Evaluation and management of knee pain in young athletes: overuse injuries of the knee
Introduction
Knee pain is a common concern for which young athletes are seen in a primary care or general practice setting. Acute macro trauma to the knee, especially in contact or collision sports is relatively less frequent and its management often requires consultation with orthopedic surgeon. On the other hand, overuse injuries affecting the knee account for the vast majority of knee pain. The underlying pathophysiology of an overuse musculoskeletal injury is repetitive and excessive stress to musculoskeletal structures. Multiple factors have been shown to contribute to overuse injuries. The factors shown to be relatively more consistently associated with overuse injuries are a sudden increase in the intensity, duration, and volume of physical activity; poor sport specific conditioning; insufficient sport-specific training; poor training techniques, and inappropriate equipment for the sport.
The intrinsic causes of knee pain are listed in Table 1 (1-7). In addition to the intrinsic causes, knee pain can be referred pain from the hip or lumbar spine pathology. Hip conditions to be considered include slipped capital femoral epiphysis, Legg-Calve-Perthes disease, and femoral neck stress fracture; whereas spine conditions to be considered include tumors of the spine or the cord, herniated disk, or spinal stenosis. Pain around the knee joint can also occur in osteosarcoma, Ewing sarcoma, synovial tumors, or osteoid osteoma. Systemic causes of knee pain include chronic juvenile arthritis, sickle cell arthropathy and leukemia. Our primary focus here is to provide a practical review of selected and significant overuse injuries seen in young athletes.

Full table
Idiopathic anterior knee pain
Idiopathic anterior knee pain, also described as patello-femoral pain syndrome, refers to non-specific, vague, mostly activity related anterior knee pain and is the most common cause of knee pain in adolescents (8-12). Gorman McNerney and Arendt state that idiopathic anterior knee pain affects around 30% of the adolescent population (13). Therefore, it is the most common cause of knee pain evaluated by primary care physicians, sport medicine physicians, and orthopedic surgeons. It is also more common in adolescent females, 2–10 times higher than their male counterparts (13).
Many factors have been postulated to contribute to the development of anterior knee pain in adolescents (Table 2) (8-13); primarily it is thought to be due to anatomical and biomechanical factors. Intense physical activity overloading the patellofemoral mechanism appears to be the most consistent factor leading to the development of anterior knee pain. The patellofemoral unit provides the mechanism for knee extension and deceleration (8). The stability of the patella in the femoral groove is provided by the surrounding soft tissue attachments and the bony supporting structures. Malalignment and abnormal tracking of the patella have been postulated to contribute to anterior knee pain (9). Vastus medialis obliquus plays an important role in stabilizing the patella in the femoral groove and its proper tracking (9).
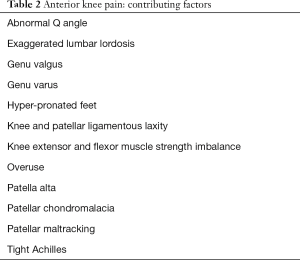
Full table
Clinical presentation
The young active athlete presents with either acute or gradual onset anterior knee pain affecting one or both knees usually seen following a recent increase in physical activity. The pain is increased after prolonged sitting (theater sign), ascending or descending stairs, and repeated squatting exercises. Usually the pain is present for few weeks with intermittent activity related exacerbations and improve with a period of rest. Deterioration of sports performance, because of increased frequency and worsening of the pain, often leads the athlete to seek medical attention. The athlete may give a history of the knee catching, pseudolocking or giving away (11).
On examination, look for abnormal gait, increased lumbar lordosis, and any asymmetry of hips or lower extremities; also, observe for atrophy and weakness of the quadriceps muscles by comparing it to the normal side. A decrease in flexibility of the hamstrings and quadriceps is a common finding (11). Isometric quadriceps contraction with the leg extended may reveal a subtle lateral patellar deviation. This can be assessed by placing a row of three dots in a straight line while the knee is relaxed (one several inches above the knee in the midline, one several inches below, and one at mid patellar point); then look for lateral displacement of the patellar dot on isometric quadriceps contraction. Knee effusion or soft tissue swelling is an uncommon finding. A full range of motion is maintained. In some athletes, tenderness may be elicited by palpating and exerting pressure on the articular margins of the patella while displacing it medially or laterally. A crepitus may be felt in some athletes. Pain is elicited with patellar inhibition or compression test (Figure 1).

