
Effectiveness of peer-mediated intervention on social skills for children with autism spectrum disorder: a randomized controlled trial
Introduction
Autism spectrum disorder (ASD) is a group of lifelong neurodevelopmental disorders. The core symptoms are social communication disorders and behavioral stereotypes with limited interest (1). The incidence of ASD in the United States is as high as 2.41%, while domestic studies show that the incidence of ASD in China is about 1%, all showing an increasing trend in recent years (2,3). For children with ASD, their social characteristics often engendered avoid eye contact, no attachment relationship, lack of compassion and sharing capabilities, imagination and role-playing games. Researchers have found autistic individuals have a higher degree of anxiety compared to the normal population and have a similar level of anxiety as those considered anxious (4). Therefore, the application of scientific and effective treatment methods to improve the social skills of autistic children is an urgent area to be explored in current pediatric medical and educational areas.
There are few definitive ideal therapies for ASD’s core and prevalent co-behavioral symptoms. The principles of therapy for ASD, according to professional opinion, include early scientifically-based, systematic, customized, and family-based therapies. The primary objective of treatment is to maximize functions, such as social communication abilities, quality of life, and capacity to live independently, while minimizing or eliminating maladaptive behaviors (5,6). There is considerable evidence that applied behavior analysis (ABA) and ABA-based early intensive behavioral intervention (EIBI) for children with ASD, their families, and the community can lead to the best outcomes (7). EIBI is a comprehensive treatment model, mainly based on discrete trial teaching (DTT). The technique focuses on teaching skills by giving clear instructions in a repeating and succinct manner, while reducing extraneous details, thereby making instructions “turn-responsive”. There is compelling evidence that EIBI is an effective and preferable treatment option for children with ASD at the moment (8). However, many families getting this therapy cannot afford it due to the exorbitant expense and lack of human and financial resources. Throughout the implementation and promotion of the therapy, several researchers also have expressed concerns that its misuse could result in additional harm to children with ASD, including more severe stereotyping and depression (9).
For the core symptoms of children with ASD, the National Institute for Health and Care Excellence (NICE) guidelines recommend social communication interventions based on play strategies and peer intervention, but no recommendations for biomedical or pharmacological interventions (10). Peer-mediated intervention (PMI) refers to an intervention that systematically teaches normally developing peers to help children with ASD actively participate in social interactions, thereby enabling children with ASD to acquire appropriate social skills. A core part of the approach is the use of peers to facilitate interaction in children with ASD, and studies have shown that the therapy can promote the integration of children with ASD into the school environment (11,12). Watkins et al. in 2015 reviewed 15 studies demonstrating the effectiveness of PMI in improving social interaction in ASD (13). However, the environments of the studies were schools, and mostly single-subject designs were used. PMI is frequently used in conjunction with other intervention tactics, such as peer intervention paired with game strategies, video demonstration, augmentative and alternative communication (AAC), etc. PMI began with basic free play between children with ASD and typically developing (TD) children and has evolved into a variety of types of intervention, including chances for peer contact, peer counseling, peer positive reporting, and group play (14). According to some researchers, although prior studies defined PMI approaches, the specific implementation of social games or operation steps has not been clearly explained (15,16).
Recently, academics have again thoroughly analyzed the effectiveness of PMI in children with ASD, revealing that the results of the analysis are consistent although there are still some gaps that need to be filled (17). For example, the current study is still planned as a multi-baseline single subject, lack of high-quality randomized controlled studies, and because of the substantial clinical variability of children with ASD and the limited sample size, the authors indicated that the results were published very cautiously. To fill in some of the gaps left by earlier research, this study used a randomized, parallel-controlled design to analyze the impact of PMI on social interaction in children with ASD at various symptom levels. We present the following article in accordance with the CONSORT reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-110/rc) (18).
Methods
Study design
This study was a single-center, randomized, single-blind, parallel-controlled clinical trial, and conducted from June 2019 to August 2019 at the outpatient clinics of Shanghai YangZhi Rehabilitation Hospital affiliated with Tongji University. The research was carried out in line with the Helsinki Declaration (as revised in 2013). The study protocol had been approved by the Ethics Committee of Shanghai YangZhi Rehabilitation Hospital with approval number YZ2019-015. The experimental group was a PMI group, and the control group was an ABA-based behavioral therapy group (EIBI). The parent(s) or legal guardian(s) of all participants gave their written informed consent. According to the PMI-related literature reviewed and the preliminary experimental results of this study in 2017 and 2018, the effect size d was 0.78, the two-sided test was used, and the type I error α was set to 0.05. Under the test power of 0.80, Gpower 3.1 the software estimated the total sample size to be 54 cases. Considering the 10% shedding rate, the final sample size for this study was 60 cases.
