Premature death of children aged 2 months to 5 years: the case of the Mother and Child Center of the Chantal Biya Foundation, Yaounde, Cameroon
Introduction
Between 1990 and 2013, the mortality of children below the age of 5 years decreased worldwide from 91/1,000 live births to 43/1,000 live births (1). On the contrary, in less developed regions, especially in sub-Saharan Africa, infant and childhood death remains at unacceptable levels. In fact, from 179 deaths per 1,000 live births in 1990, mortality went down just to 92 in 2013. In Cameroon, it dropped from 138/1,000 in 1990 to 88/1,000 in 2013 (1). At this rate, the sustainable development goal might not be achieved between now and 2030.
Certain strategies to this effect have been put in place to curb infant and childhood mortality rate, which include preventive measures and curative actions that consists the main childhood killer diseases (2,3). Very few of these patients do benefit from it since they seldom seek for healthcare services (4,5). That notwithstanding studies have shown that patients who died in hospital milieu died within 48 hours of their admission (6,7) and that a majority of these children were below the age of 5 years (7). The deaths were due to pathologies whose management might have been retarded due to errors of diagnosis and/or treatment (6). Although traditional medical treatment at home according to our findings delays patients’ arrival in the hospital, this isn’t the only cause of the poor evolution of patients in the hospital (7,8). In fact, in Tanzania, patients who died from malaria had first gone for modern treatment (9). The non recognition of danger signs constitutes another cause of delay arrival of the patients at modern healthcare provision services (6,10). In most countries South of the Sahara, statistics of global mortality, especially in children are rare to come across and are often not very reliable (11).
A good knowledge of the characteristics of patients who died soon after their admission into the hospital would be indispensible in the elaboration of appropriate interventions to cope with this challenge. The objective of our study was to describe the characteristics of children below the age of 5 years who died within 48 hours of their admission in our hospital.
Methods
Type of study
It was a retrospective descriptive study.
Contextual framework
Considering the site and situation, this study took place in mother and Child center (MCC/CBF): of the (Reception, Emergency room, Hospitalization wards as well as the archives.
The MCC/CBF is a Pediatric Hospital in Yaounde, the political capital of Cameroon, a city of nearly two and a half million inhabitants. This hospital which serves as a university teaching hospital, has a capacity of 260 beds. It is thus the largest pediatric hospital of Cameroon. It receives about 30,000 children a year and 9,000 are hospitalized. The medical staff has 15 pediatricians, 15 general practitioners and between 5–10 pediatric residents. This medical team is supported by a team of nearly 250 nurses. During the day, all patients routinely pass by the reception service that directs them according to the need either to outpatient service or emergency department. In the night, patients are sent directly to emergency department. Considering the relatively good quality and low treatment charges of this hospital, it receives people from various socioeconomic backgrounds.
As regard the period of study, it extended from the 1st of January 2008 to the 31st of December 2012.
Our study population involved solely patients from 2 months to 5 years of age who died within 48 hours of their admission into the hospital. Those who were victims of accidental trauma were excluded from the study.
Data collection procedure
The data used was collected from the registration books at the reception room, outpost and emergency consultations and also from patients’ files in the hospitalization units of the study site. They were sorted out and classified according to 3 age groups: those less than 2 months old, those from 2 months to 5 years old and those more than 5 years. From the clinical records of those aged 2 months to 5 years who died prematurely on arrival in hospital, we went further to look for information on the gender, age, address, date and time of admission, type of consultation, presenting complaint, duration of the illness, therapeutic itinerary, signs and symptoms upon admission, treatments administered, as well as the time of demise. Given the early nature of the demise before paraclinical workup could be done, the retained diagnoses were based on clinical presumptions of the pediatricians. Some patients’ files we came across had very little information, so only 373 patients’ files of the deceased children could be studied.
Ethical considerations
Our study obtained approval from the ethical committee of Université des Montagnes.