Diagnostic imaging
Plain x-ray films may help rule out other conditions causing anterior knee pain such as osteochondritis dissecans of the patella or knee, or stress fracture of the patella. Radiographs are not indicated routinely. Abnormal tilt of the patella may indicate maltracking, best seen on a tangential view at 45 degrees of flexion of the knee (13).
Treatment
This is a benign, self-limited condition with gradual resolution over a period of few weeks; rarely in some athletes, it may take up to 2 years for complete resolution of symptoms (14,15).
Conservative treatment consists of relative rest with modification of activities, local ice, and a short-term use of anti-inflammatory medications to help control the pain. Complete rest and cessation of all activities are generally not necessary and the athlete should be allowed to continue all activities as tolerated. Prolonged sitting, squatting, climbing up or going downstairs, and full arc knee extension exercises should be avoided. Alternative activities such as cycling with a proper fit, swimming, and walking are encouraged as tolerated. The effectiveness of different kinds of taping techniques and knee braces varies considerably; their use should be individualized (15,16).
Rehabilitation exercises focus on increasing the flexibility, strength, endurance, and neuromuscular retraining of the quadriceps, hamstrings, gastrocnemius, and soleus muscles (14,15). Closed kinetic chain exercises are found to be most effective (14). Knee immobilization is not recommended, except in rare instances when pain is severe affecting daily activities. Rathleff et al. compared idiopathic anterior knee pain in adults and adolescents and the efficacy of exercise therapy in both populations (10). They concluded that despite having similar exercise therapies, the success rate for adolescents was much lower. They consider the cause to be a “cause-effect relationship” between strength and the onset of idiopathic anterior pain syndrome, suggesting that in adolescents reduced hip and knee strength is a consequence of anterior idiopathic pain (10). They proposed that neuromuscular control and coordination control added to strength training would have a clinical effect (10,14).
Osgood-Schlatter disease
Osgood-Schlatter disease is an overuse injury, a traction apophysitis, affecting the tibial tubercle apophysis. Osgood-Schlatter disease is commonly seen during Tanner stage 2 or 3 (1). It is more common in adolescent boys. The incidence is higher in athletes compared to non-athletes, 21% in athletes compared to 4.5% in non-athletes in one study (1,2,17).
Rapid growth and increased physical activity predisposes to the development of this condition during early adolescence. The immature patellar tendon-tibial tubercle junction is highly susceptible to submaximal, repetitive tensile stress resulting from high intensity sport activity (17). The underlying pathology is suggestive of minor avulsions at the site and subsequent inflammatory reaction.
Clinical presentation
Osgood-Schlatter disease is most commonly seen between 11-year and 13-year of age in girls and between 12-year and 15-year in boys (1,3,4). Adolescent presents with pain over the tibial tubercle just below the knee. The pain is bilateral in 20% to 30% of patients (1,17). The pain is aggravated by sports involving jumping, squatting, and kneeling, and is relieved by a period of rest. Localized tenderness and sometimes swelling over the tibial tubercle are noted on examination. Pain with resisted knee extension, tightness of the quadriceps and hamstrings or irregularities over the tibial tubercle may also be found during exam (7).
Diagnostic imaging
X-ray may show fragmentation of tibial tubercle and sometimes an ossicle in the patellar tendon (17).
Treatment
Treatment is conservative. Decreased activity and rest will result in significant improvement in pain. In some athletes, it is not uncommon for recurrent pain to last up to two years before complete resolution (1,17). Fortunately, most will not have symptoms after fusion of growth plates (5). Osgood-Schlatter disease is a benign, self-limited condition and over treatment should be avoided. The adolescent should be allowed to participate in all sports as tolerated. Hamstrings and quadriceps stretches should be done on a regular basis to improve and maintain flexibility. The most common complication is a persistent localized swelling, which may only be of cosmetic concern.
Ossicle formation in the patellar tendon may be a source of chronic pain in some athletes and removal of such an ossicle may be indicated. Presence of Osgood-Schlatter disease does not necessarily predispose the athlete for complete avulsion of the patellar tendon from the tibial tuberosity (2,6,17). This is only a potential concern during rapid growth phase just prior to fusion of the tubercle to tibia.
