
Effect of hypertension on the long-term prognosis of children with primary focal segmental glomerulosclerosis-a retrospective cohort study
Highlight box
Key findings
• Hypertension was a risk factor for poor long-term prognosis in children with primary focal segmental glomerulosclerosis.
What is known and what is new?
• More than 50% of primary focal segmental glomerulosclerosis patients may have hypertension, which can further deteriorate the renal function.
• The incidence of end-stage renal disease was associated with hypertension.
What is the implication, and what should change now?
• For primary focal segmental glomerulosclerosis children with hypertension, blood pressure should be actively controlled to prevent the development of end-stage renal disease.
Introduction
Primary focal segmental glomerulosclerosis is a common clinicopathological syndrome that involves hematuria, albuminuria, edema, hypertension, and abnormal renal function, and lacks specificity. Acute renal failure and albuminuria are common complications (1,2). Spherical sclerosis occurs with the expansion and fusion of segmental sclerosis. At the same time, because of segmental sclerosis, the glomerular filtrate enters into the gap between the Baumann’s bursa and parietal epithelial cells, gradually peels off the glomerular pole, and then further peels off the epithelial cells and basement membrane of renal tubules. The lesion invades the downstream nephron along the renal tubules, resulting in focal tubular atrophy, renal interstitial fibrosis, and acute renal injury, which eventually lead to renal failure (3-5). About 50% of patients with primary focal segmental glomerulosclerosis can be accompanied by hypertension, which can further promote the development of end-stage renal disease. However, hypertension is a chronic disease, and some children have poor compliance and cannot control blood pressure well. Moreover, the effect of hypertension on the long-term prognosis of children with primary focal segmental glomerulosclerosis is still unclear. Studying the related factors of end-stage renal disease is helpful to prevent and treat end-stage renal disease. This study aimed to explore the impact of hypertension on the long-term prognosis of children with primary focal segmental glomerulosclerosis. We present the following article in accordance with the STARD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-649/rc).
Methods
General information
The data of 118 children with primary focal segmental glomerulosclerosis admitted to the Nursing Department of West China Second Hospital from January 2012 to January 2017 were retrospectively collected. The children were divided into a hypertension group (n=48) and a control group (n=70) according to whether they had hypertension, and were followed up for 5 years to compare the difference in prognosis between the two groups. The inclusion criteria were as follows: (I) primary focal segmental glomerulosclerosis diagnosed by renal biopsy; (II) aged 3–17 years; and (III) complete clinical medical records. The exclusion criteria were as follows: (I) lost to follow-up; (II) secondary infection; (III) malignant tumor; (IV) solitary kidney; (V) diabetes nephropathy, immunoglobulin A nephropathy, membranous nephropathy, lupus nephritis, purpura nephritis, and other nephropathies; (VI) secondary focal segmental glomerulosclerosis; and (VII) cases in which end-stage renal disease had been diagnosed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the Nursing Department of West China Second Hospital (No. 2022KY-0098), and the requirement for the patients’ written informed consent for this retrospective clinical study was waived.
Study variables
Clinicopathological features such as age at diagnosis, gender, systolic blood pressure, diastolic blood pressure, hematuria, albuminuria, edema, glomerular filtration rate, and biopsy pathological results were collected retrospectively. The renal biopsy pathological results included the classification of primary focal segmental glomerulosclerosis (non-specific type, apical type, collapsed type, cellular type, and periportal type) (6), the glomerulosclerotic ratio, the degree of tubulointerstitial disease, and the degree of foot process fusion (divided into extensive fusion and segmental fusion by 50%). According to the cumulative area of the cortical lesions, tubulointerstitial lesions were divided into mild disease (<25%), moderate disease (25–50%), and severe disease (>50%).
Treatment
All children were given hormone and/or immunosuppressive therapy. Also, children with hypertension were treated according to the Hypertension Guidelines for Children and Adolescents issued by the United States in 2017 (7).
Follow-up
The children were followed up for more than 5 years to observe the incidence of end-stage renal disease. Follow-up was carried out through outpatient visits and telephone interviews.
Definition
End-stage renal disease in children was defined as a glomerular filtration rate <15 mL/(min·1.73 m2) or necessary renal replacement therapy (dialysis ≥3 months or renal transplantation).
