Epidemiological survey on newborns born at the obstetric departments in hospitals in mid-southern region of China in 2005
Perinatal mortality and morbidity are significant global health problems, and the major causes of perinatal deaths include preterm birth, neonatal infection and asphyxia1 (1). Premature infants are at high risk for morbidity and mortality because of bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), and periventricular leukomalacia (PVL) (2). The morbidity and mortality of newborns are important indicators for evaluating the health care level of a certain country/area. Mid-southern region of China include six provinces in the middle and southern parts of China, whose economic development and health care services show wide disparities.
There are many factors of preterm delivery, such as medication or infection during pregnancy; threatened abortion; PIH; preterm rupture of membranes; antepartum hemorrhage; history of abortion/induced abortion; history of preterm delivery or stillbirth; twins/multiplets; malposition; intra-uterine asphyxia; amniotic fluid contamination; placenta aging; umbilical cord abnormality; and others. However, the roles of main risk factors that may predispose neonates to these direct causes of mortality are less well understood. It is known that cesarean section is a common surgery for the management of high-risk pregnancy. As shown in many literatures, the cesarean section-related mortality and complications were 2-4 folds of those of vaginal birth, while the incidence of neonatal asphyxia showed no remarkable decrease (3,4). Furthermore, newborns are more susceptible to complications such as wet lung, amniotic fluid aspiration, and asphyxia because they lack the process of uterine contraction and squeezing through the birth canal (5).
In this study, we investigated the conditions of newborns who born at obstetric departments in the hospitals in this region in 2005 with an attempt to provide new evidences for clinical decision-making.
Subjects and methods
Subjects
Totally 23 hospitals in the mid-southern region of China, including medical college-affiliated hospitals in the capital cities, province-level people’s hospitals, and province-level maternal and child health care hospitals, participated in this survey. Furthermore, one comprehensive hospital and one maternal and child health care hospital from non-capital cities were also randomly selected for each province. All the subjects were newborns who were born at obstetric departments from January 1, 2005 to December 31, 2005. The survey protocol was developed based on the scheme developed by the Neonatal Subspecialty Group of Chinese Pediatric Society (6). The obstetric department and newborn department in each hospital were assigned to investigate about 1,000 newborns, respectively; if the sum was less than 1,000, all the newborns from that department were enrolled for analysis. For departments with the number of newborns more than 1,000, those who were discharged throughout the first 20, 15, 10, or 7 days of each month (i.e. 2/3, 1/2, 1/3, or 1/4 of all cases) were selected for analysis, making the surveyed newborns in both obstetric department and newborn department reach 1,000 cases each.
Statistical analysis
Statistical analysis was performed using SPSS 11.0 software. Numeration data were compared using Chi square test. P<0.05 was considered significantly different.
Results
General data
Totally 15,582 newborns were born at the obstetric departments of these 23 hospitals in 2005, with a male to female ratio of 1.16:1. The incidence of preterm birth was 8.11%, and the rate of full-term delivery was 91.89%. The distribution of gestational ages at delivery was as follows: The percentages of the gestational ages at delivery that were less than 28 weeks, between 28 and 31 weeks, between 32 and 36 weeks, between 37 and 42 weeks, and more than 42 weeks were 0.29%, 0.95%, 6.87%, 91.31%, and 0.58%, respectively. More specifically, for the preterm infants, the percentages of the gestational ages at delivery that were less than 28 weeks, between 28 and 31 weeks, and between 32 and 36 weeks were 3.58%, 11.66%, and 84.76%; while for the full-term infants, the percentages of the gestational age at delivery that were between 37 and 42 weeks, and more than 42 weeks was 99.37% and 0.63%, respectively. For the birth weight, the percentages of those <1,000 g, 1,000-1,499 g, 1,500-2,499 g, 2,500-3,999 g, and >4,000 g were 0.21%, 0.52%, 5.34%, 89.83%, and 4.10%. More specifically, the distribution of the birth weight of the preterm infants was 1.57%, 6.21%, 41.98%, 49.49%, and 0.75% for body weight <1,000 g, 1,000-1,499 g, 1,500-2,499 g, 2,500-3,999 g, and >4,000 g, and that of full-term infants was 0.11%, 2.18%, 93.31%, and 4.40% for body weight 1,000-1,499 g, 1,500-2,499 g, 2,500-3,999 g, and >4,000 g. Mothers older than 35 years accounted for 6.14%; more specifically, women who were mothers of preterm infants and older than 35 years accounted for 9.26%, while women who were mothers of full-term infants and older than 35 years accounted for 5.26% (χ2=41.689, P<0.001).