Sinding-Larsen-Johansson syndrome
This overuse injury affects the junction of the inferior pole of the patella and the insertion of the patellar tendon characterized by tendonitis, tendon avulsion and later localized calcification (1,3,4,18). The condition is most commonly seen in 10- to 13-year age group (18).
Repetitive traction at the inferior pole of the patella leads to Sinding-Larsen-Johansson syndrome (18). During early adolescence, the inferior pole of the patella is immature and chronic excessive traction leads to tendonitis, micro-avulsions at the proximal attachment of the patellar tendon, and de novo calcification and ossification at the junction of the inferior pole and patellar tendon (1,18).
Clinical presentation
The athlete presents with intermittent activity related anterior knee pain of gradual onset of several weeks or months duration. Pain is aggravated by jumping and running activities. It is localized over the inferior pole of the patella and proximal attachment of the patellar tendon. Usually there is no history of direct trauma to the area. On palpation, point tenderness is elicited at the patella-patellar tendon junction.
Diagnostic imaging
Calcification and ossification at the patella-patellar tendon junction is seen on plain films (18). This should be differentiated from a bipartite patella or a patellar sleeve fracture.
Treatment
This is a benign condition and results in no long-term complications. The athlete should be allowed participation in sports as tolerated. Because the pain is activity-related, some modification in activity level may be needed. In some cases, the recurrent pain may persist for 12 to 18 months before spontaneous resolution occurs (18). Because decreased flexibility of hamstrings is a common finding in many athletes, regular hamstrings stretches should be done. Acute painful episodes respond well to decreased activity, local ice massage, and short term use of NSAIDs. Local injection of corticosteroid into and around the patellar tendon is contraindicated, and may predispose to tendon weakness and rupture.
Juvenile osteochondritis dissecans (JOCD)
JOCD is significant cause of knee pain in adolescents, both athletes and the non-athletes. JOCD is characterized by delamination and localized necrosis of the subchondral bone, with or without the involvement of the overlying articular cartilage (19-24). Lateral aspect of the medial condyle of the femur is the most common site of JOCD, accounting for 75% of JODC lesions (19).
The exact etiology or mechanism leading to the JOCD lesion is not known. The term “osteochondritis” suggests an inflammatory etiology, however histology of the lesion had shown damage of bone and cartilage rather than inflammation (9). Repetitive microtrauma is considered to be a significant factor leading to JOCD. Local bone vascular insufficiency is also postulated to contribute to JOCD (20). The lesion of JOCD can be either closed or open; and either stable or unstable (23).
Clinical presentation
JOCD is four times more common in males than in females and the lesion is bilateral in 10–20% of the cases (19). The highly active athlete presents with a history of aching gradual onset of knee pain of several days to weeks’ duration typically located over anterior knee, worse during activity. There may be a history of intermittent knee swelling following a practice or game session.
Examination may or may not reveal mild effusion or limitation of motion of the knee. Findings may also vary depending on the stage of the disease (23). In early stages with the articular cartilage over the femoral condyle still intact, the signs are non-specific. In late stages when the articular cartilage is eroded, the fragment may separate and become an intra-articular loose body. This can cause pain, effusion, and locking. When the athlete flexes internally rotated leg, from full extension to about 30 degrees, pain is elicited, that is relieved upon external rotation (Wilson sign) (19,20). This is typical only for the lesion on the medial femoral condyle.
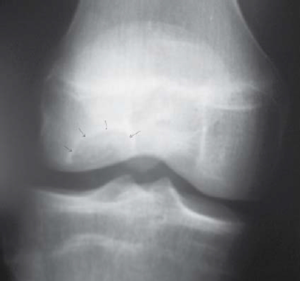
Diagnostic imaging
X-rays are indicated when JOCD is suspected. In addition to the AP and lateral views, a tunnel view is useful to see the lesion, which appears as a well demarcated radiolucent area (Figure 2) (20,21). Comparison with the other knee is important to avoid confusion with normal bone development (7). In those who demonstrate significant edema or hemarthrosis as well as marked discomfort and inability to bear weight without pain, an MRI is often obtained. An MRI can be helpful in identifying unstable lesions. However, it is important to note that MRI is less specific for identifying lesion stability in skeletally immature adolescents when compared to evaluating the same lesion in adults (7,22).
