
Clinical evaluation of autorefraction and subjective refraction with and without cycloplegia in Chinese school-aged children: a cross-sectional study
Introduction
Refraction, as a routine examination in clinics, is divided into two categories, objective and subjective. Conventional autorefractors can provide spherical, power, and axis of cylinder values, and are a common means for optometrists to obtain objective refraction data due to their convenience and effectiveness. Although it is possible to project the visual target at a distance through an optical system and avoid accommodation through mechanisms such as automated fogging systems, conventional autorefractors will still easily induce accommodation because of proximal accommodation, resulting in the measurement being more myopic. Binocular open field autorefractors can overcome the limitations of conventional autorefractors mentioned above. They can continuously measure the refraction under open field in both eyes, thus effectively reducing proximal accommodation and have shown good reliability and accuracy (1-3).
Previous reports have compared binocular open field autorefractors and conventional autorefractors in patients with and without cycloplegia (4-9), binocular open field autorefractors and subjective refraction (1,2,10), or binocular open field autorefractors and retinoscopy (3,11), as well as comparisons of the results before and after cycloplegia with binocular open field autorefractors (12,13). However, there is a paucity of data comparing binocular open field autorefractor, conventional refractors and subjective refration before and after cycloplegia using Fourier decomposition of the power profile (14). Because these instruments are commonly used, evaluating their agreement for measuring refractive error in school-aged children is important for vision screening, clinical care, and vision research. Therefore, this study compared the results of two autorefractors with the results obtained by subjective refraction in patients with and without cycloplegia. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-226/rc).
Methods
Subjects
A total of 89 patients (177 eyes) who diagnosed as refractive error in Affiliated Hospital of Nanjing University of Chinese Medicine from July 2020 to September 2020, including 47 males and 42 females, aged 11.67±3.31 (range, 6–18) years, were sequentially enrolled in this cross-sectional study. The number of cases in the area during the study period determined the sample size. All subjects underwent routine ophthalmic examination to exclude other ocular diseases and had a best corrected visual acuity no less than 0.1. Visual acuity measurements at 4 m used a retro-illuminated log minimum angle of resolution (logMAR) chart with tumbling-E target (Chicago, IL, USA). All contact lenses were removed prior to obtaining measurements. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Affiliated Hospital of Nanjing University of Chinese Medicine (No. 2020NL-128-02). Informed consent was taken from their parents or legal guardians.
Apparatus
- A conventional autorefractor, TOPCON KR3000 (Topcon, Japan), hereinafter referred to as the TOPCON autorefractor, was used. This autorefractor uses a closed-view format, having an internal fixation target, infrared light source, and automatic fogging device to relax accommodation. The subjects were asked to fixate their gaze on the target monocular inside the autorefractor during testing.
- The binocular open field autorefractor WAM-5500 (Seiko, Japan), hereinafter referred to as the WAM autorefractor, has two measurement modes, dynamic and static. Under the static mode each measurement is similar to that of a conventional autorefractor. The dynamic mode enables continuous high-frequency (5 Hz) measurement of the spherical equivalence (SE) and pupil diameter. During testing, the subjects were requested to look at the standard at a distance of 6 m in both eyes (naked eye) [20/30, Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity chart]. Measurements were taken using the static mode.
Procedure
- Sequence of examination: all subjects were examined in the following order: (i) autorefraction with WAM; (ii) autorefraction with TOPCON; (iii) cycloplegia; (iv) autorefraction with WAM; (v) autorefraction with TOPCON; and (vi) routine subjective refraction. Measurements of the right eye were performed first, followed by measurements of the left eye. Three consecutive measurements were taken with each autorefractor by two different experienced optometrists (WQJ and MX). Autorefraction after cycloplegia was then performed. Subjective refraction at a distance was performed using phoropter (Nidek, Japan) by another experienced optometrist (WH).
- Cycloplegia: cycloplegia was induced with tropicamide eye drops (5 mg/mL; Tianjin, China) every 5 minutes for 6 cycles. Autorefraction was performed 20 to 25 minutes following the final instillation.