Statistical analysis
SPSS 26.0 software (IBM, USA, Chicago) was used for data analysis. All measurement data conformed to a normal distribution and were expressed as the mean ± standard deviation, and the differences between the two groups were analyzed using an independent sample t-test. All counting data were expressed as n (%), and the chi-square test was used to analyze the differences between the two groups. The receiver operating characteristic (ROC) curve was used to analyze the predictive value of systolic and diastolic blood pressure for the development of end-stage renal disease in children with primary focal segmental glomerulosclerosis. The Kaplan-Meier survival estimate was used to analyze the cumulative survival rate, and multivariate logistics regression analysis was applied to explore the risk factors of end-stage renal disease in children with primary focal segmental glomerulosclerosis. P<0.05 indicated that the difference was statistically significant.
Results
Comparison of the clinicopathological characteristics between the two groups
Compared with the control group, the proportion of patients with severe renal tubulointerstitial damage (18.75% vs. 5.71%, P=0.026) and the incidence of end-stage renal disease (33.33% vs. 5.71%, P<0.001) in the hypertension group were significantly higher (Table 1).
Table 1
| Variables | Hypertension group (n=48) | Control group (n=70) | t/χ2 value | P value |
|---|---|---|---|---|
| Age at diagnosis (Years) | 11.42±4.12 | 10.90±3.41 | 0.742 | 0.459 |
| Gender | 0.120 | 0.729 | ||
| Male | 11 (22.92%) | 18 (25.71%) | ||
| Female | 37 (77.08%) | 52 (74.29%) | ||
| Systolic blood pressure (mmHg) | 165.77±14.02 | 115.27±13.96 | 19.270 | <0.001 |
| Diastolic blood pressure (mmHg) | 99.58±14.56 | 72.21±8.74 | 12.744 | <0.001 |
| Hematuria | 25 (52.08%) | 34 (48.57%) | 0.140 | 0.708 |
| Albuminuria | 25 (52.08%) | 39 (55.71%) | 0.151 | 0.697 |
| Edema | 30 (62.50%) | 32 (45.71%) | 0.116 | 0.734 |
| Glomerular filtration rate [mL/(min·1.73 m2)] | 107.94±19.02 | 111.51±23.89 | 0.866 | 0.388 |
| Pathological type | 3.656 | 0.454 | ||
| Non-specific type | 16 (33.33%) | 23 (32.86%) | ||
| Apical type | 11 (22.92%) | 18 (25.71%) | ||
| Collapsed type | 10 (20.83%) | 7 (10.00%) | ||
| Cellular type | 5 (10.42%) | 13 (18.57%) | ||
| Periportal type | 6 (12.50%) | 9 (12.86%) | ||
| Proportion of glomerulosclerosis (%) | 11.08±4.00 | 11.41±4.95 | 0.385 | 0.701 |
| Degree of tubulointerstitial lesion | 4.936 | 0.026 | ||
| Mild and moderate | 39 (81.25%) | 66 (94.29%) | ||
| Severe | 9 (18.75%) | 4 (5.71%) | ||
| End-stage renal disease | 16 (33.33%) | 4 (5.71%) | 15.431 | <0.001 |
Data are presented as n (%) or mean ± standard deviation.
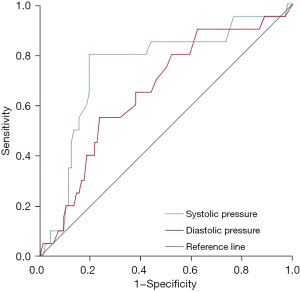
The predictive value of systolic blood pressure and diastolic blood pressure on the development of end-stage renal disease in children with primary focal segmental glomerulosclerosis
Systolic and diastolic blood pressure had a certain value in predicting the development of end-stage renal disease in children with primary focal segmental glomerulosclerosis (area under the curve: 0.752, 95% CI: 0.627–0.877, P<0.001; area under the curve: 0.659, 95% CI: 0.530–0.788, P=0.025), and the predictive value of systolic blood pressure was relatively higher (Table 2 and Figure 1).
Table 2
| Test result variable(s) | Area under the curve | P value | 95% CI | |
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Systolic blood pressure | 0.752 | <0.001 | 0.627 | 0.877 |
| Diastolic blood pressure | 0.659 | 0.025 | 0.530 | 0.788 |
Comparison of the incidence of end-stage renal disease in children
Compared with the control group, the cumulative incidence of end-stage renal disease in the hypertensive group was markedly higher (P<0.001) (Figure 2).
The risk factors of end-stage renal disease in children with primary focal segmental glomerulosclerosis
Multivariate logistic regression analysis showed that hypertension and severe renal tubulointerstitial disease were risk factors for end-stage renal disease in children with primary focal segmental glomerulosclerosis (P=0.009 and P<0.001, respectively) (Table 3).
