
Rotational osteotomy with single incision and elastic fixation for congenital radioulnar synostosis in children: a retrospective cohort study
Introduction
Congenital radioulnar synostosis (CRUS) is a rare developmental malformation of the forearm bone that manifests as a fusion of the proximal radius and ulna, as well as forearm fixation in pronation at a certain angle (1). Various therapeutic methods have been reported previously for improving the clinical symptoms of CRUS (2-4). Although the supination function cannot be compensated by treatment, pronation function can be compensated by abduction of the shoulder joint and extension of the elbow joint (5). Among these treatments, rotational osteotomy is widely used clinically due to its simplicity and effectiveness (6).
The deformity can be managed by either (7) no surgery in cases where the forearm is fixed in a useful position (8), excises the bar and the created space is filled by a tissue, and (3,9) derotation osteotomy, which places the forearm in a functional position. The derotation osteotomy is currently the most preferred (10). Bone fixation is most often performed using K-wires or plates (7,9), Many scars, loss of correction and neurovascular complications in the form were the most common complications across the studies (9,10,11). To correct the affected forearm to the target position and avoid complications such as osteofascial compartment syndrome, neurovascular stretch injury, and loss of forearm rotation angle, which may develop after rotational osteotomy, we improved rotational osteotomy for the radioulnar fusion portion according to the characteristics of osteogenesis in children by performing rotational osteotomy at the distal bifurcation of the fusion site combined with an elastic intramedullary nail for internal fixation and tubular plaster immobilization, allow replacement of the cast after 1–2 weeks of postoperative forearm detumescence to increase the forearm post-rotation angle. From June 2013 to June 2019, 27 children with CRUS were admitted and treated in The Third Affiliated Hospital of Southern Medical University. All of the patients underwent rotational osteotomy with single incision and elastic fixation by surgeons with the same level of seniority and similar surgical levels. Relatively complete follow-up data of the 27 cases (which included 39 affected limbs) were obtained. Among this study cohort, there were 23 males and four females, aged 3–13 years (average age, 5.6 years). All of the patients achieved a satisfactory clinical effect after surgery. In this article, we introduce the novel surgical method and evaluate its postoperative curative effect. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-111/rc).
Methods
Patients
Twenty-seven patients (including a total of 39 affected limbs) were admitted to the Third Affiliated Hospital of Southern Medical University from June 2013 to June 2019, including 23 males and four females (average age, 5.6 years; range, 3–13 years) (Table 1). Bilateral forearms were involved in 12 cases (three of these cases only received unilateral surgery), and a unilateral forearm was involved in 15 cases (eight cases on the left side and seven cases on the right side). Preoperative examination showed that the angle of fixed pronation deformity of the forearms ranged from 40° to 90°, with a mean of 59.7o±12.2o. All of the included patients had severe limitation of forearm rotation function on the affected side. Most of the children could only use a spoon instead of chopsticks for eating with the dominant hand, and could not hold a bowl with the non-dominant hand. The flexion and extension range of the elbow joints were normal, as were the shoulder and wrist joint functions. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of The Third Affiliated Hospital of Southern Medical University (No. 2022-004) and informed consent was taken from all the patients’ guardians.
Table 1
| Item | Value |
|---|---|
| Number of patients | 27 |
| Number of affected limbs | 39 |
| Age (years) | 5.6 (SD 2.7) |
| Sex | |
| Male | 23 |
| Female | 4 |
| Affected side | |
| Unilateral | 15 (8 left, 7 right) |
| Bilateral | 12 |
| Preoperative pronation angle | 40°–100° [average, 59.7° (SD 12.2°)] |
SD, standard deviation.
Study design
The inclusion criteria of this study were as follows: (I) patients diagnosed with a CRUS; (II) patients classified as type II, III or IV according to the Cleary-Omer classification (1); (III) patients who accepted rotational osteotomy; and (IV) patients whose parents agreed to the treatment plan. The exclusion criteria were as follows: (I) patients with surgical or anesthesia contraindications and those unable to undergo rotational osteotomy; (II) patients with other congenital malformations of the forearm; (III) patients whose affected limb had a previous injury that affected the forearm motion function; (IV) patients classified as type I according to the Cleary-Omer classification; and (V) patients whose postoperative follow-up data were missing.
