
Transition clinics: an observational study of themes important to young people with inflammatory bowel disease
Introduction
Recent epidemiological data has demonstrated a high overall prevalence and increasing incidence of inflammatory bowel disease (IBD) in the Canterbury region of New Zealand (1,2). Furthermore, the incidence of IBD in children in this region has increased many-fold over the last two decades (3). IBD in this age group can be complicated by nutritional deficiencies, impaired linear growth and psychological complications (4,5). In addition to facing various obstacles directly and indirectly related to their disease, these children all face the prospect of transitioning from paediatric to adult care at some stage following their diagnosis.
Transition of care is defined as a purposeful planned movement of adolescents and young adults with chronic physical and medical conditions from child-centred to adult-oriented health care systems (6). The absence of a smooth transition from paediatric to adult services is associated with various adverse outcomes, such as increased “lost to follow-up” rates, increased admission rates and variability in adherence to medications (7,8). Data from clinics managing other chronic illnesses such as type 1 diabetes and cystic fibrosis clearly supports the concept of transition clinics and provides a sound basis to apply such an approach in IBD (9,10).
Various barriers to successful transition in IBD have been described. Several reports indicate that adult gastroenterologists generally feel inadequately trained in adolescent care (11-13). In a recent survey of Australasian gastroenterologists, only 23% of respondents stated that adolescents with IBD were adequately prepared for transition to adult care (12). Poor handover of information and patients’ lack of responsibility for their own care were identified as major barriers to successful transition. Lack of self-efficacy and disease-specific knowledge are also likely to impact negatively on the transition process (14,15).
While many publications have examined the views of practitioners about transition and have provided guidelines for the process of transition, few studies have focused on the views and perspectives of young people about transition (16,17). The current study aimed to identify and explore the issues important to young people with IBD as they transfer to adult services.
Methods
Focus groups and questionnaire development
A qualitative study was undertaken initially to identify issues important to young people with IBD. Young people diagnosed with IBD at Christchurch Hospital, Christchurch, in the Canterbury region of New Zealand, were invited to participate in a focus group. Participants were selected to represent three distinct groups: “pre transition”, “within transition” and “post transition”. Eligibility for participation included diagnosis of IBD for more than a year, diagnosis before the age of 16 years and current age between 14 to 20 years. All participants gave informed consent. Ethical approval for the study was obtained through Southern Health and Disability Ethics Committee (HDEC) (Ref number: 14/STH/188).
The focus groups each met on one occasion and a semi structured group interview was conducted by a single investigator (SK). The interview was audio recorded for later thematic analysis. The interviews were analysed for predominant themes, opinions, concerns and ideas. These themes were then used to design an online questionnaire to evaluate young people’s thoughts about the transition process.
Online questionnaire
The questionnaire arising from the focus groups was initially piloted with four local young people with IBD for readability and appropriateness. The final questionnaire (available from the authors on request) was then used to ascertain further perspectives of the transition process in a larger group of young people who had been diagnosed with IBD before the age of 16 years.
The questionnaire asked respondents to self-report details about demographics, disease type, disease severity and medications (past and current). Respondents were asked questions about their own transition experience and factors relating to the transition process. Multi-choice, open text and ranking questions were included. Transition was defined within the questionnaire as the process from moving from pediatric to adult services. A specialist transition clinic was defined as one involving both a pediatrician and an adult gastroenterologist.
An invitation to complete the online questionnaire was circulated to local patients managed at Christchurch Hospital (Canterbury region) and nationally via the Crohn’s and Colitis New Zealand website and Facebook page. An invitation was also emailed to all regional Crohn’s and Colitis New Zealand support groups around New Zealand. The questionnaire was uploaded to an on-line platform (www.questionpro.com). Informed consent was implied by the participant’s completion of the questionnaire with ethics committee approval as earlier.
Results
Focus groups and questionnaire development
Seven participants aged between 14 and 21 years of age attended the focus groups. Three participants were pre-transition, two were within and two were post transition. All were patients seen at Christchurch Hospital, Canterbury, where there is a structured joint transition clinic.
Common themes included apprehension about meeting new teams, and being in new physical environments (Table 1). Participants were concerned about talking about potentially embarrassing issues while transitioning. There was agreement that having a shared clinic was positive. The groups felt that having an approachable doctor was important.