Data processing and statistical methods
All prescription readings were recorded in negative cylindrical form. The refractive status of each eye (spherical, cylindrical power, cylindrical axis) was recorded. The mean SE was calculated as follows: mean SE = sphere + (cylinder/2).
Cycloplegia subjective refraction results were regarded as the gold standard for measuring refractive status in children. There were difficulties assessing the variance in the astigmatic component in the conventional clinical notation. Therefore the sphere, cylinder, and axis components were converted into a vector representation (14) as follows: J0 represents the axial 0°/180° [J0 = (−C/2) × cos2β], representing with/against the rule of astigmatism; J45 represents the axial 45°/135° [J45 = (−C/2) × sin2β] (β for astigmatism axial), representing the oblique axis of astigmatism.
SE ≥−0.50 D is defined as emmetropia and hyperopia; −3.00 D ≤ SE <−0.50 D is defined as mild myopia; −6.00 D ≤ SE <−3.00 D is defined as moderate myopia; and SE <−6.00 D is defined as high myopia.
Data before and after cycloplegia were calculated using SPSS 17.0 software (IBM, USA). The coincidence rate of spherical diopter (SD), SE, and cylindrical power (defined as the difference of diopter ≤0.50 D), and the cylindrical axis (defined as difference of degree ≤20°) were evaluated. Distribution was described according to the difference of the mean SE of the two autorefractors before and after cycloplegia, respectively. A comparison of data in different measurements was performed using paired t-tests and presented graphically using Bland-Altman plots (15). The intraclass correlation coefficient (ICC) was calculated to analyze the consistency of the three measurements. A P value of less than 0.05 was considered statistically significant.
Results
All 89 subjects completed the study.
Coincidence of WAM and TOPCON results
The coincidence of SD, SE, and cylindrical power, as well as the cylindrical axis results measured by the two autorefractors were compared with those measured by subjective refraction, with and without cycloplegia (Table 1). Under non-cycloplegia conditions, the coincidence of the WAM measurements was slightly higher than that of the TOPCON measurements in the SD and SE parameters, whereas the WAM measurements were slightly lower in the astigmatism parameters. However, the coincidence of each parameter of the two autorefractors obviously improved after cycloplegia and the overall coincidence of the TOPCON autorefractor was higher than that of the WAM autorefractor.
Table 1
| Status | Eye | Group | Coincidence, n (%) | |||
|---|---|---|---|---|---|---|
| SD | SE | Cylindrical power | Cylindrical axis | |||
| Before cycloplegia | 177 | WAM | 133 (75.1) | 130 (73.4) | 144 (81.4) | 160 (90.4) |
| TOPCON | 131 (74.0) | 118 (66.7) | 162 (91.5) | 172 (97.2) | ||
| After cycloplegia | 177 | WAM | 152 (85.9) | 154 (87.0) | 144 (81.4) | 167 (94.4) |
| TOPCON | 172 (97.2) | 167 (94.4) | 166 (93.8) | 176 (99.4) | ||
SD, spherical diopter; SE, spherical equivalence.
The subjects were divided by SE results after cycloplegia, with 39 subjects in the emmetropic and hyperopic group, 94 in the mild myopic group, 37 in the moderate myopic group, and 7 in the high myopia group. The distribution of the difference between the two autorefractors (TOPCON-WAM) within 0.25 D was significantly enhanced with cycloplegia compared to before cycloplegia in all groups (Table 2).