The surgical indications were as follows: (I) pronation angle of affected forearm >60° in the non-dominant hand, or >30° in the dominant hand; (II) the patient’s parents had an urgent desire for treatment, and were told that the forearm would be fixed at a certain angle after surgery (the non-dominant hand would be fixed at a neutral position, and the dominant hand would be fixed at supination in 10°–20°).
Each patient was evaluated with activities of daily living (ADL) item scores before and after surgery (12). The hygiene and self-care items included: (I) washing face; (II) washing hair; (III) washing body; (IV) brushing teeth; (V) cutting nails; (VI) washing after defecation; (VII) lacing up shoes; (VIII) doing up buttons; (IX) dressing; (X) wearing pants; and (XI) zippering pants. The feeding-related items included: (I) using a spoon; (II) using chopsticks; (III) using a fork; (IV) using a knife; (V) drinking from a cup; (VI) pouring water into a glass; (VII) holding a bowl; and (VIII) holding a dish. The environment interaction items included: (I) using a phone; (II) reading and turning the pages; (III) writing; (IV) using a keyboard; (V) opening and closing a door (with twisting the handle); and (VI) getting up from a chair with the help of the hands. The evaluation rules were as follows: (I) 5 points signified a good result; (II) 4 points denoted a relatively good result; (III) 3 points represented a common result; (IV) 2 points signified a relatively bad result; and (V) 1 point denoted a bad result. The results of postoperative imaging examination and the final follow-up examination were compared (the union situation in osteotomy site), as well as whether the forearm rotation angle had changed. The pre- and post-operative ADL item scores were recorded for each patient.
Surgical technique
Under brachial plexus block anesthesia, the patient was placed in the supine position with the upper limb abducted and placed on the ball tube of the C-arm, and a pneumatic tourniquet was attached to the upper arm. Two Kirschner wires were inserted into the coronal plane of the medial and lateral condyles of the distal humerus for location of the proximal forearm, and the coronal plane of the radioulnar styloid for location of the distal forearm, respectively. Flexing the elbow to 90°, the vertical projection angles of the two Kirschner wires were marked as a reference to preoperatively determine the targeted rotation angle of osteotomy.
Following distal bifurcation of the radioulnar fusion site and determination of the incision position by the C-arm, a 3–4 cm incision was made longitudinally along the incision mark in the proximal ulna with the forearm placed in pronation. During this process, the skin, deep fascia, and ulnar periosteum were sequentially dissected. The periosteum was dissected along the ulna to the upper ulnar fusion bifurcation, and then released the interosseous membrane. Under the protection of the bone elevator, a transverse-truncation to the ulna and radius was performed in the same plane.
An incision (about 0.5 cm) was then made below the olecranon, which was determined as the pin entrance point, and two elastic intramedullary nails were inserted (under fluoroscopy with the C-arm) into the ulnar marrow cavity at a distance of 1 cm to the distal radial side of the olecranon. One nail was inclined to the radial side and the other was to the ulnar side, respectively entering the radial and ulnar marrow cavities and passing through the osteotomy line. Both nails were secured in the medullary cavity and flexible rotation was performed to avoid anchoring in the marrow cavity. The surplus of the intramedullary nail ends was cut off, and the ends of the nails were bent and buried subcutaneously after confirming that the position of the intramedullary nails was satisfactory by C-arm fluoroscopy, with the forearm supinated to the maximum degree.
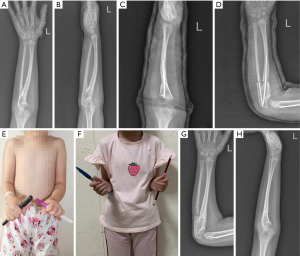
After fixation with intramedullary nails, the skin was sutured. Following the operation, the upper limb was immobilized with a tubular plaster to 90° of elbow flexion, 10°-20° supination of the dominant hand, pronation at the neutral position of the non-dominant hand, and functional position of the wrist joint. Attention was paid to the sensation and blood supply at the end of the affected limb (Figure 1). The tubular plaster was removed 4 weeks after surgery, and the intramedullary nails were taken out when imaging examination revealed satisfactory union at the osteotomy site (generally 3–5 months). Functional exercise with elbow flexion and forearm supination was performed every day after removal of the plaster.

