
Novel TTC37 mutations in a patient with Trichohepatoenteric syndrome: a case report and literature review
Introduction
Trichohepatoenteric syndrome (THES) is a rare autosomal recessive genetic enteropathy with a global incidence estimated at 1/1,000,000 births; it is also known as phenotypic diarrhea and syndromic diarrhea (1). The main features include intractable diarrhea, woolly hair abnormality, immune dysfunction, intrauterine growth restriction (IUGR), facial dysmorphism, and sometimes liver and skin abnormalities. However, the spectrum of symptoms is broad, and patients do not always present with all the main features. Intractable diarrhea usually occurs in the first days of life, but sometimes it can occur later in life (2). Some patients require life-long parenteral nutrition for survival, while others could be weaned to full enteral feeding (3). However, THES with immunodeficiency presenting without diarrhea has also been reported (4). Mild intellectual disability is seen in almost 50% of affected individuals, which may be caused either by THES itself or secondary to malnutrition caused by THES (5). Additional less common and consistent findings include congenital cardiac abnormalities and platelet dysfunction (5).
The molecular basis of THES has been investigated. Tetratricopeptide repeat domain-containing protein 37 (TTC37) and super killer viralicidic activity 2 (SKIV2L), which both encode proteins involved in RNA processing and degradation, have been identified as causative gene of THES. The occurrence of mutations in TTC37 gene on chromosome 5, as the cause of two-thirds of THES cases, was defined as THES syndrome 1 (OMIM, #222470; *614589) in early 2010 (6). THES was first described by Stankler et al. in 1982 (7). To date, less than 100 affected individuals and more than 50 TTC37 mutations have been described (5,6,8). Although four Chinese children affected with THES syndrome 1 have been described in Singapore, Taiwan (China) and Malaysia, to our knowledge, this is the first report of a patient with THES in Mainland China, harboring classical features, clinical course, and novel mutations in TTC37 gene (9-12). In addition to intractable diarrhea, woolly hair abnormality and fair skin, the infant presented with mild platelet abnormality and intractable hypoglycemia. This case extends the known broad clinical phenotype of THES. We present the following article in accordance with the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-21-574/rc).
Case presentation
A male infant from Chinese mainland was born at 37+1 weeks of gestation with a birth weight of 1,480 g (< third percentile) by emergent cesarean section due to intrauterine fetal distress. His head circumference was 29.5 cm (< third percentile), and his height was 37.4 cm (< third percentile). As shown in Figure 1, he had minor dysmorphic features with a wide and prominent forehead, prominent ears and cheeks, fair skin, and curly and hypopigmented hair. He was the first-born child to non-consanguineous parents with no significant family history. The 1 min and 5 min Apgar scores were 7 and 9, respectively. The amniotic fluid, placenta, and umbilical cord were normal. The infant was admitted to neonatal intensive care unit due to his low birth weight. His mother was healthy but experienced hyperemesis gravidarum throughout the pregnancy. The antenatal examination was followed regularly, and all results were normal except for ultrasound evidence of IUGR from 21+3 weeks of pregnancy. At 11 days of age, the infant achieved full enteral nutrition (preterm formula: 156 mL/kg/day). However, on the next day, he experienced vomiting, abdominal distention, and inappetence. After halving the formula feeding volume, the feeding status improved. At 20 days of age, the feeding volume achieved 164 mL/kg/day, but the fasting blood glucose level was only 3.4 mmol/L. On the following day, he presented fever, watery diarrhea, abdominal distention, and inappetence. Metabolic disorders were excluded by tandem mass spectrometry, urine-blood amino acids analysis. After switching to total parenteral nutrition and cessation of feeding for 3 days, diarrhea improved. The proportion of eosinophils in the blood was up to 17.6% (0.5–5.0%), the elevated eosinophil count was 4.31×109/L (0.2–2.0×109/L). Considering elevated eosinophils indicate hypersensitivity, amino acid-based formula was started at 24 days of age. After 8 days of feeding with amino acid-based formula, watery diarrhea again appeared, and it was accompanied with hypoglycemia. From then on, even slightly hypotonic oral rehydration solutions aggravated watery diarrhea. Liver enzymes and abdominal ultrasound including liver, spleen, and pancreas were normal. At 46 days of age, the blood glucose level was as low as 2.7 mmol/L, even when the glucose infusion rate was up to 14 mg/kg/min on the parenteral alone. At the same time, the insulin level was 1.4 µIU/mL and the infant got adequate weight gain with total parenteral nutrition. The levels of growth hormone, insulin-like growth factor 1, cortisol, adrenocorticotropic hormone, creatine kinase, thyroid hormones were normal. Additionally, metabolic diseases were ruled out according to tandem mass spectrometry and urine-blood amino acids analysis. Hydrocortisone (1 mg/kg/dose, every 4 hours) was used to maintain blood glucose levels until he was discharged (for 4 days). In view of the above, we speculated the hypoglycemia might be associated with THES. The whole-exome sequencing analysis identified compound heterozygous mutations (c.4130C > G: p.S1377X) and (Exon11-13 del) in the TTC37 gene, which had been inherited from his father and mother, respectively (Figure 2).
