
Collaboration and new data in ACTION: a learning health care system to improve pediatric heart failure and ventricular assist device outcomes
Introduction
Current challenges in pediatric heart failure and ventricular assist devices (VADs)
Pediatric heart failure is a significant, burdensome and complex condition associated with high morbidity and mortality. The estimated incidence of heart failure is 0.9–7.4 per 100,000 children (1). Each year in the United States, tens of thousands of children are admitted for heart failure with an in-hospital mortality of 7% (2,3). In children with congenital heart disease admitted with severe heart failure requiring at least intravenous inotropes, in-hospital mortality climbs to 26% (4). For the sickest children on the waiting list for a heart transplant, 22% will die before a donor organ becomes available (5).
A growing number of VADs are now being used to support children with severe, refractory heart failure which has improved waiting list survival (6,7). Nevertheless, outcomes remain suboptimal, especially for smaller children. In younger patients requiring a paracorporeal VAD, for example, 30% will experience a stroke and mortality is 2–3× higher compared with older patients supported with implantable VADs (8). Current resource utilization for children with advanced heart failure requiring a VAD is extremely high; median length of stay is 81 days and median hospital costs are $750,000 (9).
Managing heart failure and VADs in children is a particularly vexing challenge due to a combination of factors including: the increasing complexity and heterogeneity in children presenting with heart failure, limited number of patients managed at any given center and paucity of pediatric-specific evidence to guide clinicians sifting through an ever-growing number of diagnostic and therapeutic possibilities. Not unexpectedly, data show that experience matters; higher rates of adverse events, resource utilization and mortality are inversely related to center volume (9-11).
The need for a learning health system
The Institute of Medicine summarized the status quo in health care:
“But the pace of change is too slow, and adoption is too spotty; the system is not evolving quickly enough. The system needs to learn more rapidly, digest what does and does not work, and spread that knowledge in ways that can be broadly adapted and adopted (Figure 1) (12).”

These shortfalls are accentuated in the field of pediatric heart failure and VADs since no single center has a sufficient number of patients to achieve mastery and produce generalizable knowledge on their own. Despite considerable advancements, outcomes for children with heart failure remain suboptimal. Members of the community have realized that unless there is an overhaul of the traditional system of siloed practice, outcomes for most children will not improve. The urgent need to establish a learning health care system for our field has become abundantly clear.
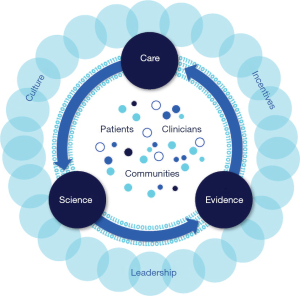
A “learning health care system” can be defined as one in which “science and informatics, patient-clinician partnerships, incentives, and culture are aligned to promote and enable continuous and real-time improvement in both the effectiveness and efficiency of care (Figure 2) (12).” A learning health care system continuously generates and collects new data, efficiently gains and disseminates new knowledge, and improves practice. A learning health care system is inclusive of diverse stakeholders.
ACTION: Advanced Cardiac Therapies Improving Outcomes Network
Employing a learning health care system model, ACTION was formed in April 2017 (www.actionlearningnetwork.org). ACTION’s mission is to improve critical outcomes for children and adult congenital heart disease patients with heart failure by developing an international collaborative learning health system that unites all key stakeholders (patients, families, clinicians, researchers and industry).
ACTION has been closely modeled after successful pediatric network-based learning health care systems that have facilitated collaboration and improved health outcomes at scale (13). Key elements to their success have been emphasized in ACTION including: focusing on goals and outcomes that matter most to participants, utilizing rigorous quality improvement methodology to assess impact, embracing transparency and creating an infrastructure that facilitates connectivity and sharing. ACTION’s philosophy can be summarized by two mottos: “steal shamelessly, share seamlessly” and “all teach, all learn” [both of which have been “stolen,” without shame, from other networks (13)]. Through this network-based learning health system, the dissemination and adoption of best practices and evaluation of outcomes has occurred at a much faster pace than in the traditional scientific model.