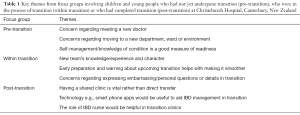
Full table
Participants who had transitioned felt that a joint clinic was positive and that having an IBD nurse would be helpful. The idea of using technology to aid in transition was also mentioned. The groups felt that self-management and disease knowledge is an important measure in assessing readiness for transition.
Background characteristics of online questionnaire respondents
Sixty respondents completed the online questionnaire, but seven were not eligible for inclusion (no diagnosis of IBD). All of the 53 remaining participants were diagnosed at 16 years or younger (Table 2). The age range of included children ranged from early adolescence to young adulthood. Forty-eight (90.6%) of the 53 participants were diagnosed with CD. Thirty-eight percent had previous surgery. Thirty-eight (71.7%) respondents were taking 1 or 2 medications daily, five were receiving three medicines and one four medicines. Nine were not currently on any therapy.
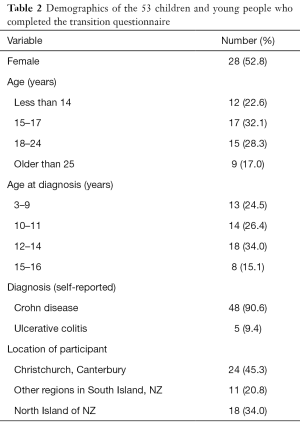
Full table
Experience of the respondents with transition
Ten (19%) of the participants had completed transition and eight (15%) participants were currently in transition. The remaining respondents were awaiting transition (n=10), did not have any experience of a transition process (n=22) or were unsure of their transition status.
Eighteen (34%) participants reported that they had access to a transition clinic in their current location. Nineteen (35.8%) participants were unsure whether they had a transition clinic. However, the majority of these participants were at the pre-transition age group and, therefore, may not have been aware yet of transition services provided at their locality.
Eighteen patients who were either in or had completed transition rated the quality of their transition experience. One participant who had completed transition found this process difficult. The other participants felt that the process was neutral (n=6), smooth (n=5) or extremely smooth (n=6).
Participants’ opinions about the transition process
The participants provided their opinions about the most important difficulties they faced in transitioning (Table 3). The most common difficulty overall, regardless of transition status was “Meeting a new doctor”. In the post transition group the difficulty ranked number one most commonly was “expressing embarrassing/personal questions”.
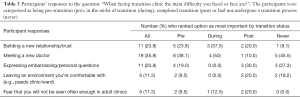
Full table
When considering how to determine readiness for transition, equal numbers of respondents ranked “Having stable, inactive disease” and “the patient’s own decision concerning readiness to transition” as the most important factors (Table 4). Three participants (all pre-transition) indicated that parental assessment was important.
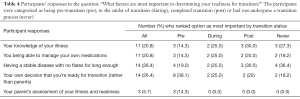
Full table
When asked to rank what they thought would make the transition to adult services easier, “The character of the adult IBD doctor” was ranked as most important by 28 of 53 respondents (Table 5). Three of the ten post transition patients and 4 of the 11 participants who had never been through a transition process, ranked IBD nurses as the strongest factor likely to make the transition to adult services easier.
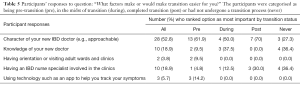
Full table
Discussion
The aim of this study was to identify and explore transition-related issues relevant to young people with IBD. A range of children and young people at different phases of the transition process were able to provide their opinions. The main concerns of these young patients were about meeting a new team and building new relationships.
As IBD incidence rises, especially among children (15,18), more young people will be moving into adulthood with this lifelong condition. A growing body of work from other chronic diseases suggests that participation in transition clinics improves disease specific outcomes (8-10). For example, a cohort of young people with IBD who had received a formalised transition clinic had improved outcomes including medication adherence, missed clinics, surgery and admission rates (14) The retrospective nature of this study means that the two groups were not comparable due to differences in practice over the time period of the study. Self-efficacy has also been shown to improve, along with increased knowledge of the need for medications, with participation in transition clinics (19,20).