Treatment
Early diagnosis followed by restriction of activities, and symptomatic treatment of pain generally allows for healing of lesions over a period of 8–12 weeks (21,22,24). Spontaneous healing of the lesion is the usual outcome in children and adolescents with open distal femoral physis. Full sport participation can be resumed once the athlete is pain free and there is roentgenographic evidence of healed lesion. Prognosis is excellent in younger patients (24).
In more advanced cases when there is separation of the osteochondral fragment, knee immobilization may be needed (1,23). All such cases should be referred to an orthopedic surgeon as surgical intervention may be necessary for further management. Treatment is based on the stability of the lesion and the status of the overlying cartilage. In some cases, the lesion may be unstable or loose, and these cases as well as in those athletes with large effusions or with marked symptoms which don’t improve with conservative care may go to surgery for drilling, reattachment, or excision of the osteochondral lesion (1,22).
Bipartite or multipartite patella
Patella typically develops from a single ossification center. Sometimes it develops from 2 (bipartite) or more (multipartite) ossification centers and the segments are united by fibrous union (25,26). Acute or chronic repetitive trauma to the patella can result in painful bipartite or multipartite patella. Reported incidence of bipartite patella is between 0.2% and 6%, most are unilateral, and the male to female ratio is 9:1 (25-27).
The sites of fibrous union between segments of patella are subject of either acute or chronic injury resulting in pain. Acute direct blow to the patella can result in fracture through the junction between the segments of patella.
Most athletes with symptomatic bipartite or multipartite patella present with insidious onset of anterior knee pain aggravated by jumping, running, squatting or kneeling. There is localized patellar tenderness and mild swelling. In cases of patellar fracture there may be hemarthrosis, and restricted knee motion. X-ray of the patella is diagnostic and shows a linear regular radiolucent line.
Most athletes will respond to a 3 to 4 weeks of rest from activity (27). If conservative treatment fails, young athletes should be referred to an orthopedic surgeon for surgical interventions (25,27).
Plica syndrome
Embryologically the knee develops from three separate compartments, namely, medial, lateral and suprapatellar (28). Synovial plicae are believed to be the remnants of these synovial compartments. Suprapatellar, infrapatellar, medial (most common) and lateral plicae are normally found in the knee (28). Pain related to plica is related to the inflammation of the medial plica. The exact incidence and prevalence in adolescent athletes is not known.
Three types of mechanisms are related to symptomatic plica in young athletes, direct trauma to the medial aspect of the knee and patella, injury to the plica as it is entrapped between the medial patellar facet and the medial condyle, and overuse injuries with the knee in flexion and with repeated external rotation of the tibia (28,29).
Most plicae are asymptomatic. In symptomatic medial plica, the athlete will present with medial knee pain that is activity related. Pain may be present intermittently for weeks to months before the athlete is seen. There may be a history of feeling pop or snap during flexion of the knee. Athlete may also describe a sense of knee locking. On examination, there will be localized tenderness over the anteromedial aspect of the patella and there may be some soft tissue swelling. The plica may also be palpated in some patients as they flex and extend the knee.
The active knee extension test, in which the patient quickly extends the knee from 90-degree flexion as in a soccer kick will elicit pain with stretching of the plica (29,30). A flexion block test is also described in which the patient takes the knee from full extension into 30 to 60 degrees of flexion and the knee is stopped in that position, again stretching the plica (29,30). The pain is anterior and above the medial joint line.
Imaging is generally neither indicated nor useful. It is important to note the synovial plica are a normal finding if found during arthroscopy unless they are related to an abnormal physical exam.
Treatment of symptomatic plica is a short period of rest, non-steroidal antiinflammatory drugs (NSAIDs), and return to usual activities and sports in a period of a few weeks (28). Some plicae remain symptomatic and require excision at arthroscopy with a thorough examination of the knee and treatment of any associated chondral or meniscal injuries which are found (28).
Iliotibial band (ITB) friction syndrome
On the lateral aspect of the knee, the ITB passes over the lateral femoral condyle and is inserted into the Gerdy’s tubercle on the lateral aspect of proximal tibia just distal to knee joint line (3). ITB syndrome refers to overuse injury affecting the tendon as it passes over the lateral femoral condyle. It is the most common cause of lateral knee pain in runners (4-6). ITB syndrome has also been reported in cycling, tennis, skiing, football, soccer, and weightlifting (6).