Table 2
| Group | Eye | Difference of SE before cycloplegia, % [n] | Difference of SE after cycloplegia, % [n] | |||||
|---|---|---|---|---|---|---|---|---|
| >+0.25 D | −0.25 D to +0.25 D | <−0.25 D | >+0.25 D | −0.25 D to +0.25 D | <−0.25 D | |||
| Emmetropia and hyperopia | 39 | 30.8% [12] | 38.5% [15] | 30.8% [12] | 25.6% [10] | 56.4% [22] | 17.9% [7] | |
| Low myopia | 94 | 8.5% [8] | 38.3% [36] | 53.2% [50] | 5.3% [5] | 56.4% [53] | 38.3% [36] | |
| Moderate myopia | 37 | 13.5% [5] | 37.8% [14] | 48.6% [18] | 5.4% [2] | 51.4% [19] | 43.2% [16] | |
| High myopia | 7 | 28.6% [2] | 28.6% [2] | 42.9% [3] | 14.3% [1] | 85.7% [6] | 0.0% [0] | |
| Total | 177 | 15.3% [27] | 37.9% [67] | 46.8% [83] | 10.2% [18] | 56.5% [100] | 33.3% [27] | |
SE, spherical equivalence; D, diopter.
The ICC values between the different examination methods with and without cycloplegia are shown in Tables 3,4.
Table 3
| Group | SD | SE | J0 | J45 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | ||||
| WAM vs. TOPCON | 0.958 | 0.944–0.968 | 0.960 | 0.946–0.970 | 0.896 | 0.863–0.922 | 0.605 | 0.503–0.691 | |||
| WAM vs. subjective refraction | 0.952 | 0.935–0.964 | 0.953 | 0.937–0.965 | 0.886 | 0.849–0.914 | 0.645 | 0.550–0.723 | |||
| TOPCON vs. subjective refraction | 0.986 | 0.981–0.989 | 0.986 | 0.981–0.990 | 0.952 | 0.936–0.964 | 0.742 | 0.668–0.802 | |||
ICC, intraclass correlation coefficient; SD, spherical diopter; SE, spherical equivalence; J0, the axial 0°/180° representing with/against the rule of astigmatism; J45, the axial 45°/135° representing the oblique axis of astigmatism; CI, confidence interval.
Table 4
| Group | SD | SE | J0 | J45 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95%CI | ICC | 95% CI | ICC | 95% CI | ||||
| WAM vs. TOPCON | 0.983 | 0.977–0.987 | 0.986 | 0.981–0.989 | 0.907 | 0.877–0.930 | 0.589 | 0.484–0.678 | |||
| WAM vs. subjective refraction | 0.983 | 0.977–0.987 | 0.986 | 0.982–0.990 | 0.895 | 0.862–0.921 | 0.501 | 0.382–0.604 | |||
| TOPCON vs. subjective refraction | 0.993 | 0.991–0.995 | 0.994 | 0.992–0.995 | 0.963 | 0.950–0.972 | 0.656 | 0.563–0.732 | |||
ICC, intraclass correlation coefficient; SD, spherical diopter; SE, spherical equivalence; J0, the axial 0°/180° representing with/against the rule of astigmatism; J45, the axial 45°/135° representing the oblique axis of astigmatism; CI, confidence interval.
A comparison of WAM and TOPCON before and after cycloplegia
The results measured by WAM and TOPCON before cycloplegia is shown in Table 5. There was high correlation and agreement in the SD, SE, and J0 readings between WAM and TOPCON, with correlation coefficient values of 0.958, 0.960, and 0.900, and ICC values of 0.958, 0.960, and 0.896, respectively. The correlation coefficients and ICC values of J45 were somewhat lower, with R=0.606 and ICC =0.605, respectively. Scatter plots and Bland-Altman scatter plots for comparison of each parameter are shown in Figures 1,2. Further comparison showed that the SD results measured by WAM were more positive than those obtained by TOPCON (t=2.578, P=0.011), and there was also a similar trend in SE (t=2.329, P=0.021). However, there were no significant differences in the J0 and J45 results (P=0.172 and P=0.156, respectively).