Study protocol
This study adopted the principle of stratified randomization, the subjects were randomized to either the PMI group or the EIBI group (1:1 ratio allocation). First, according to the degree of symptoms of the disease in children, it is classified into two types: mild to moderate and severe. Then, after randomization within each type, the final division into experimental and control groups was performed. The specific randomization method adopts the envelope method and the treatment plan received by each subject is coded by a random allocation sequence generated by a computer random number generator and placed in a sequential, sealed, light-tight envelope. Children who met the inclusion criteria can only open the envelope and receive the appropriate treatment when they agree to the trial. The research assistants who performed the data entry and analysis and the therapists who conducted the assessments were blinded to how the study subjects were grouped. However, due to the nature of the intervention, blinding the subjects and the therapists who administered the intervention was not possible.
Participants
Children with ASD
The study involved 110 sample children who met the criteria for ASD according to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (19) by a child neuropsychiatrist from a local children’s hospital and a pediatrician of our hospital. Participants met the following inclusion criteria: (I) diagnosed with ASD; (II) aged 4–12 years old; and (III) able to attend sessions continuously, with no more than four absences. The exclusion criteria were (I) children with extra impairments such as psychological problems or hearing or vision issues, and those who had motor limitations that would prohibit them from engaging in social games; (II) frequent uncontrolled aggressive behavior involving hurting themselves or others; and (III) unable to attend continuous treatment, less than 20 sessions.
PMI peers
Social recruitment through the form of posters and web platforms of our hospital was conducted for 1 month prior to the study commencing. A total of 28 children applied to attend the study, and each peer was also assessed with the Social Responsiveness Scale (SRS) to provide information on their social skills. Finally, 16 children who met the following inclusion criteria were selected as PMI peers: (I) aged 4 to 12 years old; (II) characteristics of enthusiasm, patient, voluntary, and had good pragmatic understanding and social skills based on their SRS score; and (III) able to attend continuously with no more than 1-week absences. Most peers were the children of hospital staff members, and five participated in previous experiments in 2017 and 2018. Peers were educated and trained in both group training and individual training by our experimenters for about one week, after which they were familiar with a basic knowledge of ASD and their role in the experiment.
Measures
For social interaction skills in ASD, one of the instruments currently recommended in China is the Social Responsiveness Scale (SRS) (20). The Childhood Autistic Rating Scale (CARS) can play a vital role in detecting the improvement of autism symptoms, and it has a high level of reliability and recognition (21). As a result, SRS and CARS were utilized in this study to measure the performance of children with ASD before and after the intervention. The primary outcome of the study was the changes in total SRS scores. The secondary outcomes were the changes in CARS and changes in various social indicators of SRS. During the clinical trial intervention period, the adverse events that occurred were strictly recorded as required, and the “Adverse Event Report” was filled out, including the time of occurrence, progress, and processing results.
SRS
For youngsters aged 4 to 18, the Chinese SRS version was utilized. The SRS consists of 65-item, each of which was assessed on a Likert scale (22) of 0 (not at all) to 3 (almost always). The basic raw score may then be computed, on a scale 0 to 195, with a score more than 75 indicating a clinically significant level of autistic social impairment, and the higher the score, the more severe the social impairment. The scale contains five subscales, named social awareness, social cognition, social communication, social motivation, and autistic mannerisms (23). Internal consistency (0.871–0.922) and test-retest reliability (0.81–0.94) were determined for the Chinese form of the SRS scale used in mainland China-based on research (24). This research also highlighted the validity and reliability of the caregiver-report SRS as a screening tool for ASD.
CARS
The CARS scale has 15 items that require a trained evaluator to perform while observing the child. Each item receives a score ranging from 1 (no abnormalities) to 4 (severe abnormalities), with symptoms ranging between 1 and 2 receiving a 1.5 rating, and so on. Scores range from 15 to 29.5 points indicating no autism, 30 to 37.5 is classified as mild to moderate autism, and 38 to 60 is classified as severe autism (25). According to the research and analysis of CARS, the consistency reliability of raters was 0.796, the internal consistency reliability was 0.876, the consistency between CARS and the diagnostic standard DSM-5 was high, and the Kappa score was 0.963 (26,27).
Procedures
Pre-intervention peer training
A week before the intervention, we held pre-intervention training sessions for the 16 peers who participated. They attended a lecture on basic ASD symptoms, watched a related video, and received training about how to enhance their positive support and reduce unexpected behavior or words that might appear. Peers also received training in the conduct of simple games from a treatment manual in which the experimenter taught them how to wait, cooperate, provide visual or physical prompts, coach, and give feedback to autistic children. Following the training, the trial therapists had individual conversations with the TD peers, discussing their understanding of the ASD disorder and explaining their roles and responsibilities in the trial.
