
Systematic review and meta-analysis of the curative effects and safety of endoscopic sinus surgery in children with chronic sinusitis with nasal polyps
Introduction
Childhood rhinosinusitis is an infectious respiratory tract disease caused mainly by pathogenic infection and is correlated with multiple factors, including nasal stenosis, nasal trauma, and poor resistance (1). The incidence of the disease is highest among children aged between 7 and 10 years old. Pathogens that can cause rhinosinusitis include viruses, bacteria (e.g., Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus), and fungi. Rhinosinusitis is an inflammatory disease of the sinus mucosa and often coexists with rhinitis (2,3). Owing to some special physiological features among children, such as relative stenosis of the nasal base, ostiomeatalex, and sinus openings, and hypertrophy of the tonsil and gland, the mucosal response to inflammation in children is more obvious than that of adults. Therefore, this type of infection is very likely to occur among children, which results in rhinostegnosis (4).
Common symptoms of chronic childhood rhinosinusitis include persistent or intermittent nasal congestion, mucous or sticky purulent nasal discharge, and local symptoms, such as sleep disorder, ear discomfort, and otitis media (5). Constitutional symptoms include fever, fear of cold, and loss of appetite. Furthermore, the mental state of children also changes into dysphoria or excessive crying (6,7), which has a certain influence on the child’s hearing, visual acuity, and whole-body development, including combined purulent otitis media, tympanic membrane perforation, and diminution of hearing and visual acuity (8,9). Nasal endoscopy can help to directly observe the sinuses affected by inflammation and obtain sinus samples. Anti-infection therapy is the main treatment method and antibiotics can be used for symptomatic purposes. Febrifuge is used during fever, and nasal surgery is required if necessary (10,11).
Rhinosinusitis with nasal polyps refers to chronic sinusitis with nasal polyp. Nasal normal saline medication treatment can be adopted for small polyps. After rinsing of the nasal cavity secretions and nasal polyps, the existing infections are treated with antibiotics (12). Following conservative treatment with drugs, some patients’ nasal sinusitis polyps shrink appropriately and the symptoms are controlled and alleviated (13,14). However, surgical treatment is required for polyps and sinusitis caused by poor drug treatment effects, recurrence of polyps, and abnormal anatomical structure of the nasal cavity (15,16). In such cases, the required surgery involves endoscopic resection of the nasal polyps and open sinus surgery, which are combined with postoperative nasal irrigation and nasal spray. In most cases, polyps and sinusitis are cured within 1 to 3 months after surgery (17,18). Nasal endoscopy can be performed with soft or hard endoscopy, which is determined by the proficiency of the examiners and the ages of children with polyps and sinusitis as well as the degree of their cooperation (19,20). When viscous purulent secretions are attached to the nasal cavities and nasopharynx of children with chronic rhinosinusitis, artifacts may appear on computed tomography (CT) or cervical X-ray films. Hence, it is more valuable to judge the sizes of nasal mucosal lesions and adenoids and whether the pharyngeal tube pharynx is compressed. Nasal endoscopy can be adopted as the preferred auxiliary examination method (21-23).
Although great progress has been made in the surgical treatment of sinusitis with nasal polyps, the recurrence rate is still high, and the surgical methods and perioperative management have great influence on the therapeutic effect of the disease (24). In addition, Adriaensen et al. (25) found that endoscopic sinus surgery for sinusitis with nasal polyps can effectively promote the cure time and treatment effect. However, it is not widely used because its safety is not clear. Therefore, this study adopts meta-analysis method to study the therapeutic effect of endoscopic sinus surgery on children with chronic sinusitis and nasal polyps, analyze its effectiveness and safety, and provide theoretical basis for clinical treatment. We present the following article in accordance with the PRISMA reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-189/rc).