Table 5
| Group | SD (D) | SE (D) | J0 (D) | J45 (D) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | P | 95% CI | P | 95% CI | P | 95% CI | P | ||||||||
| WAM vs. TOPCON | 0.011* | 0.021* | 0.172 | 0.156 | |||||||||||
| WAM | −1.607±2.474 | −1.974 to −1.240 | −2.142±2.563 | −2.522 to −1.762 | 0.456±0.497 | 0.383 to 0.530 | −0.009±0.191 | −0.037 to 0.020 | |||||||
| TOPCON | −1.749±2.551 | −2.127 to −1.370 | −2.272±2.668 | −2.668 to −1.876 | 0.481±0.542 | 0.400 to 0.561 | −0.027±0.198 | −0.057 to 0.002 | |||||||
| WAM vs. subjective refraction | <0.001* | <0.001* | 0.834 | 0.207 | |||||||||||
| WAM | −1.607±2.474 | −1.974 to −1.240 | −2.142±2.563 | −2.522 to −1.762 | 0.456±0.497 | 0.383 to 0.530 | −0.009±0.191 | −0.037 to 0.020 | |||||||
| Subjective refraction | −1.297±2.608 | −1.684 to −0.910 | −1.778±2.694 | −2.177 to −1.378 | 0.460±0.518 | 0.383 to 0.537 | −0.023±0.171 | −0.049 to 0.002 | |||||||
| TOPCON vs. subjective refraction | <0.001* | <0.001* | 0.098 | 0.693 | |||||||||||
| TOPCON | −1.749±2.551 | −2.127 to −1.370 | −2.272±2.668 | −2.668 to −1.876 | 0.481±0.542 | 0.400 to 0.561 | −0.027±0.198 | −0.056 to 0.002 | |||||||
| Subjective refraction | −1.297±2.608 | −1.684 to −0.910 | −1.778±2.694 | −2.177 to −1.378 | 0.460±0.518 | 0.383 to 0.537 | −0.023±0.171 | −0.049 to 0.002 | |||||||
*, P<0.05 was considered statistically significant. SD, spherical diopter; SE, spherical equivalence; J0, the axial 0°/180° representing with/against the rule of astigmatism; J45, the axial 45°/135° representing the oblique axis of astigmatism; , mean ± standard deviation; CI, confidence interval; D, diopter.

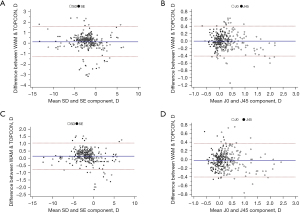
The results measured by WAM and TOPCON after cycloplegia is shown in Table 6. There was high correlation and agreement in the SD, SE, and J0 results between WAM and TOPCON, with correlation coefficients of 0.984, 0.986, and 0.909, and ICC values of 0.983, 0.986, and 0.907, respectively. The correlation coefficient and ICC value of J45 were somewhat lower, with R=0.591 and ICC =0.589, respectively. Scatter plots and Bland-Altman scatter plots for comparison of each parameter are shown in Figures 1,2. Further comparison showed that the SD and SE results measured by WAM were more positive than those obtained by TOPCON (t=3.672, P<0.001; t=3.583, P<0.001), while there was no significant difference in the J0 and J45 results (P=0.262 and P=0.122, respectively).