Statistical analyses
The data were entered into MS Excel and carried for analyses in the Epi Info software version 3.5.3. We expressed continuous variables in the form of median and interquartile range, while categorical data were expressed in the form of proportions.
The Chi-Square test was used to compare proportions and for P values <0.05, the difference between proportions was considered statistically significant.
Results
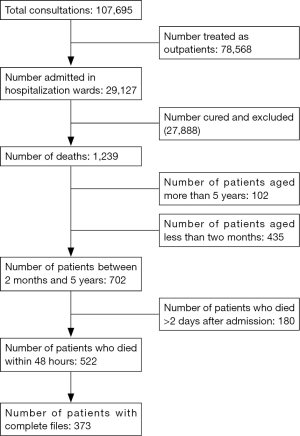
In 5 years, 107,695 children below the age of 16 had visited the MCC/CBF for a health consultation, 29,127 of whom were hospitalized. Out of a total number of 702 deaths recorded amongst patients aged between 2 months and 5 years, there were 522 early deaths within 48 hours of hospitalization (Figure 1). The incidence of deaths in the hospital was 4.9% of patients of the 2 months to 5 years age group (that is 702 deaths amongst the 14,200 patients of age 2 months to 5 years who were hospitalized).
Compared to all the admissions, the incidence of deaths specific to the 2 months to 5 years age range represented 2.4% of children (that is 702 deaths of children aged from 2 months to 5 years per 29,127 patients below the age of 16 who were hospitalized). As for early deaths the incidence was 3.7% of patients of the 2 months to 5 years age group (that is 522 deaths for 14,200 children in the considered age range). They constituted 74.27% (522/702) of total hospital mortality in children aged from 2 months to 5 years.
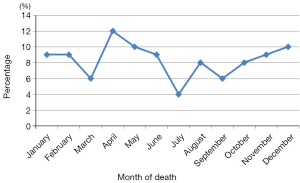
The incidence of deaths was high between March and May, then between October and December. The lowest values occurred in July (Figure 2).
General characteristics of children who died early
Age and gender
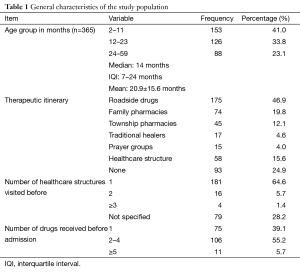
The population of children who died early was made of 205 boys (55%) and of 168 girls (45%), giving a sex ratio of 1.2. In 365 children whose ages were known, the median was 14 months, interquartile interval (IQI) 7–24 months, the mean age was 20.9 months with a standard deviation of 15.6 months. Close to 3/4 (74.8%) of patients were less than 2 years old, amongst whom 41% were aged between 2 and 12 months (Table 1). The house addresses of 123 (33%) patients wasn’t mentioned, meanwhile 224 (60%) were from Yaounde. Only 26 (7%) lived out of Yaounde.
Full table
Running to healthcare providers
The notion of self administered medication was noted in 313 patients files (Table 1). More than half (60.1%) of patients had taken such medication before being brought to healthcare service providers. They frequently took antipyretics (39.5%) alongside antimalarial drugs (19.3%). They had taken between 1 and 10 drugs with a mean of 2 drugs per patient.
Only 93 patients (24.9%) were brought to the study site without having received another form of treatment (other than hospital management). Other patients had been to at least one or more healthcare provider before coming to consult at the study site (Table 1).
Clinical characteristics of the deceased children
Time lapse between onset of illness and consultation at the MCC/CBF
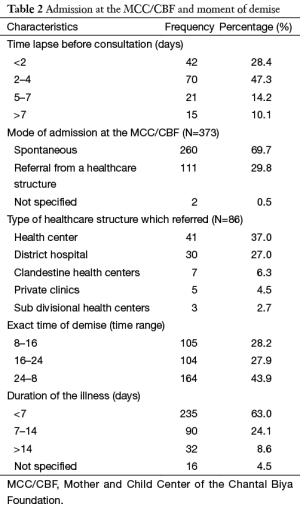
The time lapse between the onset of the illness and the initial medical attention was given for 148 patients. It varied from 0 to 30 days with a mean of 4 days. Most of the patients received initial medical attention between 2 and 4 days (Table 2).