Follow-up protocol
All participants were invited to a follow-up clinical examination. The patients were contacted by their physician working at the Third Affiliated Hospital of Southern Medical University. The patients were subjected to the following evaluation: elbow function, the ADL (dressing, writing, grabbing, reaching out the hand for catching objects, eating and drinking). The complications were assessed such as osteofascial compartment syndrome and vascular or nerve injury. Besides, the union at the osteotomy site is checked.
Statistical analysis
Measurement data were expressed as the mean (SD), while enumeration data were expressed as the number of cases and percentage. Repeated measures ANOVA (analysis of variance) was used to compare preoperative, postoperative, and final follow-up angle indexes, as well as the pre- and post-operative ADL scores between different groups. This study used a two-tailed test for the statistical analysis. P<0.05 was considered to indicate statistical significance.
Results
Surgery outcome
All patients were followed up postoperatively for a mean duration of 20.7 months. The fixed angles of forearm pronation after surgery were corrected to 0–20°, with a mean of 8.33º (SD 7.98°), and the difference was statistically significant compared with the baseline (P<0.01, Table 2). Postoperatively, none of the patients had limitations in elbow function, and the ADL, such as dressing, writing, grabbing, reaching out the hand for catching objects, and in particular eating and drinking, were basically normal and could be managed by the patients without any difficulty (Figure 2). The patients and their parents were satisfied with the forearm function. No complications, such as osteofascial compartment syndrome and vascular or nerve injury, occurred in any of the patients. Delayed union at the osteotomy site occurred in one patient, and union was achieved after forearm immobilization for a further month.
Table 2
| Items | Values |
|---|---|
| Baseline (Pre-op) (°) | 59.74 (12.25) |
| Post-op (°) | 8.33 (7.98) |
| Final follow-up (°) | 8.59 (8.10) |
| Difference between pre-op and post-op values (°) | 54.4 (14.4) |
| Difference between pre-op and final follow-up values (°) | 51.2 (14.5) |
| F | 236.85 |
| P | <0.001 |
Pre-op, pre-operation; Post-op, post-operation.
ADL assessment
The patients’ pre- and post-operative ADL item scores were compared. On average, the pre- and post-operative scores were 3.6 and 4.5, respectively, which was a 0.9-point change and was statistically significant (P<0.01). Specifically, the postoperative hygiene and self-care scores, feeding-related activities scores, and environmental interaction scores of the patients were all substantially improved (P<0.001), indicating that rotational osteotomy is an effective technique for CRUS in children and can improve the daily life of patients (P<0.01, Table 3).
Table 3
| Activity | Means (SD) | F | P | |
|---|---|---|---|---|
| Pre-op | Post-op | |||
| Hygiene and self-care items | 3.33 (0.27) | 4.38 (0.28) | 879.58 | <0.001 |
| Feeding-related items | 3.30 (0.30) | 4.38 (0.22) | 634.68 | <0.001 |
| Environmental interaction | 4.13 (0.23) | 4.52 (0.22) | 212.32 | <0.001 |
ADL, activities of daily living; SD, standard deviation; Pre-op, pre-operation; Post-op, post-operation.
Discussion
CRUS is a deformity caused by forearm bone dysplasia, which manifests as proximal fusion of the ulna and radius, and forearm fixation in pronation at a certain angle (13). At present, the pathogenesis of CRUS is still unclear; it is only known that the disease is inherited by those with a family history, mostly of patriarchal descent (14,15). In addition, congenital syndrome and other systemic malformations may occur simultaneously in patients with CRUS. Therefore, most scholars believe that this disease is related to genetic mutation and heredity (16,17). Cleary et al. (1) reported that the male-to-female ratio of the disease was about 1:1, and 60% of the patients had bilateral upper limb involvement. In this study, 15 patients had unilateral involvement and 12 patients had bilateral involvement. Twenty-three patients were males, and four were females. These results may be related to the fact that the number of included cases in this study was small, as well as the fact that young boys are more active and are more easily found to have this disease. Also, traditional concepts attach more importance to the hand function of boys and the need for surgery is more urgent in some areas. The forearms of all included patients were fixed in pronation and had dysfunction in rotation.