In the current study, the participants perceived that the biggest difficulty they faced was building a new relationship or establishing trust with the adult gastroenterologist. The only group who did not rank this as most important was the “post” transition group, who ranked expressing personal or embarrassing issues as the most important difficulty that they had faced. This emphasis on the importance of the new doctor taking on their care was also evident in the responses to the question about what was important for making transition easier: the majority of the participants ranked “the character of the adult IBD doctor” as the most important factor.
Qualitative work by Gray et al. (13) found that concerns about receiving poorer quality care in the adult setting and loss of valued relationships with paediatric providers were amongst the main issues reported by patients and parents facing transition in IBD. These findings and the current study highlight that while clinicians rate patient’s self-efficacy and disease knowledge as very important, the patient has different priorities, and is concerned about leaving the familiar paediatrician for an unfamiliar adult physician.
The timing of and readiness for transition has been shown to be one of the most important factors determining the success of the process of transfer of care (7,21). Patients’ readiness and involvement, disease stability and health care providers’ communication are some of the factors that may contribute to this process (8,13). In the present study, the participants reported that the most important factors to determine readiness for transition were disease stability (i.e., no frequent or recent flares) and their own perception of their readiness. Few participants considered that parental assessment for readiness for transition was important. The physician’s opinion was not even established as a theme. Published guidelines rank disease knowledge and self-efficacy as important factors (22-24). Again this demonstrates a discrepancy between reported important factors for young people and those of their physicians.
Of encouraging note, almost all the participants who had been in or had completed transition rated the process to be straightforward. This suggests that while people are fearful, the actual experience is better than anticipated. The nature of the current study did not enable further analysis of the factors that contributed to a smooth transition in each case.
While this study has used qualitative data to identify options for specific research questions, and has also included participants who are at various stages of the transition process, there are a number of limitations. The questionnaire was not formally validated but was based on the relevant themes from the focus groups. The overall size of the group that completed the questionnaire is relatively small, although is comparable with other IBD transition studies (13,17,19). In addition, the number of study participants from the Canterbury District Health Board, where there is an established IBD transition clinic, was high compared with other regions, which could lead to bias. Personal correspondence would suggest that most children in NZ do not have access to a formal transition clinic, and ad hoc arrangements are made as necessary.
In conclusion, transition from paediatric to adult care is a challenging time for patients, their families and healthcare systems. If transition is not planned and personalised, there is a risk that patients may fall through the cracks and consequently receive suboptimal care and even disengage with services. The current data shows that patients are concerned about meeting a new team and building a new relationship or trust. However, they also consider the character of their new team to be one of the most important factors in making transition easier. Patients advocate for their independence and highlight their own decision as an important factor in assessing readiness. It is vital that planning and conducting a structured transition is a collaborative process involving the patient, parents and healthcare providers.
Acknowledgements
Thanks to all participants for their time and contributions and to Crohns and Colitis NZ for their assistance with circulation of survey document.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval for the study was obtained through Southern Health and Disability Ethics Committee (HDEC) (Ref number: 14/STH/188). Informed consent was obtained.