Methods
Literature retrieval
We performed an electronic literature search of the PubMed, Medline, Embase, China Biology Medicine disc, Chinese National Knowledge Infrastructure, Wanfang, VIP, and Google Scholar databases from the date of establishment of the database to December 30, 2021. The Boolean logic searching method was employed to retrieve relevant articles using “endoscopic sinus surgery”, “antrochoanal polyps”, “chronic sinusitis with nasal polyps”, and “nasal polyps” as the search items. Various search items were also combined freely. The methodological quality of the included literature was evaluated by using the quality evaluation standard of randomized controlled trial (RCT) in Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. Following retrieval of multiple relevant articles, search engines were used to trace the identified articles and reference sheets with published overviews to search for literature that was not cited in the databases. The latest research progress was obtained by contacting experts and researchers in the relevant fields.
Literature inclusion and exclusion criteria
The included articles needed to meet all of the following standards: (I) the research objects were diagnosed with chronic sinusitis with nasal polyps, without pathological type limitation; (II) the intervention measure for patients in the control group was traditional surgical treatment; (III) patients in the experimental group received endoscopic sinus surgical treatment; (IV) research type: randomized controlled trial.
Studies meeting one of the following standards were eliminated: (I) studies involving research objects with severe infectious diseases; (II) articles that did not involve a randomized control trial; (III) literature with missing or unavailable data; (IV) the basic information of the research object included in the literature cannot be extracted; (V) duplicate articles or those that included few selected trial samples.
Two senior specialists independently audited the abstracts and titles as well as the full texts of the retrieved articles. Before the screening, three pre-trials needed to be carried out. Disagreements between the two experts were resolved by discussion and consensus between the two specialists. Alternatively, a third expert was asked to arbitrate.
Quality evaluation
According to Cochrane’s requirements, the methodological quality of the included literature was evaluated by using the quality evaluation standard of RCT in Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. Also, the star system was employed to measure the outcomes of research objects, case comparisons, as well as comparisons between groups (9 stars represented a full maximum score). Selected articles that scored ≥7 stars were regarded as high-quality studies with a low risk of bias. Articles that scored ≤1 star or 0 star were viewed as low-quality studies with a high risk of bias. Studies that scored 2–6 stars were seen considered medium-quality studies with a medium risk of bias.
Two senior specialists independently evaluated the quality of the articles. Before the screening, three pre-trials needed to be carried out. Disagreements between the two experts were resolved by discussion and consensus between the two specialists. Alternatively, a third expert was asked to arbitrate.
Data retrieval
Two senior specialists employed the uniform Excel worksheet to independently extract the data. Before the screening, three pre-experiments needed to be carried out. Disagreements between the two experts were resolved by discussion and consensus between the two specialists. Alternatively, a third expert was asked to arbitrate. The extracted data included the following items: (I) the first author and year of publication; (II) the number of patients in the two groups; (III) the division of patients and therapies utilized for the control and experimental groups; (IV) the recovery indexes of patients after treatment, such as postoperative intervention, postoperative recurrence, postoperative polyp formation, and postoperative visual analogue scale (VAS) pain scores.
Statistical methods
Meta-analysis was conducted by using Review manager5.3 software. The odds ratio (OR) or rate ratio (RR) value and 95% confidence interval (CI) are used as the statistics of curative effect analysis for the classified variables of research data, and mean difference (MD) or standardized mean difference (SMD) and 95% CI are used as the statistics of curative effect analysis for the continuous variables of research data. Firstly, the heterogeneity test (Q test) is carried out for the included studies. The bias risk assessment chart of Review Manager software is used to show the risk bias assessment results included in the references. Each effect is expressed by 95% confidence interval. When P>0.1 and I2<50%, the fixed effect model was used for meta-analysis. When P<0.1 and I2>50%, the random effect model was used for meta-analysis.
Results
Summary of literature collection results and quality evaluation
As shown in Figure 1, a total of 544 articles were retrieved. Of these, 243 were removed after reading the titles and abstracts, and another 292 were excluded by examining the full texts. The excluded articles mainly included 100 articles with research objects suffering from other systemic diseases and mental diseases, 37 articles without clinical trials, 44 articles with subjects did not meet inclusion criteria, 40 articles with research information that could not be extracted, and 71 articles with research outcomes lacking original data. Finally, 9 articles were included for meta-analysis. Table 1 shows the basic information of the included articles. The publication year of these articles ranged from 2007 to 2019. Figure 2 shows the results of literature quality evaluation, which demonstrated that five articles scored ≥7 stars, three scored 2–6 stars, and one scored <2 stars. All of the above articles were medium- or high-quality studies.