Numerous classification methods have been applied in CRUS, the most common of which is the Cleary-Omer classification (1), which is primarily based on imaging examination to detect whether there is an osseous connection at the proximal fusion site of the radius and ulna, and whether the radial head is dislocated. In order to facilitate intramedullary nail fixation at the same incision and perform osteotomy at the upper radioulnar fusion bifurcation, the Cleary-Omer classification was used in this study, except for type I upper radioulnar joint fiber connection.
The Jebsen-Taylor hand function test is a validated objective indicator of hand function, but its reference value should only be applied to children over 6 years of age (18). The Failla classification system, designed by Morrey et al., can be used for children over 2 years old (12), and can evaluate not only the outcomes of post-traumatic radioulnar joint synostosis, but also the forearm function (19). In this study, the ages of the included children ranged from 3 to 13 years old, with an average age of 5.6 years old. Therefore, the Failla classification system was used to compare the ADL scores before and after surgery. The results showed that the ADL scores were significantly enhanced after surgery, indicating that rotational osteotomy has a significant effect on the treatment of children with CRUS and improves their daily lives, as reflected by the substantial improvement in the hygiene and self-care, feeding-related activities, and environmental interactions of the patients postoperatively.
Simcock et al. (20) and Cleary et al. (1) reported a high incidence of neurovascular injury caused by osteotomy at the radioulnar joint fusion site. However, in this study, no neurovascular injury was observed in any patient with osteotomy at the distal bifurcation of the ulnar and radius fusion site (excluding the ulnar and radius fusion site itself). These results can be compared with other second-stage surgeries, such as drill-assisted osteotomy reported by Lin et al. (21) and dual rotary osteotomy demonstrated by El-Adl et al. (22). The results of the single-stage osteotomy in this study were similar to those of second-stage osteotomy.
In recent years, the surgical methods for CRUS have become a research hotspot, and rotation osteotomy is acknowledged owing to its good postoperative results (4,23).Murase et al. (24) and Hwang et al. (25) reported that CRUS therapy using rotation osteotomy achieved satisfactory results with employment of Kirschner wire to maintain stability after osteotomy and immobilization of the forearm with plaster external fixation. However, these methods were also prone to unstable fixation of the Kirschner wire, loss of rotation function, excessive correction of angle, and a high risk of osteofascial compartment syndrome after forearm muscle torsion. Consequently, rotational osteotomy with single incision and elastic fixation was applied in this study. The alignment of the osteotomy site was maintained with intramedullary nails elastically fixed in the radioulnar marrow cavity, and the forearm was maintained to the maximum corrective position with remodeling the elbow and wrist using tubular plaster. If complications such as obvious swelling of the forearm and numbness of the fingers occurred, the plaster could immediately be cut open longitudinally, allowing the forearm to rotate 5°–10° freely within the plaster, thereby relieving the swelling pressure in the forearm. After the swelling of the forearm is reduced, the plaster can be closed again and the forearm can be maintained at the optimal correction position.
The optimal position of forearm fixation postoperatively remains controversial (4).Factors such as the ages of the children, whether the affected limb is the dominant hand or not, tableware usage habits (e.g., chopsticks, knives and forks, or just hands), and employment intentions of the children (e.g., computer typing requires more forearm pronation) ought to be taken into account to determine the ideal position (11). Ramachandran et al. (4) showed that a slight supination position favors supination motions.In this study, in order to meet most patients’ requirements, including eating with their dominant hand using chopsticks (which involves the hand having to supinate), holding a bowl with non-dominant hand (which involves the hand having to pronate), and washing their perineum with their hands (which involves the hand having to supinate), the forearms of the non-dominant hand were fixed in a neutral position, while the forearms of the dominant hand were fixed in supination position of 10º–20°, with an overall postoperative supination fixation angle of 0–20° [average, 8.33 (SD 7.98)]. All of the patients had normal pronation and supination function postoperatively, with shoulder, elbow, and wrist compensations.