Full table
The mode of admission at the MCC/CBF
The mode of admission was précised in 371 files. More than 3/4 of patients, 285 (76.8%) were brought there by their parents at freewill, whereas 86 (23.2%) were referred from another healthcare structure. The proportion of patients referred by first and second health facilities was 12.9% and 10.3% respectively (Table 2).
The presenting complaints/reason(s) for referral
For parents who freely chose to come and consult here, the presenting complaints were mostly Fever, in 167 (58.6%) patients, digestive disorders in 123 (43.2%), respiratory difficulty in 89 (31.2%) and convulsions in 71 (25%) patients. A patient could have more than one complaint. As for the 86 others, severe anemia was the main reason for referral, found in 32 (37.8%) patients, followed by neurological problems in 19 (22.1%), then respiratory distress in 13 (15.1), and severe dehydration (DH) in 12 (14%) patients.
Nutritional state
The weight of the children was the only anthropometric parameter found in the clinical records of the patients who died early stage of their treatment. The weight for age calculated in 172 children was less than −2 Z scores in 52 (30.23%) patients.
Duration of the illness
The mean total duration of the illness before demise was 8 days with extremes of 0 to 120 days. The majority of children, 235 (63%) died less than one week from the onset of the illness.
Moments of demise
The cumulative monthly average death rate during the study period showed a wide variety in course of the year. The periods between March and May and between November and January are the times globally with greater mortality (Figure 2). During nycthemeral a majority of the deaths occurred between midnight and 8 am (Table 2).
Causes of the deaths
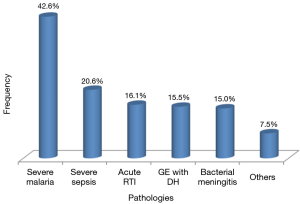
Severe malaria was the most encountered diagnosis (42.6%), followed by severe sepsis (20.6%) and acute lower respiratory tract infections (RTI) (16.1%) (Figure 3).
Discussion
The available data in the hospital registers and patients’ files enabled us to do an analysis of the epidemiology of the early deaths in our hospital.
Hospital mortality
For the age group we studied, we found an incidence of total hospital mortality of 4.9% and an early mortality of 3.7% of children hospitalized during the period of study. Miakoundoba and col at the University Teaching Hospital in Brazzaville in 2008 found a rate of 14.3% (12).
Djadou and col. in Togo reported in 2011 a mortality rate of 76.9% of children less than 5 years at CHR-TSEVI occurring within the first 48 hours (13). There exists a correlation between the infant and childhood mortality rate and the socio-economic level of a country. The countries where these studies were done are economically less advanced than Cameroon and have total infant and childhood mortality rates higher than that of Cameroon (1,14).
General characteristics of the study population
The majority of the registered deaths occurred mainly in children less than two years old. The most represented age range here was 2 to 12 months. Globally, the probability of death of a child is inversely proportional to his/her age. This is likewise in Cameroon, where the mortality rate of children below the age of 5 represents 2/3 of its total infant mortality (1). A study of mortality according to the sex shows that generally in most countries in the world (except in some Asian countries like India and china) the infant mortality is higher among male children than in females (15). The sex ratio was 1.12 in Cameroon in 2000. The difference in gender mortality noticed in our study will be simply in line with this tendency.
Mode of admission
About 3/4 of the deceased children were brought in spontaneously by their parents for consultation. Here in context, the notion of a family doctor exists only for a minority of an economically favored population. So to say for a population of about 22 million inhabitants Cameroon can hardly count 2,500 medical doctors in all sectors, amongst whom there are just about a hundred pediatricians (16). It is therefore difficult in this condition to have a reliable family doctor policy. In Switzerland for instance, with a population 3 times less than that of Cameroon, there exists a network of family doctors which counts more than 5,500 medical doctors and pediatricians outside public doctors (17). In our context, the way people perceive sickness varies. Sometimes this may depend on the sociocultural environment, at times on the level of education of the head of the family and or on the economic background (18).