Experimenter training
Experimenters from different backgrounds including three occupational experimenters, three speech and language pathologists, and one special education teacher were involved in this study. Before the intervention, experimenter training also unified all games through the treatment manual to guide the peers during the intervention. Each experimenter participated in two to three small groups which included two same-level ASD children and four typical development PMI peers. Based on the two previous experiments, we constructed a treatment manual including 28 social games based on evidence-based five types of PMI (28). We set different goals for mild to moderate and severe autism focused on social motivation, social awareness, social cognition, social communication, and social behavior, to improve social interaction and initiations. Contents and examples are shown in Table 1.
Table 1
| Levels of ASD | Objects | Type of peer intervention | Examples |
|---|---|---|---|
| Mild and moderate | Asking for help from peers actively | Peer modeling | Peers demonstrate rules of the game |
| Observing and imitating others by following game rules | Peer tutoring | Using verbal and gesture cues to assist autistic children | |
| Sharing success with others | Cooperative learning strategies | Copying games: respond when someone calls, observe, and imitate someone’s actions/language, then asking the next participant actively to demonstrate/speak to him/her | |
| Peer reinforcement | Verbally praising: “You are doing great! Thanks for being so helpful!” | ||
| Positive peer reporting | Talking about the detailed good performance in each session and appreciating autistic children’s cooperation and effort | ||
| Severe | Using an AAC device to ask for help or express needs | Peer modeling | Peers demonstrate rules of game and practice once |
| Completing waiting and taking turns | Peer tutoring | Hand over hand assist and wait for autistic children’s response | |
| Sharing food with others | Cooperative learning strategies | Passing games: one is drumming while the others pass around a toy/blossom/block to the next one | |
| Peer reinforcement | Praising by clapping hands and thumbing up when appropriate behavior occurs | ||
| Positive peer reporting | Appreciating autistic children’s cooperation and effort and giving a warm hug |
ASD, autism spectrum disorder; AAC, augmentative and alternative communication; PMI, peer-mediated intervention.
Intervention
This study was done three times a week, for 40 minutes each time, and the two groups had the same intervention frequency and treatment time.
Experimental group
The intervention sessions were conducted in the group training room in our hospital. We purchased and prepared all the materials and tools needed and stored them in a cabinet with some reward items. Each therapy session consisted of the stages outlined below (29):
- Step 1 (5 min): self-introduction (name, age), greeting everyone (children in the severe group who had difficulty in verbal communication were encouraged to shake hands);
- Step 2 (5 min): the experimenter talked about the rules of the game and invited two peers to demonstrate how to play;
- Step 3 (25 min): the game begins; peers helped the children with ASD in their group when using verbal and gesture cues or hand over hand assistance. The experimenter sat and assessed the interaction. When a project was done, the children were ecstatic and spontaneously celebrated by slapping their hands, thumbing up, and verbally praising each other. Such a celebration was a typical method to assist autistic children feel the joy of socializing and improved their social motivation;
- Step 4 (5 min): after completing the session, peers gave positive peer reporting and a warm hug to the autistic children to reinforce their performance (30).
Control group
The control group used ABA-based behavioral therapy (EIBI), with discrete trial teaching (DTT) as the main method, to reinforce the behavioral responses of children with ASD (31). In the control group, rehabilitation therapists blended core skills with particular training content, such as language expression and communication, gross and fine motor abilities, and social cognition.
Statistical analysis
Data analyses were performed using IBM SPSS Statistics Software Version 23.0 statistical software package for data processing and GraphPad Prism 9 for graph creating. The count data were expressed by the number of cases and percentage (%), and the differences between groups in the count data were compared by the chi-square test or Fisher’s exact test. The measurement data were expressed as mean (standard deviation), and the independent samples t-test was used after verifying that the data conformed to the normal distribution; if it did not conform to the normal distribution, the nonparametric test was used. Data comparison between different subgroups was performed by repeated analysis of variance, with homogeneity of variance test first, independent sample t-test was used for homogeneity of variance, and non-parametric Kruskal-Wallis one-way ANOVA was used for unequal variance. Data were summarized using the mean, standard deviation, median, and f test, and P<0.05 was considered as a significant difference to explore the effect of PMI on improving the social skills of autistic children. Using Cohen’s d or f, effect size estimates were generated for all mean differences (32), and 95% confidence intervals (CIs) or median were also reported.