With the knee in full extension the IT band lies anterior to the lateral femoral condyle and as the knee is flexed it passes over the femoral condyle at about 30 degree of flexion, and lies posterior to the femoral condyle with further flexion of the knee past 30 degrees (1). Repeated friction between the IT band and the lateral femoral condyle leads to chronic inflammation and activity related pain. Predisposing factors include overuse, IT band tightness, hamstring tightness, genu varum, internal tibial torsion, and hyper-pronated feet (6,7).
Clinical presentation
Athletes present with activity related lateral knee pain. Pain is characteristically felt only during the activity and there is no pain at rest either before or after the activity such as running. During running it is more intense during downhill running on banked surfaces (5). There is localized tenderness over the lateral femoral epicondyle about 3 cm proximal to the lateral knee joint line (7). Ober (Figure 3) and Noble tests (Figure 4) are helpful in clinical diagnosis (4-7).


Treatment
Most young athletes will respond very well with a short period of rest, modification of activity, local application of ice, and NSAIDs. A referral for physical therapy is indicated if there is no resolution with initial simple measures. Physical therapy will include assessment treatment for any predisposing biomechanical factors such as hamstring and IT band tightness as well as consideration for orthotics for hyper-pronated feet. Additionally, heat and electrical modalities may be used to control pain and inflammation. Very rarely surgery may be considered in chronic recalcitrant cases.
Quadriceps tendonitis
Quadriceps tendon strains and tendonitis, usually at the insertion of the quadriceps at the proximal pole of patella occur with chronic overuse and overloading in the jumping and running activities (5). The patient will present with pain and tenderness at the superior pole of the patella, sometimes weakness on resisted quadriceps extension. Treatment is rest, local ice application, NSAIDs, and quadriceps stretching.
Popliteus tendonitis
Popliteus muscle originates from the lateral femoral condyle and is inserted on the posterior tibia (1). The main functions of the popliteus muscle are to initiate and maintain the internal rotation of the tibia in relation to the femur, to assist the posterior cruciate ligament in preventing the posterior motion of the tibia in relation to the femur, and to derotate the knee at the initiation of the flexion (1,2). Popliteus tendonitis can result from overuse and the athlete presents with activity related lateral knee pain. Tenderness is localized on the lateral aspect of the knee and is best elicited with the patient sitting in figure of four position (Figure 5). Treatment is conservative with rest and pain management.
Acknowledgements
The authors thank Anna, Skye and Allison for their help with the manuscript preparation.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
Disclaimer: Parts of this article are adapted and updated from author’s previous work (Patel DR, Lyne ED. Overuse injuries of the knee, Patel et al. editors. Sports Medicine, McGraw Hill, 2009:330-41).
References
- Micheli LJ, Purcell L. editors. The Adolescent Athlete. A Practical Approach. New York: Springer Science, 2007:289-323.
- MacEwen GD. Tachdjian's Pediatric Orthopaedics. 3rd edition. Herring JA. editor. Philadelphia: W.B. Saunders, 2002.
