
Application of vocal organ correction combined with language training in the rehabilitation of children with cerebral palsy and language disorder
Introduction
Cerebral palsy (CP), a common neurological disease in children, refers to a syndrome resulting from various non-progressive injuries during brain development within 1 month after birth. CP is a lifelong condition that can be extremely harmful for the patient’s health. The main clinical manifestations of CP are abnormal posture and motor disorders (1). The causes of CP are diverse and multi-factorial, including congenital, hereditary, inflammatory, infectious, hypoxia, traumatic and metabolic (2). With an incidence of approximately 80%, language disorder is a common complication among patients with CP (3). Bilateral adrenal cortex and oral motor dysfunction are the main causes of language disorders in patients with CP. The lack of language acceptance and expression skills is very common and is closely related to mental retardation (4).
At present, there are more and more researches on language disorders in children with CP. A population-based study examining 84 children with CP showed participants were impaired across linguistic subdomains indicating a generalized language deficit, and co-occurring receptive and expressive language impairment was common (5). Choi et al. collected the brain MRI and language assessment reports of 172 children with CP between 3 and 7 years of age and found that both receptive and expressive language development quotients (DQs) were significantly related to PVWL or deep gray matter lesion severity (6). The clinical treatment of language disorder caused by CP is extremely challenging. Language disorders are mostly due to the corresponding neurological dysfunction caused by brain injury, and clinical treatment is extremely difficult. Microcurrent reflexotherapy combined with cortexin was used in the complex treatment of speech disorders in patients with CP (7). In China, acupuncture has proved to be effective in improving language impairment in children with CP (8). It has also been reported that vitamin D assisted rehabilitation therapy is effective in the language function and language development of children with CP and language disorder (9). Language training is a common rehabilitation program for patients with CP with language disorder. It mainly includes articulation training, pronunciation training, vocabulary training, and short sentence training. The aim of the training is to improve the patient’s language function, but it takes a long time for the training to have an effect. Therefore, patients and their families often give up the training, which affects the clinical efficacy. Furthermore, for some patients with severe language disorders, this method alone has unsatisfactory efficacy (10,11). Vocal organ correction, which is a common adjuvant treatment for children with language disorders, can reduce the difficulty and improve the clinical efficacy of language training (12). In this randomized controlled trial, the efficacy of vocal organ correction combined with language training for the rehabilitation of children with CP and language disorder was explored. We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/tp-20-223).
Methods
Clinical data
The study subjects were 98 children with CP and language disorder who were treated in our hospital between January 2015 and March 2018. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Tong De Hospital of Zhejiang Province (2014 Scientific Research Quick Review No. 065). Signed informed consent was obtained from each patient. All of the children met the screening criteria for inclusion. The patients were equally divided by random number table into the control group and the test group. The study subjects included 50 males and 48 females, aged 1–7 years (average age: 3.10±0.52 years). The types of language disorder were articulation disorder (70 cases) and language development delay (28 cases). The Gesell language development quotient (DQ) scores ranged from 35–60 (average score: 46.72±6.83). As shown in Table 1, no significant differences were observed in gender, average age, type of language disorder, or Gesell language DQ between the two groups (all P>0.05).
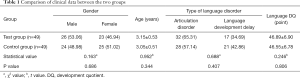
Full table
Screening criteria
To be included, children needed to meet the diagnostic criteria of CP (13), and met the diagnostic criteria of language impairment in children through language development survey (14). Informed consent from the child’s parents/guardians was also a requirement for participation.
The exclusion criteria were as follows: congenital vocal organ hypoplasia with comorbidities of congenital hypoplasia or disorder in other parts of the body; a previous history of craniocerebral trauma; other types of comorbidity, such as heart failure; or difficulty for a child or their family to cooperate to complete this study.
Study methods
The children in the control group were given language training, which was as follows:
- Articulation training:
- Respiratory training: the children were guided and helped to control their respiratory airflow by blowing trumpets, balloons, windmills, and other devices. The devices ranged from small to large, and from simple to difficult. The children performed these activities twice a day, for 10 minutes each time.