Results
From June 2019 to August 2019, 55 ASD participants and 16 peers who met the inclusion and exclusion criteria were included in the study. One case in the experimental group dropped out owing to returning home, resulting in a 1.8% shedding rate. But all 55 children with ASD were included in the statistics, 29 in the experimental group (mild to moderate n=18, severe n=11) and 26 in the control group (mild to moderate n=15, severe n=11), following the intention-to-treat (ITT) principle in clinical trials (see Figure 1). For the result after the intervention of one ASD child who shed out of the experimental group, the mid-term evaluation data was used as the final data. Children with ASD were stratified by symptom level and divided into mild-moderate and severe subgroups by CARS assessment. After randomization, the baseline data of the experimental group and the control group in terms of age, gender, and subgroup status are shown in Table 2. During the intervention, no adverse events occurred in either study group in terms of safety assessment.
Table 2
| Characteristics | Training group (n=29) | Control group (n=26) | P | |||
|---|---|---|---|---|---|---|
| N | %/mean (SD) | N | %/mean (SD) | |||
| Gender | 0.171 | |||||
| Male | 27 | 93.10 | 21 | 80.77 | ||
| Female | 2 | 6.89 | 5 | 19.23 | ||
| Subgroups | 0.741 | |||||
| Mild to moderate | 18 | 62.07 | 15 | 57.69 | ||
| Severe | 11 | 37.93 | 11 | 42.31 | ||
| Age (months) | ||||||
| Mild to moderate | 18 | 77.83 (30.10) | 15 | 63.93 (18.36) | 0.129 | |
| Severe | 11 | 72.27 (17.44) | 11 | 74.64 (20.74) | 0.775 | |
| Total | 29 | 75.72 (25.81) | 26 | 68.46 (19.74) | 0.251 | |
P>0.05 means there is no statistical difference between the two groups. SD, standard deviation.
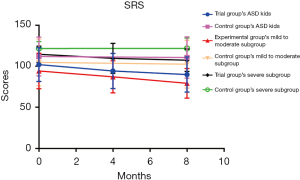
Within-group differences at posttest
The overall social ability scores of children with ASD in different groups and their subgroups at admission were compared with the scores after 1 month and 2 months of intervention. There were substantial differences in the overall ASD children and children with mild to moderate ASD in both two intervention groups before and after the intervention (P<0.05), as shown in Table 3 and Figure 2. The data analysis revealed that children with mild to moderate ASD showed differences after 1 month of intervention, with the SRS score decreasing by 7.11 (8.62) points, a difference that was statistically significant from the baseline (t=3.502, P=0.003). Following the 2-month intervention, the score declined further, to 15.06 (10.61) points lower than it was prior to the intervention, a difference that was likewise statistically significant (t=6.022, P=0.000).
Table 3
| Groups | Pre-intervention, mean (SD) | 4-week intervention, mean (SD) | 8-week intervention, mean (SD) |
|---|---|---|---|
| Trial group’s ASD kids (n=29) | 102.07 (20.52) | 94.35 (21.45)** | 89.97 (21.41)** |
| Control group’s ASD kids (n=26) | 111.92 (23.58) | – | 110.73 (25.50)* |
| Trial group’s mild to moderate subgroup (n=18) | 94.33 (21.65) | 87.22 (19.55)** | 79.28 (18.07)** |
| Control group’s mild to moderate subgroup (n=15) | 104.80 (28.53) | – | 102.60 (29.19)* |
| Trial group’s severe subgroup (n=11) | 114.72 (9.91) | 109.64 (18.33) | 107.46 (13.62) |
| Control group’s severe subgroup (n=11) | 121.64 (8.41) | – | 121.82 (12.66) |
*, P<0.05; **, P<0.01. ASD, autism spectrum disorder; SD, standard deviation; SRS, Social Responsiveness Scale.
Between-group differences and changes in different levels of ASD
Efficacy comparison of primary outcome measures: SRS
According to the changes in social ability before and after the intervention, the experimental group’s SRS score declined significantly more than the control group’s (t=−3.918, P=0.000), d=−1.043; the mild to moderate subgroup experienced the same situation (H=17.811, P=0.009), d=−1.642, as shown in Table 4. There was no significant difference in SRS score reduction between the experimental group’s severe subgroup and the control group (H=10.127, P=0.838), indicating that there was a significant difference in social skill improvement between the overall ASD children and the experimental group’s mild-to-moderate subgroup. PMI group outperformed the EIBI group.