Pregnancies of mothers
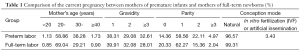
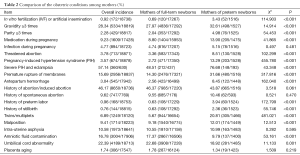
We also analyzed the data of mothers of the enrolled newborns (Tables 1,2). In their current pregnancies, the percentage of babies born to parents who had undergone in-vitro fertilization (IVF) or artificial insemination accounted for 3.43% of preterm infants, which was significantly higher than that among full-term newborns (χ2=114.903, P<0.001). The rates of medication during pregnancy, threatened abortion, preterm rupture of membranes, and antepartum hemorrhage were higher among mothers of preterm infants than mothers of full-term newborns. Analysis also showed that the incidence of pregnancy-induced hypertension syndrome (PIH), especially severe PIH or eclampsia, was significantly higher among mothers of preterm infants than mothers of full-term newborns.
Full table
Full table
During their current pregnancies, the rate of spontaneous vaginal delivery or cesarean section was 57.52% or 40.82%, respectively. Notably, 29.91% of cesarean sections were due to social factors. Preterm infants tended to have higher rates of twins, multiplets, and malposition than full-term babies, while the latter had higher incidence of amniotic fluid contamination. The incidences of intra-uterine asphyxia and placenta aging showed no significant different between the preterm infants and full-term newborns.
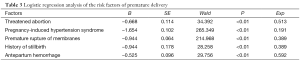
Our Logistic regression analysis included the following risk factors of preterm delivery: mother >35 years; conception mode; having gravidity ≥3; having parity ≥3; medication or infection during pregnancy; threatened abortion; PIH; preterm rupture of membranes; antepartum hemorrhage; history of abortion/induced abortion; history of preterm delivery or stillbirth; twins/multiplets; malposition; intra-uterine asphyxia; amniotic fluid contamination; placenta aging; umbilical cord abnormality; and others. It was found that threatened abortion, PIH, preterm rupture of membranes, antepartum hemorrhage, and history of stillbirth were the risk factors of preterm delivery (Table 3).
Full table
Conditions of newborns
The incidences of neonatal asphyxia were 3.78% and 1.11% one minute and five minutes after birth (0.75% and 0.48% for heavy asphyxia). Compared with full-term newborns (2.82%), preterm newborns tended to have higher rate of asphyxia one minute after birth (14.73%) (χ2=523.605, P<0.001).
The mortality of newborns born at these obstetric departments was 0.55% (5.56% for preterm infants). Among them, the mortality of preterm newborns was 5.56%, which was significantly higher than that in full-term newborns (0.11%) (χ2=673.311, P<0.001).
Discussion
The mortality of newborns in China has shown a decreasing trend along with the development of socio-economic conditions and medical sciences. According to the official statistics, the mortality of newborns in China was 13.2% in 2005 (7). Our current survey showed that the mortality of newborns born at obstetric departments in hospitals in mid-southern region of China was 0.55%, which was lower than the national average. Along with the continuous development of perinatal medicine, both the incidence of preterm delivery and the survival rate of preterm babies have increased. Our data have shown that the incidence of preterm delivery was 8.11% in the mid-southern region of China, which was lower than the rate in the United States in 2005 (12.7%) (8) but higher than China’s nationwide data in 2002 (7.8%) (9), suggesting that the rate of preterm delivery has shown an increasing trend.
It was found in our study that threatened abortion, PIH, preterm rupture of membranes, antepartum hemorrhage, and history of stillbirth were the risk factors of preterm delivery. Therefore, routine antenatal examinations for pregnant women (especially those who are older than 35 years) and active prevention/control of pregnancy-related complications will be important to prevent preterm delivery and lower the incidence and case-fatality of preterm babies.
Cesarean section is a common surgery for the management of high-risk pregnancy. In our survey, the rate of cesarean section reached 40.82%, among which 29.91% were due to social factors. In the past decades, the misunderstanding of cesarean section (especially social factors) has made the rate of cesarean section unproportionally high (3,10). Early in 1980s, the World Health Organization proposed that the rate of cesarean section should not exceed 15%. Currently, the rates of cesarean section in the industrialized countries are maintained around 5-20% (11), but are far higher in most hospitals in China. Therefore, the indications of cesarean section should be strictly followed to decrease its rate.
Also in our survey, the incidence of neonatal asphyxias who were born at the obstetric departments in hospital in mid-southern region of China was 3.78%, which was lower than those in some Chinese hospitals (5-11%) (10,12), but was still remarkably higher than those in developed countries. For example, it was 0.94% in Langspitali University Hospital in Iceland from 1997 to 2001 (13) and 0.09% in Edinburgh, UK, in 2005 (14). The prognosis of neonatal asphyxia is highly depended on the technique applied for resuscitation and its effectiveness. With effective and close cooperation between obstetric department and pediatric department, the application of new resuscitation method may dramatically decrease the incidence of neonatal asphyxia (15,16). Our survey demonstrated that the incidence of neonatal asphyxia was still high in the mid-southern region of China. Therefore, it is important to strengthen the cooperation between obstetric departments and pediatric departments, improve the quality of antenatal examination, and enhance perinatal monitoring for high-risk pregnancies. Once an intra-uterine asphyxia is identified, an effective new resuscitation method should be actively and strictly applied, so as to improve the quality of resuscitation.