- Tongue training: the children performed a variety of tongue exercises, mainly including sticking the tongue out and putting it back, rolling it back, lifting it to lick the palate, and moving it bilaterally. Under the care of professional doctors, the children practiced tongue flexibility by licking a lollipop, and this was combined with tongue exercises. The children performed these exercises twice a day, for 10 minutes each time.
- Sucking training: the children were encouraged to suck liquid from a cup using a thick, short straw, which was eventually replaced with a thin, long straw to increase the difficulty. This was carried out twice a day, for 10 minutes each time.
- Pronunciation training:
- Bilabial “p”, “b”, and “m” sounds: the children were told to carefully watch the physician’s mouth movements and patterns, and then asked to repeat the sound. This training was carried out twice a day, for 10 minutes each time.
- Velar “k” and“g” sounds: the children were instructed not to touch their palate with their tongue. Those with greater difficulty to control this kind of touch were placed in the supine position with their legs flexed to the chest, and the professional physicians used a tongue depressor to limit their tongue movement and encouraged them to to practice their pronunciation through audio-visual skills. This training was carried out twice a day, for 10 minutes each time.
- Dental and linguodental sounds, including “i”, “d”, and “n”. The children were placed in the prone position with their limbs relaxed and extended. The professional physician lifted the child’s head and flexed it forward slightly. The physician encouraged the children to imitate their pronunciation. This training was carried out twice a day, for 10 minutes each time.
- Vocabulary training:
- Two-word vocabulary training: initially, the simplest and most commonly used reduplicated words were used for training, such as “baba (dad)”, “ma ma (mom),” “ye ye (grandpa)”, and “nainai (grandma)”. The words gradually increased in difficulty, with transition to the words commonly used in daily life. This training was carried out twice a day, for 10 minutes each time;
- Three-word vocabulary training: the children trained with words such as “liang tang tang (bright)”, “xiao bao bao (baby)”, and “xiaojiahuo (little boy/girl)”. This training was carried out twice a day, for 10 minutes each time.
- Multiple-word vocabulary training: the children trained with words such as “gaogaoxingxing (happy)”, “kai kaixinxin (happy)”, and “kuaikuai le le (happy)”. This training was carried out twice a day, for 10 minutes each time.
- Short sentence training: the children were guided to perform training with short sentences such as “bao bao chi fan (Time to eat, baby)” and “bao baozhen bang (You are so great, baby)”. The sentences were gradually lengthened to increase the difficulty. This training was carried out twice a day, for 10 minutes each time. Short sentence training lasted for 3 months.
The articulation training lasted for 3 months.
Vocabulary training lasted for 3 months.
The children in the test group were given language training along with vocal organ correction. The training was focused on correcting the following vocal organs, according to the results of vocal organ disorder assessment. The details of training are as follows:
- Oral lip dyskinesia:
- Upper lip muscle correction: first, Renzhong (GV26) was pressed with the thumb pulp, kneaded gently (20 times), point-pressed (5 times), and massaged (3–5 times). Then, Dicang (ST4) was pressed 5 times.
- Lower lip muscle correction: the thumb pulp was used point, press, knead, rub, grasp, and push on the lower lip muscle for 2–3 min. Then, Lianquan (CV23) was point-pressed 5 times, and the upper and lower lip muscles were pinched gently for passive motion.
- Tongue dyskinesia: the children were asked to stretch out and draw back the tongue. If the children had difficulty stretching their tongue fully, the tip of the tongue was covered with gauze and pulled outwards. If the tongue could be stretched laterally, resistance was applied with a tongue depressor to enhance the motor ability of tongue muscles. If the tongue could not be stretched laterally, a cotton rod was used for passive stimulation, and the tongue muscles were tapped at the root to relax them. The tongue was pressed and kneaded for 5–10 minutes daily.