Table 4
| Variation in SRS | N | Mean (SD) | t/H | P | d/ɳ2 | Differences of group mean of 95% CI/M (P25, P75) |
|---|---|---|---|---|---|---|
| Total | −3.918 | 0.000** | −1.043 | −16.211, −5.197 | ||
| Trt*Posttest | 29 | −11.90 (12.80) | ||||
| Ctrl*Posttest | 26 | −1.19 (6.87) | ||||
| Mild to moderate | 17.811 | 0.009** | −1.642 | −3.000 (−5.000, 0.000) | ||
| Trt*Posttest | 18 | −15.06 (10.61) | ||||
| Ctrl*Posttest | 15 | −2.20 (3.17) | ||||
| Severe | 10.127 | 0.838 | −0.456 | −2.000 (−12.250, 0.000) | ||
| Trt*Posttest | 11 | −6.73 (14.83) | ||||
| Ctrl*Posttest | 11 | 0.18 (10.03) |
**, P<0.01. CI, confidence interval; M, median; SD, standard deviation; SRS, Social Responsiveness Scale; P25, 25th percentile; P75, 75th percentile; Trt*Posttest, treatment group post-test; Ctrl*Posttest, control group post-test.
Efficacy comparison of secondary outcome measures: CARS
According to the changes in autism symptoms before and after the intervention, the experimental group’s CARS score declined significantly more than the control group’s (t=−2.812, P=0.007), d=−0.750, as shown in Table 5. There was no significant difference in the reduction of CARS scores both between the mild to moderate and severe subgroups of the experimental group and the control group (P>0.05), indicating that only the overall ASD children had significant differences in the improvement of autism symptoms, and the PMI group was better than the EIBI group.
Table 5
| Variation in CARS | N | Mean (SD) | t/H | P | d/ ɳ2 | Differences of group mean of 95% CI/M (P25, P75) |
|---|---|---|---|---|---|---|
| Total | −2.812 | 0.007** | −0.750 | −5.370, −0.899 | ||
| Trt*Posttest | 29 | −3.50 (3.29) | ||||
| Ctrl*Posttest | 26 | −0.37 (4.90) | ||||
| Mild to moderate | −0.691 | 1.000 | 0.960 | −1.000 (−2.500, 0.000) | ||
| Trt*Posttest | 18 | −2.42 (2.98) | ||||
| Ctrl*Posttest | 15 | −0.87 (1.09) | ||||
| Severe | 16.455 | 0.094 | −0.966 | −3.250 (−6.125, −1.250) | ||
| Trt*Posttest | 11 | −5.27 (3.12) | ||||
| Ctrl*Posttest | 11 | 0.32 (7.57) |
**, P<0.01. CARS, Childhood Autism Rating Scale; CI, confidence interval; M, median; SD, standard deviation; P25, 25th percentile; P75, 75th percentile; Trt*Posttest, treatment group post-test; Ctrl*Posttest, control group post-test.
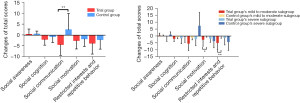
Efficacy comparison of secondary outcome measures: changes in different aspects of social skills
According to the change values of various social abilities before and after the intervention, the comparison between the groups showed that the social communication score of the experimental group decreased significantly larger than that of the control group (t=−3.869, P=0.000; 95% CI: −10.067, −3.193); the social motivation of the mild−to−moderate subgroup of the experimental group (H=16.894, P=0.011), −3.000 (25th percentile, 75th percentile: −3.000, 0.000) and the behavioral patterns of autism (H=18.150, P=0.006), −3.000 (25th percentile, 75th percentile: −5.000, 0.000), the decreased value was significantly larger than that of the mild to the moderate subgroup of the control group; and no significant difference between severe subgroups (P>0.05), as shown in Figure 3.
Discussion
The randomized controlled trial results indicated the effectiveness of a 2-month PMI intervention in a hospital environment for enhancing social skills in children with ASD. Through the evaluation and comparison before and after the intervention, it was determined that children with mild-to-moderate ASD in the PMI group had greater improvements in overall social skills than in the EIBI group. Notably, after a 1-month PMI intervention for the mild-to-moderate subgroup, social skills had been substantially different from those before the intervention, and the improvement was greater after 2 months of intervention.
In our study, peers were taught how to wait, cooperate, provide visual or physical prompts, coach, and give feedback to autistic children, and were presumed to be an active treatment mechanism. A new study from Westby indicates that peer demonstration and imitation encourage child-led play and natural interactions between kids (33). The social games used to intervene in the study included “rotating games” and “imitation games”. In the rotating games, one child is drumming while the others pass around a toy/blossom/block to the next one or they may compare the speed of passing all items to determine the winners. As they sat at a certain distance, the whole game requires children to respond and ask the name of the child nearby and could improve their social initiation and interaction skills. In the imitation games, children sat facing one direction one by one and observed and imitated someone’s actions/language, then demonstrated/spoke and repeated this to the next child. Children with autism exhibit significant deficits in imitation skills, which impedes the acquisition of more complex behaviors and socialization (34). According to Ingersoll (35), low-intensity, targeted imitation interventions can significantly improve persistent social deficits in ASD. Multiple studies have demonstrated a substantial association between imitation abilities and social behaviors in children with ASD, such as social reciprocity and the beginning of joint attention (35-37). However, it is still unknown whether imitation deficiencies are the cause or result of social impairment in ASD. Combining highly effective social imitation techniques with PMI therapy can enhance the social behavior of children with ASD and increase the likelihood of natural interactions, such as peer responses (38). Thus, social communication, social initiation, and social interaction could be improved by playing these games, and the more familiar and skillful the peers, the better. In these environments, children with ASD have the chance to interact socially with a large number of children their age, which enhances the possibility that they will acquire social skills that are generalizable (39).