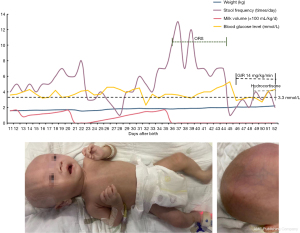
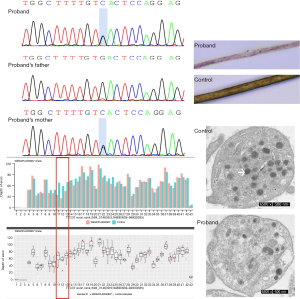
Throughout the hospital stay, there was no infection. Lymphocyte subpopulations analysis (CD3+CD19−, CD3−CD19+, CD3+CD4+, CD3+CD8+, CD3−/CD16+CD56+) showed normal cellular proportions. Immunoglobulin levels detection showed hypogammaglobulinemia of IgG [1.1 g/L, (6.6–17.5)]. Platelet size and aggregation responses to ADP (100 µmol/L) were normal, but the membrane surface-connected canalicular system was disrupted in the thin-section transmission electron microscopy images (Figure 2). The number of normal α-granules was reduced significantly in THES platelets compared to control platelets (4±2 α-granules/platelet vs. 10±3 α-granules/platelet section, P<0.05). We did not observe any lipid inclusions or electron-dense lysosomal bodies fused with an α-granules in our case. Light microscopy of hair showed decreased hair shaft pigmentation but no trichorrhexis nodosa. The parents refused intestinal biopsy, so intestinal tissue was not inspected. The infant had global developmental delay, but the neonatal behavioral neurological assessment was normal. At 52 days of age, after confirmation of the diagnosis, he was discharged from the hospital according to his parents’ wishes. At that time, his weight was 2,200 g (<third percentile), his head circumference was 34.0 cm (<third percentile), and his height was 44.5 cm (<third percentile). Then, he was fed breast milk at home with persistent liquid stools. We learned of his death at home without venous access at 4 months of age during a follow-up phone call.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardians for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Clinical heterogeneity of THES makes the diagnosis challenging. Although the acronym THES includes trichomes, hepatitis, and enteritis, any of these features may lack or evolve with time (2). Whole-exome sequencing analysis should be considered to guide treatment, prognosis, and genetic counseling. The management mainly involves chronic administration of parenteral nutrition and immunoglobulin supplementation. Immunosuppressive medications and steroids are not recommended (8). In our case report, diarrhea was not improved by steroids therapy. Since the stem cell transplantation resolved the immune defect but not the other features, it is also not recommended (8). The prognosis is mainly dependent on the immune status, the severity of diarrhea, and the need for long-term parenteral nutrition.