- Mandibular dyskinesia: Ermen (TE21) was massaged for several seconds, the root of ear and the muscles outside the tragus were kneaded up and down, and Yifeng (TE17) was point-pressed. After the tension in the muscles had been relieved, Ermen (TE21) was point-pressed with the thumb, and the mandible was moved up and down using the other four fingers. Jiache (ST6) was point-pressed 7–8 times a day.
- Soft palate dyskinesia:
- Oral-nasal separation treatment: the children were placed in the supine position. They were instructed to close their mouth and breathe through their nose. The nose was then pinched to cause the children to breathe through the mouth. If a child had difficulty understanding the breathing instructions, the physician gave a demonstration, or gently pinched the child’s lips to force them to breathe through the nose, and then pinched their noses to force them to breathe through the mouth. The children alternated between breathing through the nose and mouth for 2–3 minutes.
- Velopharyngeal closure treatment: the children sucked the straw with one end of it blocked. The straw was inserted into a cup and the child was told to breathe in or inserted into warm water and the child was told to blow. If the child did not cooperate, passive training could be given to guide the child to puff out their cheek.
- Respiratory dyskinesia: the children were placed in the supine position, and instructed to take a deep breath and hold it. The professional physician put pressure with the appropriate speed and strength on their chest and abdomen, so that the child passively, and for as long as possible, made the “a, a” sound. The children were given deep breath and blowing training. Qiangyin, Hongyin, Dazhui (GV14), and Tiantu (CV22) were point-pressed. The children underwent 1 year of treatment in total.
Observation indicators
- Changes in language function classification before and after treatment were assessed using the Chinese Rehabilitation Research Center (CRRC) sign-significate (S-S) relations examination method. Stage 1: difficultly understanding objects and events. Stage 2: a basic understanding of objects, including functional operation (2-1), matching (2-2), and selection (2-3). Stage 3: symbols of objects, including gesture symbols (3-1) and speech symbols (3-2). Stage 4: words, sentences, and main sentence components, including two-word sentences (4-1) and three-word sentences (4-2). Stage 5: grammatical rules, including word order (5-1) and the passive voice (5-2).
- Clinical efficacy. Marked effect: if the language function classification of the patient had improved by ≥2 grades after treatment. Effective: if the language function classification of the patient had improved by one grade after treatment. No effect: if the patient showed no improvement in language function classification after treatment. Total effective rate = marked effective rate + effective rate.
- Family satisfaction. An anonymous satisfaction survey was carried out among the main carers of the children in the two groups. Respondents were asked if they were very satisfied, satisfied, or not satisfied with the training. Total satisfied rate = very satisfied rate + satisfied rate.
Statistical analysis
SPSS 26.0 software (IBMCorp. Armonk, USA) was used for all statistical analysis. Normally distributed measurement data were described as mean ± standard deviation (SD) and were analyzed using t-tests. Enumeration data were described as percentage, and classification distribution data were analyzed by rank-sum test. The enumeration data between the two groups were analyzed by chi-squared test. P<0.05 was considered to be statistically significant.
Results
Changes of language function classification before and after treatment
As shown in Table 2, there was a significant difference in language function classification between the two groups before and after treatment (P<0.05). After treatment, a significant difference was found in language function classification between the two groups (P<0.05).
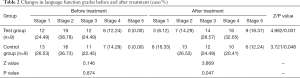
Full table
Clinical efficacy
As shown in Table 3, there was a significant difference in the distribution of clinical efficacy between the two groups (P<0.05), and the total effective rate in the test group was higher than that in the control group (P<0.05).
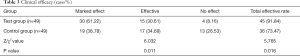
Full table
Family satisfaction
The difference in the distribution of family satisfaction between the two groups was statistically significant (P<0.05), and the total satisfaction rate of families in the test group was higher than that in the control group (P<0.05). See Table 4.