Presenting complaints/reasons for referral
The most figuring complaints were fever, digestive disorders, and respiratory difficulty. These were the symptoms related to the main causes of death in children below the age of 5 years which are acute lower RTIs, diarrhea, malaria, measles, HIV/AIDS (19). After consultation in other healthcare some of these patients were referred here mainly because of severe anemia, respiratory distress and or neurological disorders.
Moments of demise
We noted during our study that a majority of deaths occurred between midnight and 8 am. A period which corresponds to the period when medical personnel is least prone to carry out certain interventions, especially resuscitating children. To this effect, it is worthwhile to think that insufficient human resources could be sidelight as major problem in most healthcare structures. As a matter of fact, one or maximum two nurses take on night duty as opposed to 3 to 4 who does the same job during the day.
Moreover, only two general practitioners cover night duty calls as against fifteen or more during the day, who often are accompanied by more than ten pediatricians. In Togo, Azumah and col registered 66.73% of deaths during night duty calls (7). It is possible that certain patients who died at such hours could have been rescued if they have had access to the same level of medical attention and expertise available during the day.
Furthermore, in case of need of certain specific therapies, patients have to move from one pharmacy on call to another with the probability of not finding in stock the prescribed drug.
The high death rates were recorded between March and June and between October and January a period corresponding to that of high amount of rainfall in Yaounde where our study site is found. These two seasons are characterized by high rates of transmission of malaria (20). Other authors have shown the link between these seasons and the level of anemia due to malaria (21,22).
Clinical characteristics of the deceased children
In most cases, the first medical attention the patients received came averagely 4 days after the beginning of the illness, and death occurred averagely 8 days later. Here again two types of problems are brought to light: the parents ignorant and underestimating the gravity of the illness didn’t react promptly, or they simply didn’t have the means to take care of the illness. More so, 2/3 of the deceased children had first sought at least one other method of treatment (such as automedication, traditional medicine) before coming to our study site where they died within 48 hours of arrival.
Most of the self-administered drugs came from street vendors. It has been shown that besides the problem of forgery, these drugs are conserved in very poor conditions and constitute a crucial problem to public health (23,24). Effort to manage the treatment in different places might have been ineffective and the person in charge might not have referred the patient to the hospital in time. All these delays could have been avoided if the parents could have had a good knowledge of appreciation of the gravity of their child’s illness and if this was followed by a formal healthcare service (25).
Nutritional state
The nutritional state of the patient was found to be poor in a third of them. Malnutrition is infact the root cause of morbidity and mortality with regard to a majority of childhood killer diseases in children below the age of 5 years in regions with limited resources (19). To this effect, programs to fight against the different infant and childhood diseases might not yield fruits if a good and effective program to curb malnutrition is not put in place.
Causes the deaths
Many diseases are responsible for the deaths of children amongst which are malaria, meningitis, RTIs, neonatal infections and severe malnutrition (7). Malaria has revealed itself as the main cause of death in our series. This mortality tendency can be explained by the incidence of malaria. Since 2010, Cameroonian authorities have intensified the fight against malaria.
The fight against the vector has been reinforced by the intensification of the distribution of insecticide treated mosquito nets all over the national territory. In addition, the treatment of simple malaria by Artemisinin Combined Therapy is free as well as that of severe malaria in children below the age of 5 all over the nation. These measures will greatly decrease the incidence of this pathology and consequently the deaths associated to it as shown in Eritrea and Zanzibar (26,27).