This operation is simple, and the key points are as follows. Firstly, two Kirschner wires need to be inserted into the coronal planes of the medial and lateral condyles of distal humerus and radioulnar styloid, respectively. By flexing the elbow to 90°, the vertical projection angle of the two Kirschner wires can reflect the angle of the forearm deformity preoperatively, which may act as a reference for the degree of correction required during surgery. During rotational osteotomy, the change of the forearm rotation angle was observed according to the change of the projection angle of the two Kirschner wires. Secondly, the osteotomy site is determined at the distal bifurcation of the radioulnar fusion site, and the osteotomy line is determined and marked under the C-arm. Thirdly, both the dominant and non-dominant forearms are fixed at the neutral position of 0°. In doing so, the function of holding food using a chopsticks can reach a close to normal level in the dominant forearm, with compensation through the shoulder and wrist joints, and may normalize the function of holding a bowl in the palm of the non-dominant forearm. These advantages are of great benefit to Asians who mostly have meals with chopsticks and bowls. In addition, considering increasing usage of keyboards in children, this fixed angle is convenient for patients to use a keyboard. Fourthly, after releasing the periosteum at the osteotomy site and ensuring that the forearm correction position is appropriate, the radius and ulna are fixed with intramedullary nails, and at the same time, attention should be paid to avoid anchoring the tip of the intramedullary nails into the marrow cavity. Next, a tubular plaster is used to immobilize the forearm to remodel the elbow and wrist joints, and maintain the forearm rotation angle. Lastly, if the soft tissue swelling is significant postoperatively, the plaster should be cut open to allow a slight pronation of the forearm, thus reducing the forearm swelling and the risk of osteofascial compartment syndrome. The tubular plaster may be sealed 7 days after surgery, or after forearm detumescence. The plaster is removed 1 month after the operation, and the forearm needs to exercise supination function under elbow flexion to prevent the loss of the supination angle of the forearm.
Compared with traditional rotation osteotomy, the technique applied in this study has the following advantages: (I) it is easy to perform: the surgery is relatively simple and easy to master; (II) it is minimally invasive: the surgery involves performing osteotomy in the same plane, the incision is small, and there is minimal postoperative scarring; (III) it is safe: osteotomy is performed at the bifurcation of the fusion site, which is superficial and avoids the widely developmentally malformed soft tissue, vessels and nerves; and (IV) it is adjustable: the elastic fixation is achieved with intramedullary nails for internal fixation and tubular plaster for external fixation, thereby reducing the risk of osteofascial compartment syndrome by cutting open the plaster according to forearm swelling to allow a certain amount of forearm motion space. It is also important to highlight the advantages of comprehensive functional rehabilitation exercise. Early and active functional exercise of elbow flexion and forearm supination after removal of the plaster can effectively avoid joint stiffness and prevent the loss of the supination angle of the forearm.
Conclusions
Taken together, the rotational osteotomy with single incision and elastic fixation technique for CRUS in children is easy to perform, less invasive, simple to master, and provides satisfactory postoperative outcomes. It basically meets most of the daily life needs of patients and is worthy of widespread clinical application. Nevertheless, there are still some drawbacks to this technique, including the fact that the patient’s forearm remains in the fixation position and cannot rotate postoperatively. Also, no management is provided to the fusion area, and consequently, elbow motion does not improve adequately in some patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-111/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-111/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-111/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of The Third Affiliated Hospital of Southern Medical University (No. 2022-004) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cleary JE, Omer GE Jr. Congenital proximal radio-ulnar synostosis. Natural history and functional assessment. J Bone Joint Surg Am 1985;67:539-45. [Crossref] [PubMed]