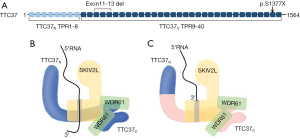
The protein coded by TTC37 gene containing tetratrico peptide repeat domains is a component of superkiller (SKI) complex involved in exosome-mediated RNA surveillance including the regulation of normal mRNA and decay of nonfunctional mRNA (Figure 3). Pathogenic variants of TTC37 can reduce protein expression or alter protein function, subsequently inducing loss of function of SKI complex (13). SKI complex is expressed at different levels in different cell types/tissues; therefore, TTC37 has multisystem effect and could affect one cell type/tissue more than another. However, the underlying mechanism by which mRNA surveillance defects lead to the symptoms associated with THES in multiple systems remains unclear. We detected two novel mutations in our patient, which were both loss-of-function mutations. The mutation (exon 39, c.4130C > G) is predicted to be “disease_causing_automatic” by MutationTaster_pred. Insertion and missense mutations in exon 40–42 in the TTC37 gene have been reported to be pathogenic mutations (6). The nonsense mutation (exon 39, c.4130C > G) is presumably devastating to the protein structure by leading to the creation of a premature stop codon and a truncated and nonfunctional peptide chain (Figure 3). The loss of exon 11-13 in our case was in frame. Given that the exon 12 is related to tetratricopeptide repeat domains as reported in previous literature (14), the change of an amino acid due to deletion mutation (Exon11-13 del) in TTC37 gene may result in the production of abnormal tetratricopeptide repeat domains.
Almost all patients with THES caused by mutations in TTC37 gene had growth retardation (intrauterine growth retardation or extrauterine failure to thrive), facial dysmorphy (especially prominent forehead) and hair abnormalities (trichorrhexis nodosa, or woolly/curly/brittle hair) (15). Approximately half of the patients presented skin abnormalities (especially cafe’ au lait spots) and mild intellectual disability. The expression level of TTC37 mRNA is high in the intestines and pathogenic variants of TTC37 gene disturb RNA exosome to affect the localization of apical transport proteins, thereby almost all patients presented intractable diarrhea (14). Only a small percentage of patients reach normal oral nutrition after many years of total parenteral nutrition. However, intestinal biopsy of all reported patients to date has suggested nonspecific villous atrophy. About 50% of the patients had abnormalities in liver biochemistry or ultrasonic appearance (10,16). Although the expression level of TTC37 in the liver is much lower than that in other tissues, hepatic dysfunction was observed irrespective of parenteral nutrition, even before the onset of diarrhea (14). In addition, immunity impairment is another common feature of THES. About 50% of reported patients presented low serum concentration of immunoglobulins or lack of humoral immune responses to immunization, although they had normal leukocyte and differential cell counts (6). The pathogenesis might be attributed to very low switched memory B lymphocytes count, impaired IFN-γ production by T and NK cells, reduced degranulation of NK cells, and abnormal T cell proliferation (9,17,18). Moreover, intractable diarrhea induces the loss of immunoglobulins from the intestines and breaks intestinal homeostasis, which may also lead to downregulation of vaccine response (9). Other rare symptoms include cardiovascular, genitourinary system, platelet anomalies, skeletal anomalies and abnormality of iron homeostasis, et al. The clinic features of previous four Chinese children and our case with THES syndrome 1 are consistent with other ethnicity (Table 1). The percentage individuals with platelet anomalies, a less frequent sign of THES, is 14% in patients with TTC37 mutation (6). Although reduced platelet α-granules and abnormal platelet canalicular system were observed in our patient, there was no hemorrhagic diathesis. That finding was consistent with the normal results of platelet aggregation assay and blood coagulation index, as well as with previous report (14). However, the molecular basis has not been elucidated.