Table 3
| Variables | B | SE | Wald | P value | Relative risk (95% CI) |
|---|---|---|---|---|---|
| Hypertension | 2.835 | 1.081 | 6.872 | 0.009 | 17.022 (2.045–141.723) |
| Severe renal tubulointerstitial disease | 5.628 | 1.398 | 16.211 | <0.001 | 278.091 (17.963–4,305.099) |
| Constant | −12.595 | 3.542 | 12.644 | <0.001 |
SE, standard error.
Discussion
Primary focal segmental glomerulosclerosis can occur at any age, but it is more common in children and adolescents. End-stage renal disease caused by primary focal segmental glomerulosclerosis has increased the burden on families and society. The prevention and treatment of end-stage renal disease are key to the treatment of primary focal segmental glomerulosclerosis. Therefore, we designed this study to identify the risk factors for the development of end-stage renal disease in primary focal segmental glomerulosclerosis children. The results showed that hypertension was a risk factor for the development of end-stage renal disease in primary focal segmental glomerulosclerosis patients.
The pathological characteristics of primary focal segmental glomerulosclerosis involves the focal distribution of the segmental sclerotic glomeruli, most of which have spherical sclerosis, accompanied by different degrees of podocyte proliferation, segmental endothelial cell and mesangial cell proliferation, renal tubular epithelial cell injury and focal atrophy, renal interstitial focal lymphocyte, monocyte infiltration, and fibrosis (8-10). When primary focal segmental glomerulosclerosis develops further, it can lead to renal insufficiency and hypertension. The mechanisms of primary focal segmental glomerulosclerosis causing hypertension mainly involve: (I) the activation of the renin-angiotensin system leads to the increase of renin-angiotensin secretion, resulting in hypertension (11-13); and (II) water and sodium retention due to renal insufficiency causes excessive blood volume, which leads to hypertension (14-16). Malignant hypertension can also promote glomerular filtration rate decline, atrophy of renal tubules, and renal interstitial fibrosis, leading to the development of end-stage renal disease and eventually forming a vicious circle (17).
Hypertension can also lead to secondary focal segmental glomerulosclerosis (18). A previous study showed that 41.00% of patients with primary focal segmental glomerulosclerosis were accompanied by hypertension, promoting the development of renal insufficiency (19), which is consistent with the results of this study. The present study showed that 40.68% (48/118) of children with primary focal segmental glomerulosclerosis had hypertension, which was related to the final development of end-stage renal disease. In addition, this study also showed that severe tubulointerstitial disease was a risk factor for end-stage renal disease in children with primary focal segmental glomerulosclerosis (P<0.001). Severe tubulointerstitial disease is a direct manifestation of the severity of primary focal segmental glomerulosclerosis. In patients with severe tubulointerstitial disease, more than 50% of tubulointerstitial lesions occurred and a large number of necrotic tissues were found in the tubulointerstitial. Patients with severe tubulointerstitial disease may eventually develops into end-stage renal disease.
Limitations
This study was a retrospective clinical study, and the number of cases was relatively insufficient.
Conclusions
Predicting the occurrence and development of different diseases has been a hot research topic in recent years, with scholars aiming to predict the prognosis of patients and guide treatment (20-24). The present study found that hypertension was a risk factor for poor long-term prognosis in children with primary focal segmental glomerulosclerosis. Therefore, for children with primary focal segmental glomerulosclerosis with hypertension, blood pressure should be actively controlled to prevent the development of end-stage renal disease in children.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-649/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-649/dss
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-649/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the Nursing Department of West China Second Hospital (No. 2022KY-0098), and the requirement for the patients’ written informed consent for this retrospective clinical study was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Patil SB, Vanikar AV, Gumber MR, et al. Churg-Strauss syndrome presenting with acute kidney injury in a case of primary focal segmental glomerulosclerosis. Int Urol Nephrol 2014;46:211-5. [Crossref] [PubMed]
- Huang J, Lin L, Xie J, et al. Glucocorticoids in the treatment of patients with primary focal segmental glomerulosclerosis and moderate proteinuria. Clin Exp Nephrol 2018;22:1315-23. [Crossref] [PubMed]
- Sinha R, Sarkar S, Mandal K, et al. Uptake of next-generation sequencing in children with end-stage renal disease secondary to focal segmental glomerulosclerosis and parental decision for kidney transplantation-Experience from a low resource setting: A Retrospective Cohort Study. Pediatr Transplant 2021;25:e13960. [Crossref] [PubMed]
- Forster BM, Nee R, Little DJ, et al. Focal Segmental Glomerulosclerosis, Risk Factors for End Stage Kidney Disease, and Response to Immunosuppression. Kidney360 2021;2:105-13. [Crossref] [PubMed]
- Saida K, Kamei K, Morisada N, et al. A novel truncating PAX2 mutation in a boy with renal coloboma syndrome with focal segmental glomerulosclerosis causing rapid progression to end-stage kidney disease. CEN Case Rep 2020;9:19-23. [Crossref] [PubMed]
- D'Agati VD, Fogo AB, Bruijn JA, et al. Pathologic classification of focal segmental glomerulosclerosis: a working proposal. Am J Kidney Dis 2004;43:368-82. [Crossref] [PubMed]
- Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017;140:e20171904.