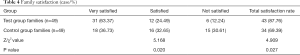
Full table
Discussion
Language communication disorder, language symbol disorder, and language expression disorder are more severe in children with CP and language disorder. The language level of such children is obviously low, making it difficult for them to communicate normally and effectively with others, which inflicts great harm on their physical and mental health (15). Improving the language ability of children with CP and language disorder during rehabilitation is important for their quality of life, as well as for the development of their physical and mental health (16), and can also reduce the mental burden on their families. Language training includes articulation training, pronunciation training, vocabulary training, and short-sentence training. The difficulty of training can be gradually increased to improve a child’s language function. However, due to the young age of children during language training, it is difficult for professional physicians to operate, and the results for some children are unsatisfactory. Therefore, there is still significant room for improvement with this program. Clinicians should focus on how to effectively enhance the language function and efficacy of children with CP with language disorder.
This study showed that after treatment, the language function classification was significantly improved in the test group and the control group compared with that before treatment. After treatment, the language function classification in the test group was significantly better than that in the control group. The distribution of clinical efficacy in the test group was also significantly better than that in the control group. The total effective rate of the test group (91.84%) was significantly higher than that of the control group (71.47%). These results indicate that vocal organ correction combined with language training in rehabilitation treatment for children with CP and language disorder can significantly improve language function, with significant clinical efficacy. Vocal organ correction included targeted corrective measures such as oral lip dyskinesia, tongue dyskinesia, mandibular dyskinesia, soft palate dyskinesia, and respiratory dyskinesia. Each targeted training significantly improves the function of the related vocal organs, especially motor function, and also enhances flexibility. The correction therefore improves the effect of pronunciation training and enhances the efficacy of language training. Compared with language training alone, vocal organ correction combined with language training has significant efficacy, and the language function classification and overall rehabilitation efficacy of children with CP and language disorder are improved (17,18). In a study of 128 children with CP and language disorder, Taub (19) showed that among different age groups and different language disorders, vocal organ correction combined with articulation training can achieve good efficacy. The language disorder of children with cerebral palsy are complex, and dysarthria is the main manifestation of language barriers (20), including dysphonia, resonance, and language development delay. In this study on vocal organ correction and articulation training, vocabulary training and short-sentence training were also combined, to better improve language function and clinical efficacy. It has certain effects on children with different types of language disorders. Our findings showed that the combination of vocal organ correction and language training could synergistically enhance the language function of children with CP and language disorder.
Furthermore, the distribution of family satisfaction in the test group was significantly better than that in the control group. The total satisfaction rate for the test group was 87.76%, significantly higher than the 69.39% for the control group. There are a number of reasons for this. First, the combination of the vocal organ correction and language training has a better effect on the improvement of the language function, with satisfactory rehabilitation results. Also, vocal organ correction requires professional physicians to help the children to complete the tasks with patience and a gentle attitude. This increases the opportunities for communication between the physician and the children and their families, and thus effectively brings a closer doctor–patient relationship.