References
- Lopez RN, Evans HM, Appleton L, et al. Point Prevalence of Pediatric Inflammatory Bowel Disease in New Zealand in 2015: Initial Results from the PINZ Study. Inflamm Bowel Dis 2017;23:1418-24. [Crossref] [PubMed]
- Su HY, Gupta V, Day AS, et al. Rising Incidence of Inflammatory Bowel Disease in Canterbury, New Zealand. Inflamm Bowel Dis 2016;22:2238-44. [Crossref] [PubMed]
- Lopez RN, Appleton L, Gearry RB, et al. Rising Incidence of Paediatric Inflammatory Bowel Disease in Canterbury, New Zealand, 1996-2015. J Pediatr Gastroenterol Nutr 2018;66:e45-50. [Crossref] [PubMed]
- Day AS, Ledder O, Leach ST, et al. Crohn's and colitis in children and adolescents. World J Gastroenterol 2012;18:5862-9. [Crossref] [PubMed]
- Lemberg DA, Day AS. Crohn disease and ulcerative colitis in children: an update for 2014. J Paediatr Child Health 2015;51:266-70. [Crossref] [PubMed]
- Blum RW, Garell D, Hodgman CH, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health 1993;14:570-6. [Crossref] [PubMed]
- Goodhand J, Hedin CR, Croft NM, et al. Adolescents with IBD: the importance of structured transition care. J Crohns Colitis 2011;5:509-19. [Crossref] [PubMed]
- Philpott JR, Kurowski JA. Challenges in Transitional Care in Inflammatory Bowel Disease: A Review of the Current Literature in Transition Readiness and Outcomes. Inflamm Bowel Dis 2019;25:45-55. [Crossref] [PubMed]
- Cadario F, Prodam F, Bellone S, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 2009;71:346-50. [Crossref] [PubMed]
- Tuchman LK, Schwartz LA, Sawicki GS, et al. Cystic fibrosis and transition to adult medical care. Pediatrics 2010;125:566-73. [Crossref] [PubMed]
- Hait EJ, Barendse RM, Arnold JH, et al. Transition of adolescents with inflammatory bowel disease from pediatric to adult care: a survey of adult gastroenterologists. J Pediatr Gastroenterol Nutr 2009;48:61-5. [Crossref] [PubMed]
- Wright EK, Williams J, Andrews JM, et al. Perspectives of paediatric and adult gastroenterologists on transfer and transition care of adolescents with inflammatory bowel disease. Intern Med J 2014;44:490-6. [Crossref] [PubMed]
- Gray WN, Resmini AR, Baker KD, et al. Concerns, Barriers, and Recommendations to Improve Transition from Pediatric to Adult IBD Care: Perspectives of Patients, Parents, and Health Professionals. Inflamm Bowel Dis 2015;21:1641-51. [Crossref] [PubMed]
- Cole R, Ashok D, Razack A, et al. Evaluation of Outcomes in Adolescent Inflammatory Bowel Disease Patients Following Transfer From Pediatric to Adult Health Care Services: Case for Transition. J Adolesc Health 2015;57:212-7. [Crossref] [PubMed]
- Benchimol EI, Fortinsky KJ, Gozdyra P, et al. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis 2011;17:423-39. [Crossref] [PubMed]
- Gray WN, Reed-Knight B, Morgan PJ, et al. Multi-Site Comparison of Patient, Parent, and Pediatric Provider Perspectives on Transition to Adult Care in IBD. J Pediatr Nurs 2018;39:49-54. [Crossref] [PubMed]
- Dabadie A, Troadec F, Heresbach D, et al. Transition of patients with inflammatory bowel disease from pediatric to adult care. Gastroenterol Clin Biol 2008;32:451-9. [Crossref] [PubMed]
- Ruel J, Ruane D, Mehandru S, et al. IBD across the age spectrum: is it the same disease? Nat Rev Gastroenterol Hepatol 2014;11:88-98. [Crossref] [PubMed]
- Yerushalmy-Feler A, Ron Y, Barnea E, et al. Adolescent transition clinic in inflammatory bowel disease: quantitative assessment of self-efficacy skills. Eur J Gastroenterol Hepatol 2017;29:831-7. [Crossref] [PubMed]
- Schmidt S, Herrmann-Garitz C, Bomba F, et al. A multicenter prospective quasi-experimental study on the impact of a transition-oriented generic patient education program on health service participation and quality of life in adolescents and young adults. Patient Educ Couns 2016;99:421-8. [Crossref] [PubMed]
- Kim J, Ye BD. Successful transition from pediatric to adult care in inflammatory bowel disease: what is the key? Pediatr Gastroenterol Hepatol Nutr 2019;22:28-40. [Crossref] [PubMed]
- Baldassano R, Ferry G, Griffiths A, et al. Transition of the patient with inflammatory bowel disease from pediatric to adult care: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2002;34:245-8. [Crossref] [PubMed]
- Brooks AJ, Smith PJ, Lindsay JO. Monitoring adolescents and young people with inflammatory bowel disease during transition to adult healthcare. Frontline Gastroenterol 2018;9:37-44. [Crossref] [PubMed]
- Hait E, Arnold JH, Fishman LN. Educate, communicate, anticipate-practical recommendations for transitioning adolescents with IBD to adult health care. Inflamm Bowel Dis 2006;12:70-3. [Crossref] [PubMed]