Table 1
| Patient identification | Mainland China | Singapore | Malaysia | Taiwan (China) Case 1 | Taiwan (China) Case 2 | Total patients |
|---|---|---|---|---|---|---|
| Growth (IUGR/failure to thrive) | IUGR | Failure to thrive | Failure to thrive | Failure to thrive | IUGR | Almost all |
| Facial dysmorphy | Yes | Yes | Yes | Yes | No | Almost all |
| Hair abnormalities | Yes | Yes | Yes | Yes | No | Almost all |
| Skin abnormalities | Fair skin | Eczema | No | Café’au lait spots | No | Approximately50% |
| Refractory diarrhea (onset age) | Yes (3 wk) | Yes (4 wk) | Yes (2 mo) | Yes (2 wk) | Yes (new born) | Almost all |
| TPN | Yes | Yes | Yes | Yes | Yes | Almost all |
| Liver disease | No | Cirrhosis | Hepatomegaly | Cirrhosis | Cirrhosis | Approximately 50% |
| Neurodevelopmental delay | No | Yes | No | Yes | No | Approximately 50% |
| Dysimmunity | Yes | Yes | No | Yes | Yes | Approximately 50% |
| Cardiovascular | No | Small to moderate fenestrated atrial septal defect | No | Coaractation of aorta | Atrial septal defect | Approximately 10% |
| Platelet anomalies | Yes | No | No | Yes | No | Occasional |
| Skeletal anomalies | No | No | Poor dentition | No | No | Occasional |
| Genitourinary system | No | No | No | No | No | Occasional |
| Abnormality of iron homeostasis | Not available | Not available | Not available | Not available | Not available | Occasional |
| Mutation in genomic DNA | c.4130C>G Exon 11-13 del | c.3691C>T; c.3507T>G | c.3426dupA (homo) | Del3464-5AA (homo) | c.3507G>T; Ins3724A |
IUGR, intrauterine growth retardation; TPN, total parenteral nutrition.
It is noteworthy that the intractable hypoglycemia observed in our case has not been reported before in patients with THES. Even though there was a report of one THES patient with hyperinsulinism, no details were provided (16). In our patient, we excluded all metabolic, endocrine disorders, and genetic disorders causing hypoglycemia. Moreover, TTC37 disruption has been shown to cause mitochondrial dysfunction (19). A Drosophila model with disrupted TTC37 showed growth retardation, triacylglycerol accumulation, and aberrant metabolism in glycolysis and TCA cycle (20). The impaired aerobic metabolism may also cause hypoglycemia. However, the intractable hypoglycemia is relation to TTC37 gene mutation or secondary to malnutrition is still unknown. The association between intractable hypoglycemia and TTC37 genetic defect needs further evaluations.
In conclusion, our report described a first case of a Chinese infant with THES caused by TTC37 mutation from China mainland. Two novel mutations (c.4130C > G) and (Exon11-13 del) extend the gene mutation spectrum of THES. The clinical features of Chinese patient are consistent with other ethnicity. Molecular diagnosis is useful for patients with unexplained intractable diarrhea, which puts an end to a long diagnostic odyssey. The prenatal genetic diagnosis is possible, if the parents, whose infant with THES, are identified with TTC37 pathogenic variants.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundations of China (No. 82001601).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-21-574/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-21-574/coif). All authors report that they receive support from the National Natural Science Foundations of China, and have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardians for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fabre A, Badens C. Human Mendelian diseases related to abnormalities of the RNA exosome or its cofactors. Intractable Rare Dis Res 2014;3:8-11. [Crossref] [PubMed]
- Oz-Levi D, Weiss B, Lahad A, et al. Exome sequencing as a differential diagnosis tool: resolving mild trichohepatoenteric syndrome. Clin Genet 2015;87:602-3. [Crossref] [PubMed]
- Fabre A, Petit LM, Hansen LF, et al. A new mutation in the C-terminal end of TTC37 leading to a mild form of syndromic diarrhea/tricho-hepato-enteric syndrome in seven patients from two families. Am J Med Genet A 2018;176:727-32. [Crossref] [PubMed]
- Karaca Edeer N, Aykut A, Pariltay E, et al. A Novel TTC37 Mutation Causing Clinical Symptoms of Trichohepatoenteric Syndrome Such as Pyoderma Gangrenosum and Immunodeficiency Without Severe Diarrhea. J Investig Allergol Clin Immunol 2019;29:396-8. [Crossref] [PubMed]
- Trichohepatoenteric Syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al. editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; January 11, 2018.