In contrast to a traditional hierarchical organization, ACTION has a flexible structure comprised of many empowered and self-directed leaders and committees working on separate but interrelated initiatives aligned with the common goal. In 2 years, ACTION has grown to include nearly 40 different centers internationally and a diverse community of patients and families, clinicians, researchers, industry partners and regulatory bodies actively collaborating and sharing ideas and data to improve pediatric heart failure outcomes. Initiatives highlighting ACTION’s collaboration and data will be discussed below.
Collaboration in ACTION
Network-wide quality improvement initiatives
At the onset, ACTION participants came together, discussed potential goals and unanimously agreed that decreasing the high risk of stroke should be the top priority. Utilizing quality improvement methodology, ACTION participants identified three potential key drivers of stroke and targets for improvement: anticoagulation, blood pressure and communication. Baseline network stroke data was collected. After much discussion and generous sharing of best practices and experience, novel anticoagulation, blood pressure monitoring and communication protocols were created and tested. In December 2018, three new protocols were officially launched together as “The Initial ABCs of Stroke Prevention: Quality Improvement Bundle.” As a testament to the participants’ commitment to collaboration, over 30 centers agreed to change their practice and follow the new protocols, and thus far, implementation has been nearly universal. In the near future, we will be able to determine whether or not these interventions have had their desired effect.
Currently only 55% of children with “dischargeable” VADs are being discharged to home (8). Continuing to focus on goals that matter most to patients and families, ACTION members are working on an initiative to safely discharge more children on VADs across the network by identifying important barriers and creating and implementing new processes. ACTION is engaging at least one patient or parent from each center to participate in this initiative.
VADs can be intimidating and overwhelming to patients, families and providers alike. There are very limited educational resources available that are designed specifically for the pediatric population. Many VAD caretakers are inadequately informed and trained. ACTION is partnering with design experts and graphic artists to create pediatric-specific materials (infographics, learning modules, videos, and even virtual reality games; Figure 3) to educate patients, families and providers about VADs in children and how to care for them. These resources will be freely accessible to all ACTION participants.

Practice standardization
Standardization in health care can potentially reduce unnecessary variability, improve quality and efficiency, decrease risk, and enable providers to more easily learn from each other’s experiences. With standardization, the efficacy of new care practices can be better assessed (14).
Given the complexity and limited number of pediatric heart failure and VAD patients, ACTION believes that standardization of practice is necessary to more quickly gain generalizable knowledge and improve outcomes in this field overall.
In addition to the standardized quality improvement initiatives mentioned above, ACTION has created standardized guidelines for addressing common pediatric VAD scenarios through multi-center sharing and discussion of best practices, experience and available evidence. These “harmonization” documents offer standardized approaches to issues such as pre-implant evaluation, thrombosis, driveline care, imaging, stroke, right heart failure and compassionate deactivation.
The next major phase of ACTION will focus on pediatric heart failure. To start, ACTION is working collaboratively to standardize definition, classification and documentation of heart failure in children across centers. This will allow us to better characterize and understand the problem and target areas for improvement.
Centralization and resource sharing
ACTION provides the necessary improvement infrastructure, resources, experience and expertise to carry out projects and improve outcomes that most centers would not have on their own. ACTION has chosen to centralize all legal and regulatory processes (i.e., institutional review board, data use agreement) and data coordination. Although the upfront effort is significant, ACTION believes long-term maintenance and compliance will be simpler and less onerous for each individual center.
Building an online community
Successful learning health care systems utilize a virtual repository, or a “commons” to readily share resources and experiences (13). ACTION has adopted a commercially-available team management app (Basecamp, basecamp.com) for this purpose. This simple app provides a platform for storing documents and files, schedules, to-do lists and real-time communication. Through the app’s message boards and chat features, ACTION members freely post questions and answers, troubleshoot, share ideas and learn from each other to improve care. The lively and generous engagement through this app is proof of how ACTION members have fully adopted the philosophies of “steal shamelessly, share seamlessly” and “all teach, all learn.” This platform has effectively brought the community closer together.