Table 6
| Group | SD (D) | SE (D) | J0 (D) | J45 (D) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | P | 95% CI | P | 95% CI | P | 95% CI | P | ||||||||
| WAM vs. TOPCON | <0.001* | <0.001* | 0.262 | 0.122 | |||||||||||
| WAM | −1.250±2.556 | −1.629 to −0.871 | −1.795±2.656 | −2.189 to −1.401 | 0.475±0.494 | 0.402 to 0.548 | −0.038±0.194 | −0.066 to −0.009 | |||||||
| TOPCON | −1.382±2.646 | −1.774 to −0.989 | −1.919±2.733 | −2.324 to −1.513 | 0.494±0.530 | 0.415 to 0.572 | −0.018±0.179 | −0.044 to 0.009 | |||||||
| WAM vs. subjective refraction | 0.197 | 0.595 | 0.391 | 0.291 | |||||||||||
| WAM | −1.250±2.556 | −1.629 to −0.871 | −1.795±2.656 | −2.189 to −1.401 | 0.475±0.494 | 0.402 to 0.548 | −0.038±0.194 | −0.066 to −0.009 | |||||||
| Subjective refraction | −1.297±2.608 | −1.684 to −0.910 | −1.778±2.694 | −2.177 to −1.378 | 0.460±0.518 | 0.383 to 0.537 | −0.023±0.171 | −0.049 to 0.002 | |||||||
| TOPCON vs. subjective refraction | <0.001* | <0.001* | 0.002* | 0.635 | |||||||||||
| TOPCON | −1.382±2.646 | −1.774 to −0.989 | −1.919±2.733 | −2.324 to −1.513 | 0.494±0.530 | 0.415 to 0.572 | −0.018±0.179 | −0.044 to 0.009 | |||||||
| Subjective refraction | −1.297±2.608 | −1.684 to −0.910 | −1.778±2.694 | −2.177 to −1.378 | 0.460±0.518 | 0.383 to 0.537 | −0.023±0.171 | −0.049 to 0.002 | |||||||
*P<0.05 was considered statistically significant. SD, spherical diopter; SE, spherical equivalence; J0, the axial 0°/180° representing with/against the rule of astigmatism; J45, the axial 45°/135° representing the oblique axis of astigmatism; , mean ± standard deviation; CI, confidence interval; D, diopter.
A comparison of WAM and TOPCON before cycloplegia and subjective refraction after cycloplegia
The correlation and agreement of the SD, SE, and J0 results between WAM before cycloplegia and subjective refraction after cycloplegia was extremely high, with correlation coefficients of 0.953, 0.954, and 0.886, and ICC values of 0.952, 0.953, and 0.886, respectively. However, the correlation coefficient and ICC value of J45 were somewhat lower, with R=0.648 and ICC =0.645, respectively. Scatter plots and Bland-Altman scatter plots for comparison of each parameter are shown in Figures 3,4.

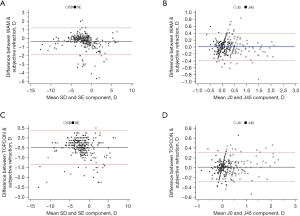
The correlation and agreement of the SD, SE, and J0 results between Topcon before cycloplegia and subjective refraction after cycloplegia were extremely high, with correlation coefficients of 0.986, 0.986, and 0.953, and ICC values of 0.986, 0.986, 0.952, respectively. Interestingly, the correlation coefficient and ICC value of J45 were somewhat lower, with R=0.750 and ICC =0.742, respectively. Scatter plots and Bland-Altman scatter plots for comparison of each parameter are shown in Figures 3,4.
Further comparison found that the SD of WAM and TOPCON before cycloplegia were both more negative than that of subjective refraction after cycloplegia (t=−5.219, P<0.001; t=−13.873, P<0.001). There was a similar trend for SE (t=−6.005, P<0.001; t=−14.739, P<0.001). However, neither the J0 results nor the J45 results showed any statistical difference (P=0.834 and P=0.098, and P=0.207 and P=0.693, respectively).
A comparison of the WAM, TOPCON, and subjective refraction results after cycloplegia
The results of the refractive parameters for WAM, TOPCON, and subjective refraction after cycloplegia is shown in Table 6.
The correlation coefficients of the SD, SE, and J0 results between WAM and subjective refraction were 0.983, 0.986, and 0.896, respectively, and the ICC values were 0.983, 0.986, and 0.895, respectively, while the correlation coefficient and ICC value of J45 were somewhat lower, with R=0.505 and ICC =0.501.
The correlation coefficients of the SD, SE, and J0 results between WAM and subjective refraction were 0.994, 0.994, and 0.963, respectively, and the ICC values were 0.993, 0.994, and 0.963, respectively, while the correlation coefficient and ICC value of J45 were somewhat lower, with R=0.656 and ICC =0.656. Scatter plots and Bland-Altman scatter plots for comparison of each parameter are shown in Figures 5,6.