Preventive measures against these diseases still need to be reinforced. A more aggressive population sensitization campaign on the benefits of using insecticide treated bed nets (freely distributed to them) is necessary in order to reduce the incidence of malaria which is the major cause of death in our study location. In fact, it has been proven that most people take but don’t use these mosquito nets (28). The treatment of simple malaria in children less than 5 years is officially free of charge in Cameroon. If these measures could be effective in our context, a greater proportion of this population could have probably been out of risk from getting to the stage of lethal severe malaria.
Also, prompt arrival in the hospital for prompt and effective treatment of these children need to be encouraged, the hospital staff and structures on their own part need to instill confidence on the population by their hard work and successes. Our work illustrates that the vast majority of parents go for self administered medication with molecules of uncertain quality, and arrive the hospital very late. Sepsis, acute lower RTIs, gastroenteritis (GE) and meningitis were the other main causes of death in our research.
There could be a high probability initially trivial illnesses, get complicated as days go further without appropriate treatment. The reinforcement of Integrated Management of Childhood Diseases (IMCD) and more particularly of community IMCD will help to limit these situations.
Limitations
We did not collect information on all deaths that occurred during our study period. Our point of interest was focused only on early deaths in children aged 2 months to 5 years. So, we have certainly left out some information that could have permitted us to better discuss our results.
Conclusions
This study shows that for deaths which occurred within 48 hours of admission in children aged from 2 months to 5 years, the age group of less than a year was by far the most represented. These deaths were mostly due to evitable causes and courses, with malaria at the apex. The reinforcement of preventive measures and programs targeting children’s health such as the IMCD would be a main priority in the formulation of solutions to this phenomenon.
Acknowledgements
We are grateful to all the staff of Mother and Child Center, Chantal Biya Foundation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Levels and Trends in Child Mortality. Available online: http://www.unicef.org/media/files/Levels_and_Trends_in_Child_Mortality_2014.pdf
- Christopher JB, Le May A, Lewin S, et al. Thirty years after Alma-Ata: a systematic review of the impact of community health workers delivering curative interventions against malaria, pneumonia and diarrhoea on child mortality and morbidity in sub-Saharan Africa. Hum Resour Health 2011;9:27. [PubMed]
- Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year? Lancet 2003;362:65-71. [PubMed]
- Commeyras C, Ndo JR, Merabet O, et al. Comportement de recours aux soins et aux médicaments au Cameroun. Cah Sante 2005;16:5-12.
- Koffi AK, Libite PR, Moluh S, et al. Social autopsy study identifies determinants of neonatal mortality in Doume, Nguelemendouka and Abong-Mbang health districts, Eastern Region of Cameroon. J Glob Health 2015;5:010413. [PubMed]
- Källander K, Hildenwall H, Waiswa P, et al. Delayed care seeking for fatal pneumonia in children aged under five years in Uganda: a case-series study. Bull World Health Organ 2008;86:332-8. [PubMed]
- Azoumah KD, Balaka B, Matey K, et al. Mortalite hospitaliere a «l'hopital d'enfants de yendoube» de dapaong au Togo. Médecine d'Afrique noire 2007;54:5-8.