Table 1
| First author | Publication year | Number of patients | Therapies | Follow-up visit length (months) | |||
|---|---|---|---|---|---|---|---|
| Control group | Experimental group | Control group | Experimental group | ||||
| Smith (17) | 2016 | 80 | 80 | Traditional surgical treatment | Endoscopic sinus surgery | 3 | |
| Murr (18) | 2011 | 38 | 38 | Traditional surgical treatment | Endoscopic sinus surgery | 2 | |
| Marple (19) | 2012 | 105 | 105 | Traditional surgical treatment | Endoscopic sinus surgery | 3 | |
| Luong (20) | 2018 | 80 | 80 | Traditional surgical treatment | Endoscopic sinus surgery | 3 | |
| Konstantinidis (21) | 2007 | 31 | 31 | Traditional surgical treatment | Endoscopic sinus surgery | 12 | |
| Konstantinidis (22) | 2010 | 27 | 27 | Traditional surgical treatment | Endoscopic sinus surgery | 12 | |
| Forwith (23) | 2016 | 47 | 53 | Traditional surgical treatment | Endoscopic sinus surgery | 6 | |
| Bugten (24) | 2008 | 55 | 56 | Traditional surgical treatment | Endoscopic sinus surgery | 3 | |
| Adriaensen (25) | 2017 | 18 | 18 | Traditional surgical treatment | Endoscopic sinus surgery | 2 | |
Bias risk assessment outcomes
Figures 3,4 show the evaluation outcomes of multiple risk bias charts of the included articles drawn using Review Manager software. Each methodological characteristic of the articles was included, and the assessment outcomes were input into computers to create the bias risk assessment charts. The charts suggested that the bias risks of random sequence generation (selection bias), allocation concealment (selection bias), blinding of outcome assessment (detection bias), and incomplete outcome data [attrition bias, selective reporting (reporting bias)] were low. The risk bias assessment of the blinding of participants and personnel (performance bias) and other biases was about 50%. The risk bias of articles was remarkably low, except for the articles by Konstantinidis et al. (2007) (21) and Luong et al. (2018) (20).
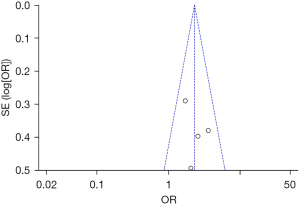
Comparison of polyp formation
Figure 5 displays the polyp formation comparison results among patients in the two groups after treatment, which indicated that the percentage of the research findings of Marple et al. (2012) (19) was the highest final combined results, accounting for 71.9%. The horizontal lines of the 95% CI of most articles crossed invalid vertical lines. Three included articles compared polyp formation among the patients, including a total of 161 research objects in the control and experimental groups, respectively. The polyp formation comparison between patients in the two groups after treatment indicated no statistical heterogeneity (Chi2=0.03, I2=0%, P=0.98). Also, the joint effect size (rhombus blocks) intersected invalid vertical lines, the odds ratio (OR) reached 2.18, and the 95% CI amounted to (1.22, 3.88). The analysis using fixed-effects models demonstrated that the number of patients with polyp formation in the experimental group was significantly less than that in the control group (Z=2.65, P=0.008).
Figure 6 shows the funnel plot illustrating the polyp formation comparison outcomes of patients in the two groups after treatment. The included circles were evenly and roughly symmetrical on both sides of the invalid vertical line, which indicated that the included articles showed no obvious publication bias.