Collaboration outside of ACTION
ACTION is committed to active collaboration not only within its network but outside of it as well. ACTION is a founding and committed member of Cardiac Networks United, a new integrated research and improvement “network of networks” which aims “to foster novel and impactful science across the lifespan that would not otherwise be possible without such collaborative efforts, accelerate the translation of discovery to improvements in clinical care, and support greater efficiency through sharing resources in pediatric and congenital heart disease (15).” ACTION is also partnering with important, existing registries and databases including Society of Thoracic Surgeons - Pedimacs/Intermacs, Pediatric Heart Transplant Society, and United Network for Organ Sharing. Together they are devising ways to streamline data entry, link and share data, and collaborate on joint research and quality improvement projects.
Data in ACTION
Quality improvement focus
A learning health care system continuously collects and analyzes data to improve care. Unlike traditional registries, ACTION’s data collection is primarily focused on rapid quality improvement not the traditional research model. Quality improvement data is typically more narrowly focused, has fewer measures and is collected as close to real-time as possible. Currently, the registry is collecting data on all pediatric and congenital patients with VADs throughout the network. Data entry has been designed by stakeholders and streamlined for efficiency. Data collection is focused on the quality improvement project at hand, initially stroke in VADs. Data forms are intended to be flexible and nimble and expected to change as ACTION’s priorities shift in the future.
Real-world data sharing with industry and regulatory bodies
First approved in December 2011, the Berlin Heart EXCOR is still the only VAD approved by the FDA for use in children despite widespread use of other VADs. One of ACTION’s major goals is to promote more pediatric-specific labeling and support for devices and therapies used in heart failure. Industry and regulatory bodies are important and valued partners in ACTION and resources are actively shared between these groups. ACTION is committed to openly sharing “real-world” data and evidence to achieve this goal.
Simply defined, real-world data consists of data from a variety of potential sources that are routinely generated or collected in the course of health care delivery. Historically, monitoring of safety has been conducted through a limited, passive system of medical device reporting of adverse events which is subject to incomplete and biased data (16). To improve post market surveillance of the Berlin Heart EXCOR, ACTION is collecting and sharing high quality, real-world data with Berlin Heart, other industry partners and the FDA.
For rare conditions such as pediatric heart failure when a randomized control study may not be feasible, real-world data can be used across a wide spectrum of research in both observational and interventional studies to more efficiently generate evidence of effect (17). ACTION is contributing this real-world evidence so that commonly used VADs can obtain pediatric-specific regulatory approval and support. ACTION seeks to be a vital platform for future device and drug trials for pediatric advanced heart failure. ACTION also plans to expand and integrate other real-world data sources, from its current registry and quality improvement data collection to include patient-reported outcomes, smart devices, social media and larger socioeconomic databases.
Real-world data is an evolving concept for all partners; therefore, it will require innovative solutions. ACTION is fully committed to the highest quality of data using processes that are being developed in collaboration with FDA, other regulatory authorities and industry partners.
Data accessibility and transparency
ACTION desires to make its data accessible and useable to the entire community. ACTION is creating real-time, interactive center-specific and ACTION-wide VAD reports and dashboards that can be readily accessed. As ACTION’s collective experience grows, this dashboard will be used to instantaneously display specific outcomes based on patient characteristics (age, size, diagnosis, clinical status) and device type. This will become a powerful tool for decision-making and anticipatory guidance for clinicians and families. The dashboard will facilitate benchmarking and target specific areas for improvement. Through this tool and other avenues, ACTION seeks to promote informed decision-making and transparency between clinicians, centers, researchers, families and patients.
Conclusions
Considerable improvement can be made in the care of children with significant heart failure. ACTION was formed because community members believe that working together is the best and fastest way to improve and advance the field. The network-based learning health care system model provides the best framework for fostering active collaboration and learning.
Acknowledgments
None.