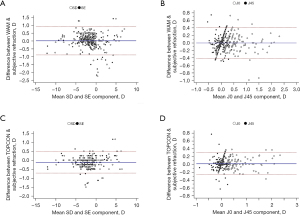
There were no statistically significant differences between WAM and subjective refraction after cycloplegia in SD, SE, J0, nor J45 results (P=0.197, P=0.595, P=0.391, and P=0.291, respectively). The SD, SE, and J0 results of TOPCON were significantly different from those of subjective refraction (t=−3.774, P<0.001; t=−6.158, P<0.001; and t=3.125, P=0.002, respectively), while the J45 results were not significantly different (P=0.635).
Discussion
The clinic practice of prescription in juvenile myopia involves subjective refraction based on static retinoscopy or autorefraction results after cycloplegia and the use of trial frames after pupil recovery. However, cycloplegia may cause many inconveniences to patients. Open field autorefractors can reduce near perceptual accommodation and prevent myopic overcorrection due to the simultaneous gaze in both eyes and the open field design. It is widely used as a screening method in myopic children (16) and accommodative response measurements (17,18). However, it is debatable whether the results of open field autorefractor are reliable enough to use directly in prescription glasses. This study investigated two different computerized autorefractors and subjective refraction before and after cycloplegia, so as to evaluate the accuracy and reliability of each method. The data herein demonstrated that the WAM-5500 autorefractor was more reliable than the TOPCON KR-3000 autorefractor, both before and after cycloplegia. However results of both autorefractors cannot completely substitute cycloplegia refraction in school-aged children.
The coincidence rate of WAM and TOPCON before and after cycloplegia showed the following: (I) the coincidence rate with subjective refraction was enhanced after cycloplegia, especially with TOPCON; and (II) the distribution of the difference between the two autorefractors (TOPCON-WAM) within 0.25 D was significantly enhanced with cycloplegia compared to before cycloplegia in all groups. The above-mentioned trends are most likely caused by cycloplegia decreasing the accommodation and closer to the actual results, as suggested by previous report (5). Furthermore, the SD and SE results of WAM before cycloplegia were more reliable, which may be attributed to the binocular open field design being more effective at reducing the influence of accommodation compared to conventional autorefractors based on the principle of monocular fogging (19,20). However, the accuracy of both autorefractors require further improvement. The results of the cylindrical power and axial measurements obtained with TOPCON were more accurately than those measured by WAM before and after cycloplegia.
The ICC is used to show consistency between measurements and ranges from 0 to 1. Generally, an ICC value <0.2 indicates poor consistency; 0.2–0.4 illustrates low levels of consistency; 0.4–0.6 demonstrates a moderate level of consistency; and 0.6–0.8 represents high levels of consistency. A strong degree of consistency is demonstrated by ICC values ranging from 0.8 to 1.0. The SD, SE, and J0 values of both autorefractors and subjective refraction had extremely high correlation (R>0.8) and agreement (ICC >0.8), both before and after cycloplegia. However, J45 had significantly lower correlation and coincidence values, indicating a higher correlation and coincidence among the three different examination methods for spherical with the rule/against the rule astigmatism data, but poor correlation and coincidence for oblique astigmatism data, which were generally consistent with results reported by Kuo et al. (11).
Previous studies have demonstrated that both WAM and TOPCON can be applied to visual acuity screening in a large Chinese population, with WAM performing better in school-aged children (7). Tsuneyoshi et al. (19) showed that WAM improved instrumental myopic shift more significantly than conventional autorefractors, with a SE difference of 0.51±0.33 D. However, this difference decreased with age, which was similarly reported by Gwiazda et al. (21). In our study, before cycloplegia, the SD and SE results obtained by WAM were more positive than those obtained by TOPCON, by 0.14 D and 0.12 D, respectively (t=2.578, P=0.011; t=2.329, P=0.021). These results suggested that WAM can relax accommodation more efficiently than TOPCON. However, as the difference was not great, it is unlikely to have any clinical significance. The difference in SD and SE values measured with and without cycloplegia by WAM was both 0.35 D, similar to the study of Gopalakrishnan et al. (12). Reports by Nagra et al. (9) and Queirós et al. (13) reported that SE differences measured by WAM with and without cycloplegia were 0.28 D and 0.23 D, respectively, which were both smaller than the results observed in this present study. This may be due to their subjects being adults, with relatively less active accommodation compared to children.