Comparison of postoperative intervention
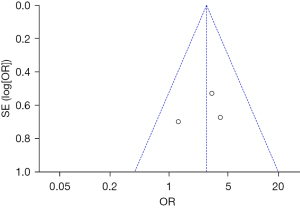
Figure 7 shows the postoperative intervention comparison results of patients in the two groups after treatment, which indicated that the percentage of the research results of Marple et al. (2012) (19) was the highest in the final combined results, accounting for 45.6%, followed by the findings of Luong et al. (2018) (20) (27.3%). Also, the transverse lines of the 95% CI of most articles were to the right of the ineffective longitudinal lines, while the transverse lines of only a few articles crossed the invalid vertical lines. Four articles compared the postoperative intervention among patients, including a total of 641 research objects in the control and experimental groups, respectively. The results demonstrated no statistical heterogeneity (Chi2=2.61, I2=0%, P=0.46). The joint effect size (rhombus blocks) was to the right of the ineffective longitudinal line. Also, the OR reached 2.30 and the 95% CI amounted to (1.61, 3.30). The analysis using fixed-effects models indicated that the differences in postoperative intervention between patients in the two groups showed statistical significance, and postoperative intervention of patients in the control group was markedly more frequent than that in the experimental group (Z=4.56, P<0.00001).
Figure 8 shows the funnel plot illustrating the comparison of postoperative intervention of patients in the two groups after treatment below. Most included circles were concentrated in the apical region with high research accuracy. The circles were to the left and right of the middle line with symmetrical distribution, which demonstrated that the included articles showed no obvious publication bias.
Comparison of postoperative recurrence of patients in the two groups
Postoperative follow-up visits were implemented for patients to analyze recurrence. Figure 9 displays the results of the comparison of postoperative recurrence between the two groups below, which indicated that the percentage of the research findings of Bugten et al. (2008) (24) was the highest in the final combined results, accounting for 34.3%. Moreover, the transverse lines of the 95% CIs of most articles were to the right of the ineffective longitudinal lines, while the transverse lines of only a few articles intersected the invalid vertical lines. Three articles compared the postoperative recurrence of patients, including a total of 182 research objects in the control group, and 189 research objects in the experimental group. The results showed no statistical heterogeneity (Chi2=1.59, I2=0%, P=0.45). Also, the joint effect size (rhombus blocks) was to the right of the invalid vertical lines. The OR reached 2.78 and the 95% CI amounted to (1.40, 5.52). The analysis using fixed-effects models showed that postoperative recurrence of patients in the experimental group was significantly less frequent than that in the control group (Z=2.92, P=0.004).
Figure 10 shows the funnel plot displaying the comparison of postoperative recurrence in the two groups, which demonstrated that the included circles were concentrated in the apical region with high research accuracy. The circles were to the left and right of the middle line with a roughly symmetrical distribution, which indicated that the included articles showed no obvious publication bias.
Postoperative VAS scores of patients in two groups
Figure 11 shows the results of the comparison of postoperative VAS pain scores among patients in the control group and experimental groups. The percentage of the research results of the study conducted by Konstantinidis et al. (2007) (21) was the highest in the final combined results, accounting for 46.1%. Furthermore, the transverse lines of 95% CI of articles were all on the right side of the ineffective longitudinal lines, without intersection. Four articles compared the postoperative VAS pain scores among patients, including a total of 227 research objects in the control and experimental groups, respectively. The results revealed statistical heterogeneity (Chi2=12.63, I2=84%, P=0.002). The joint effect size (rhombus blocks) was to the right of the ineffective longitudinal lines. Also, the MD reached 4.51 and the 95% CI amounted to (3.96, 5.05). The analysis using random-effects models indicated that the postoperative VAS scores of patients in the experimental group were markedly lower than those in the control group (Z=16.29, P<0.00001).
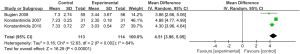
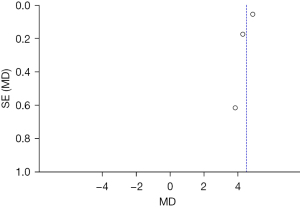
Figure 12 shows the funnel plot demonstrating the results of the comparison of postoperative VAS scores between the two groups. The included circles were to the left and right of the middle line with a roughly symmetrical distribution, which indicates that the articles showed no obvious publication bias.