- Wu M, Fallon R, Heyworth BE. Overuse injuries in the pediatric population. Sports Med Arthrosc 2016;24:150-8. [Crossref] [PubMed]
- Stein CJ, Micheli LJ. Overuse injuries in youth sports. Phys Sportsmed 2010;38:102-8. [Crossref] [PubMed]
- Seto CK, Statuta SM, Solari IL. Pediatric running injuries. Clin Sports Med 2010;29:499-511. [Crossref] [PubMed]
- Beck NA, Patel NM, Ganley TJ. The pediatric knee: current concepts in sports medicine. J Pediatr Orthop B 2014;23:59-66. [Crossref] [PubMed]
- Yen YM. Assessment and treatment of knee pain in the child and adolescent athlete. Pediatr Clin North Am 2014;61:1155-73. [Crossref] [PubMed]
- Dutton RA, Khadavi MJ, Fredericson M. Patellofemoral Pain. Phys Med Rehabil Clin N Am 2016;27:31-52. [Crossref] [PubMed]
- Rothermich MA, Glaviano NR, Li J, et al. Patellofemoral pain: epidemiology, pathophysiology, and treatment options. Clin Sports Med 2015;34:313-27. [Crossref] [PubMed]
- Rathleff MS, Vicenzino B, Middelkoop M, et al. Patellofemoral Pain in Adolescence and Adulthood: Same Same, but Different? Sports Med 2015;45:1489-95. [Crossref] [PubMed]
- Kodali P, Islam A, Andrish J. Anterior knee pain in the young athlete: diagnosis and treatment. Sports Med Arthrosc 2011;19:27-33. [Crossref] [PubMed]
- Barber Foss KD, Myer GD, Chen SS, et al. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train 2012;47:519-24. [Crossref] [PubMed]
- Mcnerney ML, Arendt EA. Anterior knee pain in the active and athletic adolescent. Curr Sports Med Rep 2013;12:404-10. [Crossref] [PubMed]
- Alba-Martín P, Gallego-Izquierdo T, Plaza-Manzano G, et al. Effectiveness of therapeutic physical exercise in the treatment of patellofemoral pain syndrome: a systematic review. J Phys Ther Sci 2015;27:2387-90. [Crossref] [PubMed]
- Barton CJ, Lack S, Hemmings S, et al. The 'Best Practice Guide to Conservative Management of Patellofemoral Pain': incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med 2015;49:923-34. [Crossref] [PubMed]
- Smith TO, Drew BT, Meek TH, et al. Knee orthoses for treating patellofemoral pain syndrome. Cochrane Database Syst Rev 2015.CD010513. [PubMed]
- Vaishya R, Azizi AT, Agarwal AK, et al. Apophysitis of the Tibial Tuberosity (Osgood-Schlatter Disease): A Review. Cureus 2016;8:e780. [PubMed]
- Valentino M, Quiligotti C, Ruggirello M. Sinding-Larsen-Johansson syndrome: a case report. J Ultrasound 2012;15:127-9. [Crossref] [PubMed]
- Peters TA, Mclean ID. Osteochondritis dissecans of the patellofemoral joint. Am J Sports Med 2000;28:63-7. [PubMed]
- Pascual-Garrido C, Moran CJ, Green DW, et al. Osteochondritis dissecans of the knee in children and adolescents. Curr Opin Pediatr 2013;25:46-51. [Crossref] [PubMed]
- Schulz JF, Chambers HG. Juvenile osteochondritis dissecans of the knee: current concepts in diagnosis and management. Instr Course Lect 2013;62:455-67. [PubMed]
- Kocher MS, Tucker R, Ganley TJ, et al. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med 2006;34:1181-91. [Crossref] [PubMed]
- Uppstrom TJ, Gausden EB, Green DW. Classification and assessment of juvenile osteochondritis dissecans knee lesions. Curr Opin Pediatr 2016;28:60-7. [Crossref] [PubMed]
- Yang JS, Bogunovic L, Wright RW. Nonoperative treatment of osteochondritis dissecans of the knee. Clin Sports Med 2014;33:295-304. [Crossref] [PubMed]
- Matic GT, Flanigan DC. Return to activity among athletes with a symptomatic bipartite patella: a systematic review. Knee 2015;22:280-5. [Crossref] [PubMed]
- Oohashi Y. Developmental anomaly of ossification type patella partita. Knee Surg Sports Traumatol Arthrosc 2015;23:1071-6. [Crossref] [PubMed]
- Mcmahon SE, Leroux JA, Smith TO, et al. The management of the painful bipartite patella: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:2798-805. [Crossref] [PubMed]
- Bellary SS, Lynch G, Housman B, et al. Medial plica syndrome: a review of the literature. Clin Anat 2012;25:423-8. [Crossref] [PubMed]
- Schindler OS. 'The Sneaky Plica' revisited: morphology, pathophysiology and treatment of synovial plicae of the knee. Knee Surg Sports Traumatol Arthrosc 2014;22:247-62. [Crossref] [PubMed]
- Stubbings N, Smith T. Diagnostic test accuracy of clinical and radiological assessments for medial patella plica syndrome: a systematic review and meta-analysis. Knee 2014;21:486-90. [Crossref] [PubMed]