The SD results measured by WAM and TOPCON before cycloplegia were both significantly more negative than subjective refraction post cycloplegia, with differences of 0.31 D and 0.45 D, respectively (t=−5.219, P<0.001; and t=−13.873, P<0.001, respectively). There was a similar trend in the SE results (t=−6.005, P<0.001; and t=−14.739, P<0.001, respectively). This demonstrated an inability to remove the influence of accommodation in both autorefractors. Therefore, neither autorefractor can completely substitute cycloplegia refraction. This was consistent with the results of Kara et al. (22), with the exception that their subjects were mainly children aged 3–6 years. The age span was more fragmented and the refractive distribution was also relatively skewed towards myopia. The study by Davies and colleagues (2) reported that the SE difference between WAM and subjective refraction was 0.14 D, which is lower than that in the present study. This may be due to the adult study population with relatively less active accommodation and the absence of cycloplegia in their study.
The SD and SE results obtained by WAM were 0.13 D and 0.12 D more positive than those obtained by TOPCON after cycloplegia, respectively (t=3.672, P<0.001; t=3.583, P<0.001, respectively). This indicated that even after cycloplegia, the WAM results were still more positive than the TOPCON results, which was consistent with the report by Ying and colleagues (6). Most of the subjects in the latter study were African American hyperopic children aged 4–5 years, and the results were not compared to the TOPCON autorefractor but to the hand-held Retinomax refractor, which is inherently more myopic than table mounted refractors (23). There were no statistically significant differences between the results obtain by WAM and subjective refraction in SD, SE, J0, and J45 parameters (P=0.197, P=0.595, P=0.391, and P=0.291, respectively). However, the SD, SE, and J0 results obtained by TOPCON were significantly different from those obtained by subjective refraction (t=−3.774, P<0.001; t=−6.158, P<0.001; t=3.125, P=0.002), suggesting that even after cycloplegia, the results of WAM were more accurate and reliable than TOPCON. However, for the coincidence rate, TOPCON results were high than WAM after cycloplegia. It may because the difference standard was set as 0.50 D which caused some error.
There were several limitations to this study. The sample size was relatively small and subjects with different refractive status and types of astigmatism were excluded. With the exception of the coincidence rate, none of the other parameters measured classified the subjects by diopter. It is possible that the accuracy of the results may correlate with the refractive status and further studies should be conducted.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-226/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-226/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-226/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Affiliated Hospital of Nanjing University of Chinese Medicine (No. 2020NL-128-02). Informed consent was taken from their parents or legal guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sheppard AL, Davies LN. Clinical evaluation of the Grand Seiko Auto Ref/Keratometer WAM-5500. Ophthalmic Physiol Opt 2010;30:143-51. [Crossref] [PubMed]
- Davies LN, Mallen EA, Wolffsohn JS, et al. Clinical evaluation of the Shin-Nippon NVision-K 5001/Grand Seiko WR-5100K autorefractor. Optom Vis Sci 2003;80:320-4. [Crossref] [PubMed]
- Qi LS, Yao L, Zhao J, et al. Comparison of objective refraction by open-field auto-refractor to conventional cycloplegic retinoscopy in teenagers with low ametropia. Academic Journal of Chinese Pla Medical School 2018;39:384-7.