Discussion
Chronic rhinosinusitis with nasal polyps has a broad impact on the population worldwide, with a global incidence of nearly 4% (26). Once mature, nasal polyps will block the sinus openings and normal airflow, resulting in nasal congestion, rhinorrhea, facial pain, and anosmia. Early-stage and small nasal polyps with rhinosinusitis can be treated with drugs, mainly including antibiotics, mucus promoters, short-term nasal vasoconstrictors, and glucocorticoid nasal sprays (such as roxithromycin, cimetidine tablets, ephedrine hydrochloride and nitrofurazone nasal drops, and flixonase) (27). The aforementioned drugs can assist in normal saline rinsing of the nasal cavity and promote the discharge of secretions and functional recovery of the mucosa. Surgical treatment is the best therapeutic method for rhinosinusitis with large nasal polyps or cases with poor drug therapy effects. Surgery needs to be performed under nasal endoscopy, and regular postoperative follow-up visits and nasal medications are required, which can effectively prevent recurrence (28).
Meta-analysis was adopted in this research, which included a total of 9 included articles; the randomized control grouping method was adopted applied for 8 articles and the retrospective analysis method was used for only one article, which resulted in bias among the included articles. However, this bias had little influence on the results of the research in general. The results of a single study may lack certain reliability. Meta-analysis was used to quantitatively integrate every article to avoid potential differences caused by the sampling of different populations among each article. In addition, the sample number was increased and the reliability of the conclusion was improved according to the various weights assigned to the outcomes by the sample number of each article (29). The quality of meta-analysis depended primarily on the authenticity and integrity of the analyzed articles. Considering the objective influences of the articles, the number of the articles was limited. In subsequent research, it is necessary to increase the sample size and avoid bias during the analysis.
The compound Boolean logic searching method was used to conduct a meta-analysis of relevant studies comparing traditional surgical treatment and endoscopic sinus surgery to investigate the curative effects and safety of endoscopic sinus surgery in children with chronic sinusitis with nasal polyps. The outcomes indicated that the comparison of polyp formation in the two groups after treatment demonstrated no statistical heterogeneity (Chi2=0.03, I2=0%, P=0.98). The analysis using fixed-effects models revealed that the number of patients with polyp formation in the experimental group was significantly less than that in the control group (Z=2.65, P=0.008). It also demonstrated that differences in the postoperative intervention of patients in the two groups showed statistical significance. The postoperative intervention in control group patients was markedly more frequent (Z=4.56, P<0.00001), which was similar to the findings of Wang et al. (2020) (30).
After surgical treatment for sinusitis, recurrence may occur in nearly 80% of patients, and about 40% of patients require a second surgical treatment. Moreover, most patients still have difficulty in controlling the disease 3 to 5 years after the sinus surgery. Systemic corticosteroid therapy can be used for patients on the basis of sinus surgery. The results of the comparison of postoperative recurrence in the two groups revealed no statistical heterogeneity (Chi2=1.59, I2=0%, P=0.45). The analysis using fixed-effects models showed that postoperative recurrence among patients in the experimental group was significantly less frequent than that in the control group (Z=2.92, P=0.004).
The results of the comparison of postoperative VAS scores between the two groups suggested statistical heterogeneity (Chi2=13.53, I2=78%, P=0.004). The analysis using random-effects models demonstrated that the postoperative VAS scores of patients in the experimental group were notably lower than those in the control group (Z=18.06, P<0.00001). In summary, endoscopic surgical therapy not only reduces the postoperative polyp formation and postoperative recurrence but also effectively improves postoperative pain among patients. Furthermore, it showed excellent curative effects and high safety in the treatment of children with sinusitis with nasal polyps.
Conclusions
The compound Boolean logic searching method was adopted in this paper to conduct a meta-analysis of relevant studies comparing traditional surgical treatment and endoscopic sinus surgery to explore the efficacy and safety of endoscopic sinus surgery in children with chronic sinusitis with nasal polyps. The results revealed that endoscopic sinus surgical treatment could reduce postoperative recurrence and pain among patients, and showed high efficacy and safety in the treatment of children with chronic sinusitis with nasal polyps.