Hospitals participated in this survey (sorted in Hanyu Pinyin order): Guangdong Guangzhou No.1 People’s Hospital (Zhang Youxiang), Shenzhen Bao’an District Maternal and Child Health Care Hospital (Ye Zhenzhi), Guangdong Shenzhen People’s Hospital (Wu Benqing), Guangdong Province People’s Hospital (Nong Shaohan), Guangxi Beihai Maternal and Child Health Care Hospital (Wang Ruihua), Guangxi Beihai People’s Hospital (Wang Ling), Guangxi Maternal and Child Health Care Hospital (Liu Xianzhi), Guangxi Mingzu Hospital, Guangxi Yulin Maternal and Child Health Care Hospital, Haikou Maternal and Child Health Hospital (Shi Lin), Hainan Sanya People’s Hospital (Hu Xia), Hainan Maternal and Child Health Care Hospital (Guo Xiufeng), Hainan Wenchang Qingling Maternal and Child Health Care Hospital (Chen Xujie), The Affiliated Hospital of Hainan Medical University (Guo Shaoli), He’nan Jiaozuo Maternal and Child Health Care Hospital (Mu Xiurong), Henan Luoyang Women and Children’s Health Care Center (Zhao Baili), Hubei Provincial Maternal and Child health Care Hospital (Xia Shiwen), Hunan Provincial Maternal and Child Health Care Hospital (Cheng Linxia), Hunan People’s Hospital (Li Yun), Hunan Xiangtan Maternal and Child Health Care Hospital (Zeng Jianwu), Hunan Xiangtan Central Hospital (Chen Xiaohua), Zhengzhou University Affiliated Third Hospital (Cheng Xiuyong), Central South University Affiliated Xiangya Hospital (Wang Qinghong).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kafulafula G, Mwatha A, Chen YQ, et al. Intrapartum antibiotic exposure and early neonatal, morbidity, and mortality in Africa. Pediatrics 2009;124:e137-44. [PubMed]
- Engle WA, Tomashek KM, Wallman C. “Late-preterm” infants: a population at risk. Pediatrics 2007;120:1390-401. [PubMed]
- Lu YQ, Nong WZ. Retrospective analysis on cesarean section rate over 10 years. Guang Xi Yi Xue 2004;26:1001-2.
- Huang SH, Huang YM. Analysis of reasons for high cesarean section rate. Zhong Guo Fu You Bao Jian 2005;20:1813-4.
- Niu ZY, Jin Q, Zhang X. Analysis of 120 cases of newborn asphysia after cesarean section. Yun Nan Yi Yao 2007;28:270-1.
- The Subspecialty Group of Neonatology, Pediatric Society, Chinese Medical Association. Epidemiologic survey for hospitalized neonates in China. Zhong Guo Dang Dai Er Ke Za Zhi 2009;11:15-20. [PubMed]
- China health development in 2006 statistical bulletin.Available online: http://www.moh.gov.cn/publicfiles/business/htmlfiles/zwgkzt/pgb/200805/34857.htm
- Raju TN, Higgins RD, Stark AR, et al. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics 2006;118:1207-14. [PubMed]
- The Subspecialty Group of Neonatology, Pediatric Society, Chinese Medical Association. An initial epidemiologic investigation of preterm infants in cities of China. Zhong Guo Dang Dai Er Ke Za Zhi 2005;7:25-9.
- Fang ZS. Analysis of change in cesarean section rate and its related social factor over 5 years. Yi Yao Lun Tan Za Zhi 2007;28:50-1.
- Zhang JP. Analysis on cesarean section between 1997 and 2006. Zhong Guo Fu You Bao Jian 2007;22:2340-1.
- Ma RY. Clinical analysis of 324 cases of newborn asphysia. Xian Dai Yi Yuan 2007;7:36-7.
- Becher JC, Stenson BJ, Lyon AJ. Is intrapartum asphyxia preventable? BJOG 2007;114:1442-4. [PubMed]
- Palsdottir K, Dagbjartsson A, Thorkelsson T, et al. Birth asphyxia and hypoxic ischemic encephalopathy, incidence and obstetric risk factors. Laeknabladid 2007;93:595-601. [PubMed]
- Wyllie J, Niermeyer S. The role of resuscitation drugs and placental transfusion in the delivery room management of newborn infants. Semin Fetal Neonatal Med 2008;13:416-23. [PubMed]
- Nicolai T. Pediatric resuscitation. Curr Opin Anaesthesiol 2008;21:204-8. [PubMed]