- Rosenfield M, Ciuffreda KJ. Evaluation of the SVOne Handheld Autorefractor in a Pediatric Population. Optom Vis Sci 2017;94:159-65. [Crossref] [PubMed]
- Wan XH, Lin Z, Cai XG, et al. Comparison between binocular, open-field auto ref/keratometer and conventional autorefractor. Zhonghua Yan Ke Za Zhi 2012;48:519-23. [PubMed]
- Ying GS, Maguire MG, Kulp MT, et al. Comparison of cycloplegic refraction between Grand Seiko autorefractor and Retinomax autorefractor in the Vision in Preschoolers-Hyperopia in Preschoolers (VIP-HIP) Study. J AAPOS 2017;21:219-23.e3. [Crossref] [PubMed]
- Wang D, Jin N, Pei RX, et al. Comparison between two autorefractor performances in large scale vision screening in Chinese school age children. Int J Ophthalmol 2020;13:1660-6. [Crossref] [PubMed]
- Satou T, Takahashi Y, Niida T. Comparison of refractive value and pupil size under monocular and binocular conditions between the Spot Vision Screener and binocular open-field autorefractor. Strabismus 2020;28:186-93. [Crossref] [PubMed]
- Nagra M, Akhtar A, Huntjens B, et al. Open versus closed view autorefraction in young adults. J Optom 2021;14:86-91. [Crossref] [PubMed]
- Choong YF, Chen AH, Goh PP. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am J Ophthalmol 2006;142:68-74. [Crossref] [PubMed]
- Kuo YC, Wang JH, Chiu CJ. Comparison of open-field autorefraction, closed-field autorefraction, and retinoscopy for refractive measurements of children and adolescents in Taiwan. J Formos Med Assoc 2020;119:1251-8. [Crossref] [PubMed]
- Gopalakrishnan A, Hussaindeen JR, Sivaraman V, et al. The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study-Defining a Threshold for Non-Cycloplegic Myopia Prevalence in Children. J Clin Med 2021;10:1215. [Crossref] [PubMed]
- Queirós A, González-Méijome J, Jorge J. Influence of fogging lenses and cycloplegia on open-field automatic refraction. Ophthalmic Physiol Opt 2008;28:387-92. [Crossref] [PubMed]
- Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci 1997;74:367-75. [Crossref] [PubMed]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307-10. [Crossref] [PubMed]
- Gopalakrishnan A, Hussaindeen JR, Sivaraman V, et al. Prevalence of myopia among urban and suburban school children in Tamil Nadu, South India: findings from the Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study. Ophthalmic Physiol Opt 2022;42:345-57. [Crossref] [PubMed]
- Ortiz-Peregrina S, Ortiz C, Martino F, et al. Dynamics of the accommodative response after smoking cannabis. Ophthalmic Physiol Opt 2021;41:1097-109. [Crossref] [PubMed]
- Redondo B, Vera J, Molina R, et al. Less is more: optimal recording time for measuring the steady-state accommodative response. Clin Exp Optom 2021; Epub ahead of print. [Crossref] [PubMed]
- Tsuneyoshi Y, Negishi K, Tsubota K. Importance of Accommodation and Eye Dominance for Measuring Objective Refractions. Am J Ophthalmol 2017;177:69-76. [Crossref] [PubMed]
- Kobashi H, Kamiya K, Handa T, et al. Comparison of Subjective Refraction under Binocular and Monocular Conditions in Myopic Subjects. Sci Rep 2015;5:12606. [Crossref] [PubMed]
- Gwiazda J, Weber C. Comparison of spherical equivalent refraction and astigmatism measured with three different models of autorefractors. Optom Vis Sci 2004;81:56-61. [Crossref] [PubMed]
- Kara C, Petriçli İS. Inability of Open-Field Autorefraction to Eliminate Accommodation in Preschoolers. J Pediatr Ophthalmol Strabismus 2017;54:311-8. [Crossref] [PubMed]
- Farook M, Venkatramani J, Gazzard G, et al. Comparisons of the handheld autorefractor, table-mounted autorefractor, and subjective refraction in Singapore adults. Optom Vis Sci 2005;82:1066-70. [Crossref] [PubMed]