However, the Meta-analysis in this study is limited due to various confounding factors. In addition, many risk factors and indicators may not be included in the study, which greatly reduces the combined effect. Therefore, follow-up analysis of patients with sinusitis and nasal polyps should be included in future studies to explore the therapeutic effect of endoscopic sinus surgery combined with systemic corticosteroids on chronic sinusitis and nasal polyps in children, so as to improve the results of the meta-analysis.
In conclusion, the results of this meta-analysis provide a theoretical foundation and supportive data for the clinical treatment of rhinosinusitis and other symptoms.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-189/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-189/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- DeConde AS, Mace JC, Levy JM, et al. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope 2017;127:550-5. [Crossref] [PubMed]
- Scangas GA, Wu AW, Ting JY, et al. Cost Utility Analysis of Dupilumab Versus Endoscopic Sinus Surgery for Chronic Rhinosinusitis With Nasal Polyps. Laryngoscope 2021;131:E26-33. [Crossref] [PubMed]
- Zhang L, Zhang Y, Gao Y, et al. Long-term outcomes of different endoscopic sinus surgery in recurrent chronic rhinosinusitis with nasal polyps and asthma. Rhinology 2020;58:126-35. [Crossref] [PubMed]
- Ernst FR, Imhoff RJ, DeConde A, et al. Budget Impact of a Steroid-Eluting Sinus Implant Versus Sinus Surgery for Adult Chronic Sinusitis Patients with Nasal Polyps. J Manag Care Spec Pharm 2019;25:941-950. [Crossref] [PubMed]
- Leggewie B, Gabrielpillai J, Strieth S. Management strategies for chronic rhinosinusitis with nasal polyps. HNO 2022;70:79-86. [Crossref] [PubMed]
- Marioni G, Zanotti C, Brescia G. Chronic rhinosinusitis with nasal polyps in the elderly: Assessing current evidence. Allergy Asthma Proc 2018;39:9-13. [Crossref] [PubMed]
- Veloso-Teles R, Cerejeira R. Endoscopic sinus surgery for chronic rhinosinusitis with nasal polyps: Clinical outcome and predictive factors of recurrence. Am J Rhinol Allergy 2017;31:56-62. [Crossref] [PubMed]
- Miglani A, Divekar RD, Azar A, et al. Revision endoscopic sinus surgery rates by chronic rhinosinusitis subtype. Int Forum Allergy Rhinol 2018;8:1047-51. [Crossref] [PubMed]
- Tong XT, Liu PQ, Zhou HQ, et al. The expression and significance of TRPM8 among chronic rhinosinusitis with nasal polyps. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2021;56:1059-65. [PubMed]
- Yoshida K, Takabayashi T, Imoto Y, et al. Reduced nasal nitric oxide levels in patients with eosinophilic chronic rhinosinusitis. Allergol Int 2019;68:225-32. [Crossref] [PubMed]
- Zhang LC, Sun JW, Li XP, et al. Effect of endoscopic sinus surgery on olfactory function in patients with chronic rhinosinusitis with nasal polyps. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2019;33:713-7. [PubMed]
- Dadgarnia M, Rahmani A, Baradaranfar M, et al. The relationship between endoscopic and radiologic findings and olfactory status of patients with chronic rhinosinusitis with nasal polyps before and after the endoscopic sinus surgery. Eur Arch Otorhinolaryngol 2019;276:397-400. [Crossref] [PubMed]
- Cabrera-Ramírez MS, Domínguez-Sosa MS, Borkoski-Barreiro SA, et al. Analysis and results of endoscopic sinus surgery in chronic rhinosinusitis with polyps. Acta Otorrinolaringol Esp 2017;68:80-5. [Crossref] [PubMed]