To investigate the effectiveness of PMI in children with ASD more accurately, we conducted stratified research based on the severity of the children’s ASD symptoms. In comparison to EIBI, the results demonstrated that children with mild-to-moderate ASD showed a greater improvement in social skills. Before the official start of this study, the research team drew on the previous pre-experiment to design social games of varying degrees of difficulty based on the five intervention types in PMI therapy, taking into account the characteristics of ASD children with varying levels of symptoms and formed a treatment manual. However, we found children in the severe level small groups could not participate well through the same social games used in mild to moderate level groups, as they could not comprehend the meaning of games, which made it difficult to cooperate and complete them successfully. Moreover, the PMI peers also felt frustrated and had less positive behavior and emotions toward severely autistic children. A treatment manual and improved implementation fidelity may be required in such cases (40).
Because PMI is primarily an intervention strategy to enhance the social skills of children with ASD, we did comparison research on the indicators of various social skills in each subgroup of children with ASD. The study showed that the PMI group was significantly better than the EIBI group in the improvement of autism symptoms and social communication skills in overall ASD children, and the improvement of social motivation and autistic behavior in children with mild to moderate autism. According to research, social difficulties in ASD are mainly caused by abnormalities in social motivation and/or social cognition (41). Some researchers suggest that persons who do not have cognitive impairments should first work on strengthening their social motivation before gaining social skills (42). The theory of social motivation states that weak social motivation can make people change their attention to social information and disrupt the seeking of social experience, thereby triggering the knock-on effect of poor social learning (43). In this study, therapists instructed peer children to use methods preferred by children with ASD to engage their attention, follow the rules of play for various social interactions, and provide timely feedback, thereby reducing the occurrence of negative behavioural patterns in children with ASD. In addition, there is evidence that timely rewards in social encounters can increase social motivation (44). We found that increased social motivation had a significant impact on overall social competence.
Although most studies investigated PMI in inclusive settings or school settings, it is still important and meaningful to explore its effectiveness in a hospital setting as many autistic children receive initial services in hospital or rehabilitation centers (13,45). This setting could be an important foundation to establish basic social skills before children enter the school context and promote better performance for school participation and daily life. In some developing countries, including China, there are few therapists or special education teachers working in schools, and children with ASD even cannot attend normal schools due to a lack of support and effective approach to help them (46). The improvement of their social skills in the hospital setting will provide more opportunities for children to be admitted to school, improving their performance.
Based on the above analysis, we also identify several flaws in this work. First, a bigger sample size is required to investigate the influence of PMI on the various social functions of ASD children. This study is influenced by the actual scenario, and the smaller sample size is insufficient to accurately reflect the variations in each index of the severe subgroup. Second, the primary and secondary indicators of this study are semi-quantitative scales and insufficiently objective. In the future, testing can consider more objective quantitative indicators. Third, ASD requires long-term intervention, and the observation time of this study is limited. In order to obtain more sufficient evidence, real-world studies may be considered in the future.
Conclusions
According to the findings, PMI therapy can increase social motivation in children with mild to moderate ASD, minimize undesirable behavior patterns, effectively improve overall social skills and enhance effective social communication with others. After expanding the sample size, improving social games, or increasing the duration of the intervention, the efficacy of children with severe ASD has to be further investigated.
Acknowledgments
We would like to express our gratitude to all PMI peers, autistic children, and their families for participation and cooperation in this work. We also appreciate the teamwork of the Pediatric Rehabilitation Department at Shanghai YangZhi Rehabilitation hospital.