- Hung NN. Derotational osteotomy of the proximal radius and the distal ulna for congenital radioulnar synostosis. J Child Orthop 2008;2:481-9. [Crossref] [PubMed]
- Dong Y, Hu P, Liu F, et al. Treatment of congenital radioulnar synostosis with radial derotational osteotomy and local subcutaneous pedicled fat flap filling in fusion area. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2020;34:820-5. [PubMed]
- Ramachandran M, Lau K, Jones DH. Rotational osteotomies for congenital radioulnar synostosis. J Bone Joint Surg Br 2005;87:1406-10. [Crossref] [PubMed]
- Rutkowski PT, Samora JB. Congenital Radioulnar Synostosis. J Am Acad Orthop Surg 2021;29:563-70. [Crossref] [PubMed]
- Shingade VU, Shingade RV, Ughade SN. Results of single-staged rotational osteotomy in a child with congenital proximal radioulnar synostosis: subjective and objective evaluation. J Pediatr Orthop 2014;34:63-9. [Crossref] [PubMed]
- Bishay SN. Minimally invasive single-session double-level rotational osteotomy of the forearm bones to correct fixed pronation deformity in congenital proximal radioulnar synostosis. J Child Orthop 2016;10:295-300. [Crossref] [PubMed]
- Kanaya F, Ibaraki K. Mobilization of a congenital proximal radioulnar synostosis with use of a free vascularized fascio-fat graft. J Bone Joint Surg Am 1998;80:1186-92. [Crossref] [PubMed]
- Pei X, Han J. Efficacy and feasibility of proximal radioulnar derotational osteotomy and internal fixation for the treatment of congenital radioulnar synostosis. J Orthop Surg Res 2019;14:81. [Crossref] [PubMed]
- Barik S, Farr S, Gallone G, et al. Results after treatment of congenital radioulnar synostosis: a systematic review and pooled data analysis. J Pediatr Orthop B 2021;30:593-600. [Crossref] [PubMed]
- Ogino T, Hikino K. Congenital radio-ulnar synostosis: compensatory rotation around the wrist and rotation osteotomy. J Hand Surg Br 1987;12:173-8. Erratum in: J Hand Surg 1987;12:402. [PubMed]
- Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981;63:872-7. [Crossref] [PubMed]
- Pasupathy B, Tholgappiyan T, Sureshbabu M. Congenital radio ulnar synostosis, analysis of functional outcome using double rotation osteotomy and osteotomy at synostosis site. International Journal of Orthopaedics Sciences 2018;4:755-9. [Crossref]
- Iyoko IK, Iyoko II, Essien MA, et al. Congenital proximal radioulnar synostosis-a case report. Radiol Case Rep 2020;15:1313-6. [Crossref] [PubMed]
- Shen F, Yang Y, Li P, et al. A genotype and phenotype analysis of SMAD6 mutant patients with radioulnar synostosis. Mol Genet Genomic Med 2022;10:e1850. [Crossref] [PubMed]
- Elliott AM, Kibria L, Reed MH. The developmental spectrum of proximal radioulnar synostosis. Skeletal Radiol 2010;39:49-54. [Crossref] [PubMed]
- Suzuki T, Nakano M, Komatsu M, et al. ZMAT2, a newly-identified potential disease-causing gene in congenital radioulnar synostosis, modulates BMP signaling. Bone 2020;136:115349. [Crossref] [PubMed]
- Sears ED, Chung KC. Validity and responsiveness of the Jebsen-Taylor Hand Function Test. J Hand Surg Am 2010;35:30-7. [Crossref] [PubMed]
- Kshirsagar A, Kalaiah K, Sridhar DK. Derotational osteotomy in the treatment of congenital radioulnar synostosis: A report of 11 cases. International Journal of Orthopaedics Sciences 2021;7:108-11. [Crossref]
- Simcock X, Shah AS, Waters PM, et al. Safety and Efficacy of Derotational Osteotomy for Congenital Radioulnar Synostosis. J Pediatr Orthop 2015;35:838-43. [Crossref] [PubMed]
- Lin HH, Strecker WB, Manske PR, et al. A surgical technique of radioulnar osteoclasis to correct severe forearm rotation deformities. J Pediatr Orthop 1995;15:53-8. [Crossref] [PubMed]
- El-Adl W. Two-stage double-level rotational osteotomy in the treatment of congenital radioulnar synostosis. Acta Orthop Belg 2007;73:704-9. [PubMed]
- Satake H, Kanauchi Y, Kashiwa H, et al. Long-term results after simple rotational osteotomy of the radius shaft for congenital radioulnar synostosis. J Shoulder Elbow Surg 2018;27:1373-9. [Crossref] [PubMed]
- Murase T, Tada K, Yoshida T, et al. Derotational osteotomy at the shafts of the radius and ulna for congenital radioulnar synostosis. J Hand Surg Am 2003;28:133-7. [Crossref] [PubMed]
- Hwang JH, Kim HW, Lee DH, et al. One-stage rotational osteotomy for congenital radioulnar synostosis. J Hand Surg Eur Vol 2015;40:855-61. [Crossref] [PubMed]