- Du K, Huang Z, Si W, et al. Dynamic Change of T-Helper Cell Cytokines in Nasal Secretions and Serum after Endoscopic Sinus Surgery in Chronic Rhinosinusitis with Nasal Polyps. ORL J Otorhinolaryngol Relat Spec 2020;82:74-85. [Crossref] [PubMed]
- Singh A, Luong AU, Fong KJ, et al. Bioabsorbable steroid-releasing implants in the frontal sinus ostia: a pooled analysis. Int Forum Allergy Rhinol 2019;9:131-9. [PubMed]
- Nguyen DT, Guillemin F, Arous F, et al. Assessment of quality-of-life outcomes after surgery for nasal polyposis with the DyNaChron questionnaire. Eur Arch Otorhinolaryngol 2015;272:367-75. [Crossref] [PubMed]
- Smith TL, Singh A, Luong A, et al. Randomized controlled trial of a bioabsorbable steroid-releasing implant in the frontal sinus opening. Laryngoscope 2016;126:2659-64. [Crossref] [PubMed]
- Murr AH, Smith TL, Hwang PH, et al. Safety and efficacy of a novel bioabsorbable, steroid-eluting sinus stent. Int Forum Allergy Rhinol 2011;1:23-32. [Crossref] [PubMed]
- Marple BF, Smith TL, Han JK, et al. Advance II: a prospective, randomized study assessing safety and efficacy of bioabsorbable steroid-releasing sinus implants. Otolaryngol Head Neck Surg 2012;146:1004-11. [Crossref] [PubMed]
- Luong A, Ow RA, Singh A, et al. Safety and Effectiveness of a Bioabsorbable Steroid-Releasing Implant for the Paranasal Sinus Ostia: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg 2018;144:28-35. [PubMed]
- Konstantinidis I, Triaridis S, Printza A, et al. Olfactory dysfunction in nasal polyposis: correlation with computed tomography findings. ORL J Otorhinolaryngol Relat Spec 2007;69:226-32. [Crossref] [PubMed]
- Konstantinidis I, Witt M, Kaidoglou K, et al. Olfactory mucosa in nasal polyposis: implications for FESS outcome. Rhinology 2010;48:47-53. [Crossref] [PubMed]
- Forwith KD, Han JK, Stolovitzky JP, et al. RESOLVE: bioabsorbable steroid-eluting sinus implants for in-office treatment of recurrent sinonasal polyposis after sinus surgery: 6-month outcomes from a randomized, controlled, blinded study. Int Forum Allergy Rhinol 2016;6:573-81. [Crossref] [PubMed]
- Bugten V, Nordgård S, Steinsvåg S. Long-term effects of postoperative measures after sinus surgery. Eur Arch Otorhinolaryngol 2008;265:531-7. [Crossref] [PubMed]
- Adriaensen GFJPM, Lim KH, Fokkens WJ. Safety and efficacy of a bioabsorbable fluticasone propionate-eluting sinus dressing in postoperative management of endoscopic sinus surgery: a randomized clinical trial. Int Forum Allergy Rhinol 2017;7:813-20. [Crossref] [PubMed]
- Lourijsen ES, de Borgie CA, Vleming M, et al. Endoscopic sinus surgery in adult patients with chronic rhinosinusitis with nasal polyps (PolypESS): study protocol for a randomised controlled trial. Trials 2017;18:39. [Crossref] [PubMed]
- Luukkainen A, Seppälä M, Renkonen J, et al. Low lymphatic vessel density associates with chronic rhinosinusitis with nasal polyps. Rhinology 2017;55:181-91. [Crossref] [PubMed]
- Wu Y, Sun Y, Huang Z, et al. The impact of endoscopic sinus surgery on sinonasal microbiome of chronic rhinosinusitis with nasal polyps. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2020;34:1097-102. [PubMed]
- Al Sharhan SS, Al Bar MH, Assiri SY, et al. Pattern of symptom improvement following endoscopic sinus surgery for chronic rhinosinusitis. BMC Surg 2021;21:288. [Crossref] [PubMed]
- Wang J, Shen L, Huang ZQ, et al. Efficacy of buffered hypertonic seawater in different phenotypes of chronic rhinosinusitis with nasal polyps after endoscopic sinus surgery: a randomized double-blind study. Am J Otolaryngol 2020;41:102554. [Crossref] [PubMed]