Footnote
Conflicts of Interest: ACTION receives funding from Medtronic, Abbott, Berlin Heart, Children’s Heart Association of Cincinnati, Cincinnati Children’s Innovation Fund and other individual philanthropic donors. A Lorts is a consultant for Abbott, Berlin Heart, and SynCardia and has an educational grant from Medtronic. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Shaddy RE, George AT, Jaecklin T, et al. Systematic Literature Review on the Incidence and Prevalence of Heart Failure in Children and Adolescents. Pediatr Cardiol 2018;39:415-36. [Crossref] [PubMed]
- Nandi D, Lin KY, O'Connor MJ, et al. Hospital Charges for Pediatric Heart Failure-Related Hospitalizations from 2000 to 2009. Pediatr Cardiol 2016;37:512-8. [Crossref] [PubMed]
- Rossano JW, Kim JJ, Decker JA, et al. Prevalence, morbidity, and mortality of heart failure-related hospitalizations in children in the United States: a population-based study. J Card Fail 2012;18:459-70. [Crossref] [PubMed]
- Burstein DS, Shamszad P, Dai D, et al. Significant mortality, morbidity and resource utilization associated with advanced heart failure in congenital heart disease in children and young adults. Am Heart J 2019;209:9-19. [Crossref] [PubMed]
- Davies RR, McCulloch MA, Haldeman S, et al. Urgent listing exceptions and outcomes in pediatric heart transplantation: Comparison to standard criteria patients. J Heart Lung Transplant 2017;36:280-8. [Crossref] [PubMed]
- Rossano JW, Cherikh WS, Chambers DC, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Twenty-first pediatric heart transplantation report-2018; Focus theme: Multiorgan Transplantation. J Heart Lung Transplant 2018;37:1184-95. [Crossref] [PubMed]
- Zafar F, Castleberry C, Khan MS, et al. Pediatric heart transplant waiting list mortality in the era of ventricular assist devices. J Heart Lung Transplant 2015;34:82-8. [Crossref] [PubMed]
- Morales DLS, Rossano JW, VanderPluym C, et al. Third Annual Pediatric Interagency Registry for Mechanical Circulatory Support (Pedimacs) Report: Preimplant Characteristics and Outcomes. Ann Thorac Surg 2019;107:993-1004. [Crossref] [PubMed]
- Rossano JW, Cantor RS, Dai D, et al. Resource Utilization in Pediatric Patients Supported With Ventricular Assist Devices in the United States: A Multicenter Study From the Pediatric Interagency Registry for Mechanically Assisted Circulatory Support and the Pediatric Health Information System. J Am Heart Assoc 2018. [Crossref] [PubMed]
- Morales DL, Zafar F, Rossano JW, et al. Use of ventricular assist devices in children across the United States: analysis of 7.5 million pediatric hospitalizations. Ann Thorac Surg 2010;90:1313-8; discussion 1318-9. [Crossref] [PubMed]
- Peng DM, Koehl DA, Cantor RS, et al. Outcomes of children with congenital heart disease implanted with ventricular assist devices: An analysis of the Pediatric Interagency Registry for Mechanical Circulatory Support (Pedimacs). J Heart Lung Transplant 2019;38:420-30. [Crossref] [PubMed]
- Smith M, Saunders R, Stuckhardt L, et al. editors. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Committee on the Learning Health Care System in America, Institute of Medicine. Washington, DC: The National Academies Press, 2013.
- Britto MT, Fuller SC, Kaplan HC, et al. Using a network organisational architecture to support the development of Learning Healthcare Systems. BMJ Qual Saf 2018;27:937-46. [Crossref] [PubMed]
- Leotsakos A, Zheng H, Croteau R, et al. Standardization in patient safety: the WHO High 5s project. Int J Qual Health Care 2014;26:109-16. [Crossref] [PubMed]
- Gaies M, Anderson J, Kipps A, et al. Cardiac Networks United: an integrated paediatric and congenital cardiovascular research and improvement network. Cardiol Young 2018. [Epub ahead of print]. [PubMed]
- FDA’s Pediatric Advisory Committee. Executive Summary: Berlin Heart Inc. EXCOR Pediatric Ventricular Assist Device. Available online: https://www.fda.gov/media/100172/download. Accessed 6/21/19 2016.
- Sherman RE, Anderson SA, Dal Pan GJ, et al. Real-World Evidence - What Is It and What Can It Tell Us? N Engl J Med 2016;375:2293-7. [Crossref] [PubMed]