Funding: This study was supported by the Shanghai Federation of the Disable Research Project and Shanghai YangZhi Rehabilitation Hospital.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-110/rc
Trial Protocol: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-110/tp
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-110/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-110/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The research was carried out in line with the Helsinki Declaration (as revised in 2013). The study protocol had been approved by the Ethics Committee of Shanghai YangZhi Rehabilitation Hospital with approval number YZ2019-015. The parent(s) or legal guardian(s) of all participants gave their written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharma SR, Gonda X, Tarazi FI. Autism Spectrum Disorder: Classification, diagnosis and therapy. Pharmacol Ther 2018;190:91-104. [Crossref] [PubMed]
- Xu G, Strathearn L, Liu B, et al. Prevalence of Autism Spectrum Disorder Among US Children and Adolescents, 2014-2016. JAMA 2018;319:81-2. [Crossref] [PubMed]
- Sun X, Allison C, Wei LP, et al. Autism prevalence in China is comparable to Western prevalence. Molecular Autism 2019;10:7. [Crossref] [PubMed]
- White SW, Oswald D, Ollendick T, et al. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev 2009;29:216-29. [Crossref] [PubMed]
- Subspecialty Group of Developmental and Behavioral Pediatrics. the Society of Pediatrics, Chinese Medical Association; Children's Health Committee, Pediatric Branch of the Chinese Medical Doctor Association; Childhood Autism Diagnosis and Prevention Technology and Standards Research Project Expert Group. Principles of identification and management of common co-occurring problems in children with autism spectrum disorders. Chinese Journal of Pediatrics 2018;56:174-8.
- Will MN, Currans K, Smith J, et al. Evidenced-Based Interventions for Children With Autism Spectrum Disorder. Curr Probl Pediatr Adolesc Health Care 2018;48:234-49. [Crossref] [PubMed]
- Howard JS, Stanislaw H, Green G, et al. Comparison of behavior analytic and eclectic early interventions for young children with autism after three years. Res Dev Disabil 2014;35:3326-44. [Crossref] [PubMed]
- Grigorenko EL, Torres S, Lebedeva EI, et al. Evidence-Based Interventions for ASD: A Focus on Applied Behavior Analysis (ABA) Interventions. Psychology. Journal of the Higher School of Economics 2018;15:711-27.
- Kupferstein H. Evidence of increased PTSD symptoms in autistics exposed to applied behavior analysis. Advances in Autism 2018;4:19-29. [Crossref]
- Assessment, diagnosis and interventions for autism spectrum disorders: a national clinical guideline. Edinburgh, Scotland: Scottish Intercollegiate Guidelines Network (SIGN), 2016. Available online: http://resource.nlm.nih.gov/101714471
- Chan JM, Lang R, Rispoli M, et al. Use of peer-mediated interventions in the treatment of autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders 2009;3:876-89. [Crossref]
- Bambara LM, Cole CL, Telesford A, et al. Using Peer Supports to Encourage Adolescents With Autism Spectrum Disorder to Show Interest in Their Conversation Partners. J Speech Lang Hear Res 2021;64:4845-60. [Crossref] [PubMed]
- Watkins L, O'Reilly M, Kuhn M, et al. A review of peer-mediated social interaction interventions for students with autism in inclusive settings. J Autism Dev Disord 2015;45:1070-83. [Crossref] [PubMed]
- Schmidt C, Stichter JP. The Use of Peer-Mediated Interventions to Promote the Generalization of Social Competence for Adolescents with High-Functioning Autism and Asperger's Syndrome. Exceptionality 2012;20:94-113. [Crossref]
- Carter EW, Cushing LS, Clark NM, et al. Effects of Peer Support Interventions on Students' Access to the General Curriculum and Social Interactions. Research and Practice for Persons with Severe Disabilities 2005;30:15-25. [Crossref]
- Trembath D, Balandin S, Togher L, et al. Peer-mediated teaching and augmentative and alternative communication for preschool-aged children with autism. J Intellect Dev Disabil 2009;34:173-86. [Crossref] [PubMed]
- Aldabas R. Effectiveness of peer-mediated interventions (PMIs) on children with autism spectrum disorder (ASD): a systematic review. Early Child Development and Care 2019;190:1586-603. [Crossref]
- Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010;152:726-32. [Crossref] [PubMed]
- Vahia VN. Diagnostic and statistical manual of mental disorders 5: A quick glance. Indian J Psychiatry 2013;55:220-3. [Crossref] [PubMed]
- Hodges H, Fealko C, Soares N. Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation. Transl Pediatr 2020;9:S55-65. [Crossref] [PubMed]
- Chu JH, Bian F, Yan RY, et al. Comparison of diagnostic validity of two autism rating scales for suspected autism in a large Chinese sample. World J Clin Cases 2022;10:1206-17. [Crossref] [PubMed]
- Leung S-O. A Comparison of Psychometric Properties and Normality in 4-, 5-, 6-, and 11-Point Likert Scales. Journal of Social Service Research 2011;37:412-21. [Crossref]
- Cederberg CD, Gann LC, Foley-Nicpon M, et al. ASD Screening Measures for High-Ability Youth With ASD: Examining the ASSQ and SRS. Gifted Child Quarterly 2018;62:220-9. [Crossref]
- Cen CQ, Liang YY, Chen QR, et al. Investigating the validation of the Chinese Mandarin version of the Social Responsiveness Scale in a Mainland China child population. BMC Psychiatry 2017;17:51. [Crossref] [PubMed]
- Chlebowski C, Green JA, Barton ML, et al. Using the childhood autism rating scale to diagnose autism spectrum disorders. J Autism Dev Disord 2010;40:787-99. [Crossref] [PubMed]
- Breidbord J, Croudace TJ. Reliability generalization for Childhood Autism Rating Scale. J Autism Dev Disord 2013;43:2855-65. [Crossref] [PubMed]
- Meng X, Jiang H, Ma G, et al. Comparison of the application value of two scales in diagnosing autism spectrum disorders in children. Guangxi Medical Journal 2018;40:503-5.
