
This article has an erratum available at: http://dx.doi.org/10.21037/tp-21-475 the article has been update on 2021-10-01 at here.
Comparative study of one-stage and the novel two-stage urethroplasty using the transected urethral plate and transverse preputial island flap (TPIF) for severe hypospadias: a single-center experience
Introduction
Hypospadias is a common congenital anomaly of the pediatric urinary system. The prevalence of hypospadias in China has shown an increasing trend with an average annual increase of 7.43% from 1996 to 2008, especially in the eastern region (1). Compared with distal hypospadias, proximal hypospadias is more intractable in pediatric urinary surgery because it is often accompanied by severe chordee, which requires a more complicated surgical procedure and leads to a higher rate of postoperative complications. The urethral plate tissue is used as crucial material for hypospadias repair. The preservation of the urethral plate is relatively simple, and the complication rate is low. For hypospadias patients with severe concurrent chordee, transection of the urethral plate is unavoidable. Hence, urethroplasty combining transected urethral plate tissue and transverse preputial island flap (TPIF) has been increasingly adopted.
In recent years, the clinical application of two-stage surgery has been constantly reported, although most surgeons still choose the one-stage procedure for proximal hypospadias (2,3). Since 2014, one-stage and two-stage urethroplasty combining transected urethral plate and TPIF have been adopted to treat severe hypospadias at our hospital, with both procedures producing desirable effects. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tp-20-392).
Methods
Ethics statement
This study was conducted following the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Nanjing Medical University affiliated with Nanjing Children’s Hospital (NO. 201801172-1) and informed consent was obtained from all patients.
Study design and patients
Clinical data on 110 pediatric patients with proximal hypospadias accompanied by severe chordee who were admitted to our hospital between May 2014 and December 2019 were retrospectively analyzed. Urethral plate transection was performed on all patients. Among them, 14 patients received dorsal tunica albuginea plication to completely straighten the penis. All surgeries were performed by the same surgeon.
Surgical technique
Single-stage repair
After making two parallel incisions along with the urethral plate, circumcision was performed at 0.5 cm proximal to the coronal sulcus and penile skin was degloved to the root. Then, the urethral plate was transected at the point of maximum curvature. After dissociating the proximal urethral plate and the tunica albuginea, the penis was completely straightened. In case of incomplete correction, dorsal tunica albuginea plication was applied. We then used a 1.5 cm wide TPIF and moved it to the ventral penile side (Figure 1A). We made a vertical incision, the length of the proximal transected urethral plate, on the proximal midline of the flap (Figure 1B). We then inserted the plate to create a spoon-shaped proximal anastomosis. Thereafter, we sutured the tubularized flap from the proximal urethral opening to the distal penis. We then extended the two parallel incisions to the glans tip and made a vertical incision, the length of the distal transected urethral plate plus the glans urethral canal, on the distal midline of the flap. We inserted the urethral plate to create a spoon-shaped anastomosis (Figure 1C,D). We sutured the tubularized flap until the distal end (Figure 1E). We then dissociated the tunica albuginea of the corpora cavernosa from the glans and formed the border of the glans. We trimmed the border of the glans, pulled it closer to the middle line, and constructed a two-layer anastomosis on the glans. We covered the tension-free flap on the neourethra along the dorsal prepuce midline, according to the length of the urethra, and fixed it in place using one stitch. We then moved the dorsal prepuce to the ventral side of the penis, trimmed it, and sutured it to form the penile skin. We inserted a dual balloon catheter when suturing the urethral and pressure bandaged the incisions in the penis shaft, scrotum, and perineum. We later removed the pressure dressing on the 5th postoperative day and the urethral catheter on the 12th–14th postoperative day.
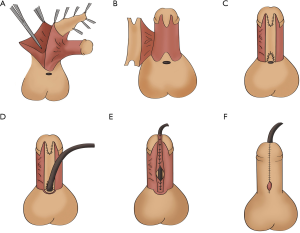
Two-stage repair
The procedure was similar to one-stage urethroplasty. The only difference was that when suturing, we left a fistula at the proximal end of the flap tube and fixed it in place to the surrounding skin using an interrupting suture to create the proximal end of the neourethral in the lower shaft (Figure 1F). Urethroplasty was performed at least six months or one year later. During urethroplasty, an incision was made 3 mm from the fistula in a circular manner. The flap was then dissociated until it was tension-free, and the interrupted sutures were made to form the urethra. We then covered subcutaneous penile tissue and sutured the incision. Later, we removed the urethral catheter on the 10th–12th postoperative day.