- Lorbach SK, Hokamp JA, Quimby JM, et al. Clinicopathologic characteristics, pathology, and prognosis of 77 dogs with focal segmental glomerulosclerosis. J Vet Intern Med 2020;34:1948-56. [Crossref] [PubMed]
- Gheissari A. Focal segmental glomerulosclerosis and end-stage kidney disease in children. J Nephropharmacol 2015;4:61-2.
- Fogo AB, Lusco MA, Najafian B, et al. AJKD Atlas of Renal Pathology: Focal Segmental Glomerulosclerosis. Am J Kidney Dis 2015;66:e1-2. [Crossref] [PubMed]
- Solis-Jimenez F, Perez-Navarro LM, Cabrera-Barron R, et al. Effect of the combination of bumetanide plus chlorthalidone on hypertension and volume overload in patients with chronic kidney disease stage 4-5 KDIGO without renal replacement therapy: a double-blind randomized HEBE-CKD trial. BMC Nephrol 2022;23:316. [Crossref] [PubMed]
- Albertoni Borghese MF, Oronel LH, Ortiz MDC, et al. Hypertension and renal disease programming: focus on the early postnatal period. Clin Sci (Lond) 2022;136:1303-39. [Crossref] [PubMed]
- Balagobi B, Niroshan V, Brammah T, et al. Bilateral nephrectomy as a rescue therapy for refractory hypertension in an end stage renal disease patient: Brahmastra in hypertension management-A case report. Int J Surg Case Rep 2022;98:107566. [Crossref] [PubMed]
- Kwon S, Lee SR, Choi EK, et al. Hypertension control and end-stage renal disease in atrial fibrillation: a nationwide population-based cohort study. Clin Res Cardiol 2022;111:284-93. [Crossref] [PubMed]
- Kawamura S, Fujimoto K, Hayashi A, et al. Plasma and serum prorenin concentrations in diabetes, hypertension, and renal disease. Hypertens Res 2022;45:1977-85. [Crossref] [PubMed]
- Damianaki A, Polychronopoulou E, Wuerzner G, et al. New Aspects in the Management of Hypertension in Patients with Chronic Kidney Disease not on Renal Replacement Therapy. High Blood Press Cardiovasc Prev 2022;29:125-35. [Crossref] [PubMed]
- Kadiri S, Thomas JO. Focal segmental glomerulosclerosis in malignant hypertension. S Afr Med J 2002;92:303-5.
- Fukuda K, Shimizu A, Kaneko T, et al. A case of secondary focal segmental glomerulosclerosis associated with malignant hypertension. CEN Case Rep 2013;2:68-75. [Crossref] [PubMed]
- Ghali M, Aloui S, Letaief A, et al. A multicenter study on profile of hypertension in focal segmental glomerulosclerosis in Tunisia. Ann Cardiol Angeiol (Paris) 2015;64:187-91. [Crossref] [PubMed]
- Chen Y, Wang J, Zhang X, et al. Correlation between apparent diffusion coefficient and pathological characteristics of patients with invasive breast cancer. Ann Transl Med 2021;9:143. [Crossref] [PubMed]
- Qi A, Li Y, Yan S, et al. Effect of postoperative chemotherapy on blood glucose and lipid metabolism in patients with invasive breast cancer. Gland Surg 2021;10:1470-7. [Crossref] [PubMed]
- Qi A, Li Y, Sun H, et al. Incidence and risk factors of sexual dysfunction in young breast cancer survivors. Ann Palliat Med 2021;10:4428-34. [Crossref] [PubMed]
- He XC, Chen HY, Qiu Y, et al. Associations of iron status with breast cancer risk factors in adult women: Findings from National Health and Nutrition Examination Survey 2017-2018. J Trace Elem Med Biol 2021;68:126867. [Crossref] [PubMed]
- Teng D, Xia S, Hu S, et al. miR-887-3p Inhibits the Progression of Colorectal Cancer via Downregulating DNMT1 Expression and Regulating P53 Expression. Comput Intell Neurosci 2022;2022:7179733. [Crossref] [PubMed]
(English Language Editor: A. Kassem)