- Bourgeois P, Esteve C, Chaix C, et al. Tricho-Hepato-Enteric Syndrome mutation update: Mutations spectrum of TTC37 and SKIV2L, clinical analysis and future prospects. Hum Mutat 2018;39:774-89. [Crossref] [PubMed]
- Stankler L, Lloyd D, Pollitt RJ, et al. Unexplained diarrhoea and failure to thrive in 2 siblings with unusual facies and abnormal scalp hair shafts: a new syndrome. Arch Dis Child 1982;57:212-6. [Crossref] [PubMed]
- Fabre A, Bourgeois P, Coste ME, et al. Management of syndromic diarrhea/tricho-hepato-enteric syndrome: A review of the literature. Intractable Rare Dis Res 2017;6:152-7. [Crossref] [PubMed]
- Lee WI, Huang JL, Chen CC, et al. Identifying Mutations of the Tetratricopeptide Repeat Domain 37 (TTC37) Gene in Infants With Intractable Diarrhea and a Comparison of Asian and Non-Asian Phenotype and Genotype: A Global Case-report Study of a Well-Defined Syndrome With Immunodeficiency. Medicine (Baltimore) 2016;95:e2918. [Crossref] [PubMed]
- Lee WS, Teo KM, Ng RT, et al. Novel mutations in SKIV2L and TTC37 genes in Malaysian children with trichohepatoenteric syndrome. Gene 2016;586:1-6. [Crossref] [PubMed]
- Zheng B, Pan J, Jin Y, et al. Targeted next-generation sequencing identification of a novel missense mutation of the SKIV2L gene in a patient with trichohepatoenteric syndrome. Mol Med Rep 2016;14:2107-10. [Crossref] [PubMed]
- Chong JH, Jamuar SS, Ong C, et al. Tricho-hepato-enteric syndrome (THE-S): two cases and review of the literature. Eur J Pediatr 2015;174:1405-11. [Crossref] [PubMed]
- Kögel A, Keidel A, Bonneau F, et al. The human SKI complex regulates channeling of ribosome-bound RNA to the exosome via an intrinsic gatekeeping mechanism. Mol Cell 2022;82:756-769.e8. [Crossref] [PubMed]
- Monies DM, Rahbeeni Z, Abouelhoda M, et al. Expanding phenotypic and allelic heterogeneity of tricho-hepato-enteric syndrome. J Pediatr Gastroenterol Nutr 2015;60:352-6. [Crossref] [PubMed]
- Fabre A, Breton A, Coste ME, et al. Syndromic (phenotypic) diarrhoea of infancy/tricho-hepato-enteric syndrome. Arch Dis Child 2014;99:35-8. [Crossref] [PubMed]
- Fabre A, Martinez-Vinson C, Roquelaure B, et al. Novel mutations in TTC37 associated with tricho-hepato-enteric syndrome. Hum Mutat 2011;32:277-81. [Crossref] [PubMed]
- Vély F, Barlogis V, Marinier E, et al. Combined Immunodeficiency in Patients With Trichohepatoenteric Syndrome. Front Immunol 2018;9:1036. [Crossref] [PubMed]
- Kinnear C, Glanzmann B, Banda E, et al. Exome sequencing identifies a novel TTC37 mutation in the first reported case of Trichohepatoenteric syndrome (THE-S) in South Africa. BMC Med Genet 2017;18:26. [Crossref] [PubMed]
- Kohda M, Tokuzawa Y, Kishita Y, et al. A Comprehensive Genomic Analysis Reveals the Genetic Landscape of Mitochondrial Respiratory Chain Complex Deficiencies. PLoS Genet 2016;12:e1005679. [Crossref] [PubMed]
- Ohnuma K, Kishita Y, Nyuzuki H, et al. Ski3/TTC37 deficiency associated with trichohepatoenteric syndrome causes mitochondrial dysfunction in Drosophila. FEBS Lett 2020; [Epub ahead of print]. [Crossref] [PubMed]


