainable irritability and lung nodules, Kawasaki disease should be highly suspected.
In addition, it is important to note that pulmonary nodules are another clinical manifestation of Kawasaki disease. With the improvement of clinical manifestations after the regular treatment of Kawasaki disease, it is unnecessary to reexamine patients by undertaking a chest imaging examination, as these cases have shown that pulmonary nodules disappear, and there are no sequelae. A biopsy should not be suggested unless the lesions do not show improvement after the acute Kawasaki disease has been treated. However, future clinical studies need to explore further whether this kind of patient requires antibiotic treatment.
The parents of the patients expressed gratitude to us, and the treatments the patients received were timely and effective.
Acknowledgments
This paper has been edited by English Language Editors: L. Huleatt and J. Chapnick.
Funding: We acknowledge the support by Qingdao Municipal Hospital Clinical diagnosis and treatment Technology Innovation Fund Project (CXJJ-009).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://dx.doi.org/10.21037/tp-21-66
Peer Review File: Available at https://dx.doi.org/10.21037/tp-21-66
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/tp-21-66). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, including ensuring that any questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from both the patients’ parents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Orenstein JM, Shulman ST, Fox LM, et al. Three linked vasculopathic processes characterize Kawasaki disease: a light and transmission electron microscopic study. PLoS One 2012;7:e38998 [Crossref] [PubMed]
- Hoshino S, Tsuda E, Yamada O. Characteristics and fate of systemic artery aneurysm after Kawasaki disease. J Pediatr 2015;167:108-12.e1-2.
- Kobayashi T, Ayusawa M, Suzuki H, et al. Revision of diagnostic guidelines for Kawasaki disease (6th revised edition). Pediatr Int 2020;62:1135-8.
- McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 2017;135:e927-99. Erratum in: Circulation 2019;140:e181-4. [Crossref] [PubMed]
- Itani MH, Zakhour RG, Haddad MC, et al. Prolonged fever with pulmonary nodules in a 4-month-old baby. Pediatr Infect Dis J 2010;29:784, 788.
- Higuchi Y, Ochi M, Shimizu J, et al. A 9-year-old girl with Kawasaki disease and pulmonary nodules. Clin Rheumatol 2020;39:3139-40. [Crossref] [PubMed]
- Akagi K, Abe J, Tanaka K, et al. Kawasaki disease with pulmonary nodules and coronary artery involvement: a report of two cases and a review of the literature. Int J Rheum Dis 2017;20:1862-4. [Crossref] [PubMed]
- Monedero Picazo MD, Gómez Fernández-Montes J, Molina Fábrega R, et al. Radiologic findings in the lungs of patients with Kawasaki disease. Radiologia 2006;48:14-8. [Crossref] [PubMed]
- He T, Ling J, Chen J, et al. Intravenous immunoglobulin-resistant Kawasaki disease with multiple pulmonary nodules: a case report and literature review. J Clin Pediatr 2020;38:490-2.
- Freeman AF, Crawford SE, Finn LS, et al. Inflammatory pulmonary nodules in Kawasaki disease. Pediatr Pulmonol 2003;36:102-6. [Crossref] [PubMed]
- Gibbons RJ, Smith S, Antman E, et al. American College of Cardiology/American Heart Association clinical practice guidelines: Part I: where do they come from? Circulation 2003;107:2979-86. [Crossref] [PubMed]
- Gibbons RJ, Smith SC Jr, Antman E, et al. American College of Cardiology/American Heart Association clinical practice guidelines: Part II: evolutionary changes in a continuous quality improvement project. Circulation 2003;107:3101-7. [Crossref] [PubMed]
- Matsubara O, Tan-Liu NS, Kenney RM, et al. Inflammatory pseudotumors of the lung: progression from organizing pneumonia to fibrous histiocytoma or to plasma cell granuloma in 32 cases. Hum Pathol 1988;19:807-14. [Crossref] [PubMed]
- Freud E, Bilik R, Yaniv I, et al. Inflammatory pseudotumor in childhood. A diagnostic and therapeutic dilemma. Arch Surg 1991;126:653-5. [Crossref] [PubMed]