In summary, vocal organ correction combined with language training should be used in the rehabilitation of children with CP and language impairment. This combination not only effectively improves the language function of such children, but also obtains the optimal effect, with high satisfaction among children's families, making it superior to language training alone. However, this study still has limitations: (I) the clinical sample of children with cerebral palsy included in this article is small. This requires communication and negotiation with similar clinical hospitals to join this study. At the same time, we also need to communicate and cooperate patiently with family members to obtain more clinical samples. (II) During rehabilitation, children's language environment at home, training compliance, and other factors can affect the clinical efficacy of treatment, which may have led to some deviation in the results. How to create a good home language environment and enhance training compliance should be directions and goals in future research.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/tp-20-223
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tp-20-223
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-20-223). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Tong De Hospital of Zhejiang Province (2014 Scientific Research Quick Review No. 065). Signed informed consent was obtained from each patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cristian A, Giammarino C, Olds M, et al. Safety considerations for patients with communication disorders in rehabilitation medicine settings. Phys Med Rehabil Clin N Am 2012;23:343-7. [Crossref] [PubMed]
- Upadhyay J, Tiwari N, Ansari MN. Cerebral Palsy: Etiology, Pathophysiology and Therapeutic Interventions. Clin Exp Pharmacol Physiol 2020. [Crossref] [PubMed]
- Mou Z, Teng W, Ouyang H, et al. Quantitative analysis of vowel production in cerebral palsy children with dysarthria. J Clin Neurosci 2019;66:77-82. [Crossref] [PubMed]
- Sankar C, Mundkur N. Cerebral palsy-definition, classification, etiology and early diagnosis. Indian J Pediatr 2005;72:865-8. [Crossref] [PubMed]
- Mei C, Reilly S, Reddihough D, et al. Language outcomes of children with cerebral palsy aged 5 years and 6 years: a population-based study. Dev Med Child Neurol 2016;58:605-11. [Crossref] [PubMed]
- Choi JY, Choi YS, Park ES. Language Development and Brain Magnetic Resonance Imaging Characteristics in Preschool Children With Cerebral Palsy. J Speech Lang Hear Res 2017;60:1330-8. [Crossref] [PubMed]
- Ukhanova TA, Gorbunov FE, Ivanova VV. Reflexotherapy combined with cortexin in the complex treatment of speech disorders in patients with cerebral palsy. Zh Nevrol Psikhiatr Im S S Korsakova 2011;111:19-22. [PubMed]
- Zhang QM, Jin R. Zhongguo Zhen Jiu 2005;25:699-701. [Clinical observation on children with language disorder of cerebral palsy treated by acupuncture]. [PubMed]
- Zhu X, Jiao R, Tu M, et al. The effect of vitamin D auxiliary rehabilitation therapy in children with cerebral palsy and language dysfunction. Minerva Pediatr 2019;71:495-9. [Crossref] [PubMed]
- Lin JP, Kaminska M, Perides S, et al. Bilateral globus pallidus internus deep brain stimulation for dyskinetic cerebral palsy supports success of cochlear implantation in a 5-year old ex-24 week preterm twin with absent cerebellar hemispheres. Eur J Paediatr Neurol 2017;21:202-13. [Crossref] [PubMed]
- Pennington L, Stamp E, Smith J, et al. Internet delivery of intensive speech and language therapy for children with cerebral palsy: a pilot randomised controlled trial. BMJ Open 2019;9:e024233. [Crossref] [PubMed]
- Collier B, Blackstone SW, Taylor A. Communication access to businesses and organizations for people with complex communication needs. Augment Altern Commun 2012;28:205-18. [Crossref] [PubMed]
- Novak I, Morgan C, Adde L, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr 2017;171:897-907. [Crossref] [PubMed]
- Rescorla L, Alley A. Validation of the language development survey (LDS): a parent report tool for identifying language delay in toddlers. J Speech Lang Hear Res 2001;44:434-45. [Crossref] [PubMed]
- Watson RM, Pennington L. Assessment and management of the communication difficulties of children with cerebral palsy: a UK survey of SLT practice. Int J Lang Commun Disord 2015;50:241-59. [Crossref] [PubMed]
- Horridge KA, Harvey C, McGarry K, et al. Quantifying multifaceted needs captured at the point of care. Development of a Disabilities Terminology Set and Disabilities Complexity Scale. Dev Med Child Neurol 2016;58:570-80. [Crossref] [PubMed]
- Kim SW, Kim JY, Lee SY, et al. The Comparison of M-B CDI-K Short Form and K-ASQ as Screening Test for Language Development. Ann Rehabil Med 2016;40:1108-13. [Crossref] [PubMed]
- Silva PF, Quintino LF, Franco J, et al. Measurement properties and feasibility of clinical tests to assess sit-to-stand/stand-to-sit tasks in subjects with neurological disease: a systematic review. Braz J Phys Ther 2014;18:99-110. [Crossref] [PubMed]
- Taub E. The behavior-analytic origins of constraint-induced movement therapy: an example of behavioral neurorehabilitation. Behav Anal 2012;35:155-78. [Crossref] [PubMed]
- Mou Z, Teng W, Ouyang H, et al. Quantitative analysis of vowel production in cerebral palsy children with dysarthria. J Clin Neurosci 2019;66:77-82. [Crossref] [PubMed]
(English Language Editor: J. Reynolds)