- Hill Z, Kendall C, Arthur P, et al. Recognizing childhood illnesses and their traditional explanations: exploring options for care-seeking interventions in the context of the IMCI strategy in rural Ghana. Trop Med Int Health 2003;8:668-76. [PubMed]
- de Savigny D, Mayombana C, Mwageni E, et al. Care-seeking patterns for fatal malaria in Tanzania. Malar J 2004;3:27. [PubMed]
- Terra de Souza AC, Peterson KE, Andrade FM, et al. Circumstances of post-neonatal deaths in Ceara, Northeast Brazil: mothers' health care-seeking behaviors during their infants' fatal illness. Soc Sci Med 2000;51:1675-93. [PubMed]
- World Health Organization. Statistiques Sanitaires Mondiales 2009. Available online: http://www.who.int/gho/publications/world_health_statistics/FR_WHS09_Full.pdf
- Miakoundoba RC, Mabiala Babela JR, Senga P. Morbidity and mortality of children aged 1 to 4 years in the University Teaching Hospital, Brazzaville (Congo). Available online: http://www.santetropicale.com/club/pdf/0508/5505_09.pdf
- Azoumah KD. Mortalite hospitaliere des enfants ages moins de 5 ans au chr-tsevie (togo), de 2007 A 2011. Available online: https://www.researchgate.net/publication/281237091_MORTALITE_HOSPITALIERE_DES_ENFANTS_AGES_MOINS_DE_5_ANS_AU_CHR-TSEVIE_TOGO_DE_2007_A_2011
- Mortality rate, infant (per 1,000 live births). Available online: https://www.researchgate.net/publication/281237091_MORTAhttp://data.worldbank.org/indicator/sp.dyn.imrt.inLITE_HOSPITALIERE_DES_ENFANTS_AGES_MOINS_DE_5_ANS_AU_CHR-TSEVIE_TOGO_DE_2007_A_2011
- Sex Differentials Childhood Mortality. Available online: http://www.un.org/esa/population/publications/SexDifChildMort/SexDifferentialsChildhoodMortality.pdf
- National Observatory of Human Resources for health in Cameroon. Available online: http://cm-minsante-drh.com/site/images/stories/Rapport_general_du_recensement01_12_2011_misenforme_FINAL05122001.pdf
- Actu. Bulletin des medecins de famille et de L'enfance suisse. Available online: http://www.medecinsdefamille.ch/fileadmin/user_upload/hausaerzteschweiz/Standpunkte/Standpunkte-1_15_f_web.pdf
- Coulibaly I, Keita B, Kuepie M. Les déterminants du recours thérapeutique au Mali: entre facteurs socioculturels, économiques et d’accessibilité géographique. Actes des colloques de l'AIDELF 2008:223-40.
- World Health Organization. Serious childhood problems in countries with limited resources. Available online: http://apps.who.int/iris/bitstream/10665/42923/1/9241562692.pdf?ua=1
- Nguefack F, Chelo D, Tejiokem MC, et al. Frequency of severe anemia in children aged 2 months to 15 years at Mother and Child Centre of the Chantal Biya Foundation Yaounde, Cameroon. Pan Afr Med J 2012;12:46. [PubMed]
- Okiro EA, Hay SI, Gikandi PW, et al. The decline in paediatric malaria admissions on the coast of Kenya. Malar J 2007;6:151. [PubMed]
- Mockenhaupt FP, Ehrhardt S, Eggelte TA, et al. Plasmodium falciparum multiplicity correlates with anaemia in symptomatic malaria. Trop Med Int Health 2003;8:857-9. [PubMed]
- Les médicaments de la rue en Afrique. Available online: http://news.doccheck.com/fr/blog/post/882-les-medicaments-de-la-rue-en-afrique/
- Les médicaments de la rue en Afrique: A qui profite le crime? Available online: http://convict.seneweb.com/les-medicaments-de-la-rue-en-afrique-a-qui-profite-le-crime_b_6.html
- Dongre AR, Deshmukh PR, Garg BS. Perceptions and health care seeking about newborn danger signs among mothers in rural Wardha. Indian J Pediatr 2008;75:325-9. [PubMed]
- Nyarango PM, Gebremeskel T, Mebrahtu G, et al. A steep decline of malaria morbidity and mortality trends in Eritrea between 2000 and 2004: the effect of combination of control methods. Malar J 2006;5:33. [PubMed]
- Bhattarai A, Ali AS, Kachur SP, et al. Impact of artemisinin-based combination therapy and insecticide-treated nets on malaria burden in Zanzibar. PLoS Med 2007;4:e309. [PubMed]
- Libite PR, Kelodjoue S, Dzossa AD, et al. Republic of Cameroon: Demographic and Health Survey and Multiple Indicator Cluster Survey (DHS-MICS) 2011. Available online: http://www.cabdirect.org/abstracts/20133374469.html