- Dunn M, Shelnut J, Ryan J, et al. A Systematic Review of Peer-Mediated Interventions on the Academic Achievement of Students with Emotional/Behavioral Disorders. Education and Treatment of Children 2017;40:497-524. [Crossref]
- Hu X, Zheng Q, Lee GT. Using Peer-Mediated LEGO® Play Intervention to Improve Social Interactions for Chinese Children with Autism in an Inclusive Setting. J Autism Dev Disord 2018;48:2444-57. [Crossref] [PubMed]
- Smith SM, Simon J, Bramlett RK. Effects of Positive Peer Reporting (PPR) on Social Acceptance and Negative Behaviors Among Peer-Rejected Preschool Children. Journal of Applied School Psychology 2009;25:323-41. [Crossref]
- Chen Y, Cao J. A rehabilitation intervention model for children with autism spectrum disorders. Chinese Journal of Practical Pediatrics 2019;34:652-55, 665.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd edition. New York: Routledge, 1988.
- Westby C. Improving Play of Children With Autism Through a Peer-Mediated Intervention. Word of Mouth 2021;32:9-12. [Crossref]
- Ingersoll B, Schreibman L. Teaching reciprocal imitation skills to young children with autism using a naturalistic behavioral approach: effects on language, pretend play, and joint attention. J Autism Dev Disord 2006;36:487-505. [Crossref] [PubMed]
- Ingersoll B. Brief report: effect of a focused imitation intervention on social functioning in children with autism. J Autism Dev Disord 2012;42:1768-73. [Crossref] [PubMed]
- Happé F, Cook JL, Bird G. The Structure of Social Cognition: In(ter)dependence of Sociocognitive Processes. Annu Rev Psychol 2017;68:243-67. [Crossref] [PubMed]
- Hanna E, Meltzoff AN. Peer Imitation by Toddlers in Laboratory, Home, and Day-Care Contexts: Implications for Social Learning and Memory. Dev Psychol 1993;29:701-10. [Crossref] [PubMed]
- Dueñas AD, Plavnick JB, Goldstein H. Effects of a Multicomponent Peer Mediated Intervention on Social Communication of Preschoolers With Autism Spectrum Disorder. Exceptional Children 2020;87:236-57. [Crossref]
- Martinez JR, Waters CL, Conroy MA, et al. Peer-Mediated Interventions to Address Social Competence Needs of Young Children With ASD: Systematic Review of Single-Case Research Design Studies. Topics in Early Childhood Special Education 2019;40:217-28. [Crossref]
- Gunning C, Breathnach Ó, Holloway J, et al. A Systematic Review of Peer-Mediated Interventions for Preschool Children with Autism Spectrum Disorder in Inclusive Settings. Review Journal of Autism and Developmental Disorders 2019;6:40-62. [Crossref]
- Dawson G, Webb SJ, McPartland J. Understanding the nature of face processing impairment in autism: insights from behavioral and electrophysiological studies. Dev Neuropsychol 2005;27:403-24. [Crossref] [PubMed]
- Itskovich E, Zyga O, Libove RA, et al. Complex Interplay Between Cognitive Ability and Social Motivation in Predicting Social Skill: A Unique Role for Social Motivation in Children With Autism. Autism Res 2021;14:86-92. [Crossref] [PubMed]
- Chevallier C, Kohls G, Troiani V, et al. The social motivation theory of autism. Trends Cogn Sci 2012;16:231-9. [Crossref] [PubMed]
- Warnell KR, Sadikova E, Redcay E. Let's chat: developmental neural bases of social motivation during real-time peer interaction. Dev Sci 2018;21:e12581. [Crossref] [PubMed]
- Carter EW, Gustafson JR, Sreckovic MA, et al. Efficacy of Peer Support Interventions in General Education Classrooms for High School Students With Autism Spectrum Disorder. Remedial and Special Education 2016;38:207-21. [Crossref]
- McCabe H. Parent Advocacy in the Face of Adversity: Autism and Families in the People's Republic of China. Focus on Autism and Other Developmental Disabilities 2007;22:39-50. [Crossref]