Statistical analysis
The chi-squared test was used to compare postoperative incidences of curvature, urinary fistula, urethral stricture, urethral diverticulum, and urethral rupture in the glans between the two groups. Measurement data were compared using Fisher’s exact test. A P value of <0.05 was considered to indicate statistical significance. All data were processed using GraphPad Prism 5 software.
Results
In total, 110 patients were included in our study. Among them, 66 patients (aged 7 months to 12 years, mean age 21.92±13.37 months at surgery) had undergone one-stage urethroplasty (one-stage group) and 44 (aged 7 months to 12 years and 9 months, mean age 24.78±13.59 months at surgery) had undergone partial staged urethroplasty (partial staged group). Patients in the one-stage group had 3–5 cm (3.57±0.53 cm) urethral defects with a glans diameter of 1.0–1.4 cm (1.20±0.083 cm), while patients in the two-stage group had 3–5 cm (3.86±0.70 cm) urethral defects with a glans penis diameter of 0.8–2.5 cm (1.21±0.39 cm). There were no statistically significant differences in age, glans diameter, or length of the urethral defect after straightening between the two groups (P>0.05) (Table 1).
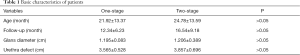
Full table
The two groups of patients were followed up for 2–53 months (mean follow-up: 14.02 months; Table 1). In the one-stage group, there were 18 cases with urinary fistula (6 in the shaft and 12 in the coronal sulcus) and one case each of granular dehiscence, urethral diverticulum, urethral diverticulum, and urethral rupture in the glans. Among these cases, 20 were treated by performing a second fistula repair or urethroplasty, while the patient with granular dehiscence did not receive a second surgery after declining the treatment. In contrast, in the two-stage group, no patients reported urinary fistula after the second fistula repair. Only 4 cases of granular dehiscence were found, while 2 of these cases were successfully repaired after reoperation and another two were not repaired due to underdeveloped glans and potential postoperative complications, after obtaining consent from their parents. The success rate of surgery in the one-stage group was 62.5%, while the partial staged group had a success rate of 88.57%, indicating a statistically significant difference between the two groups (Table 2). Additionally, age at surgery, glans diameter, and length of urethral defect did not show any statistically significant difference between the one-stage and two-stage groups. No urethral stricture was found in either group. No statistically significant difference was found in the incidence of the urethral diverticulum or granular dehiscence.
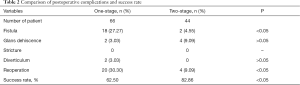
Full table
Discussion
Proximal hypospadias with severe concurrent chordee is a challenging disease for pediatric urology. Urethral plate transection combined with dorsal tunica albuginea plication is often used to fully correct the curvature. Since its debut in 1980, Duckett urethroplasty has become the preferred one stage surgical method to treat proximal hypospadias with severe concurrent chordee. However, the rates of postoperative complications after the Duckett procedure vary among different reports (4,5). Andersson et al. reported a high incidence of postoperative complications (ranging from 33% to 90%), with an especially high incidence of anastomotic stenosis at the proximal and distal ends (6). It is also acknowledged that the procedure of urethral stricture reversal after the hypospadias surgery is rather complicated. The anastomotic stenosis caused by the scar precludes the possibility of dilating the urethra and therefore cannot be treated using urethral dilatation. Hence, in most cases, urethrostomy must be conducted before staged surgery. Repeated operations may result in local scar contracture and subsequently poor cosmetic results. This not only exerts negative impacts on the outcomes and clinical application of Duckett urethroplasty but also creates suffering for both patients and their parents. Additionally, the Duckett procedure is complex and technically demanding, requiring a high level of clinical experience. As a result, many urologists exert extra caution when choosing this procedure.
Most scholars had previously thought that the urethral plate was underdeveloped and therefore should be excised, thus TPIF alone was used in urethroplasty. A small fraction of scholars held the notion that a well-developed urethral plate could be preserved and utilized in hypospadias repair, while a poorly developed or underdeveloped urethral plate had to be excised. Others considered the urethral plate as an ideal material to be used to repair hypospadias (7). For all types of hypospadias, preserving the urethral plate during urethroplasty ensures adequate blood supply in the newly formed urethra and provides ideal repair material. Additionally, in this procedure, no circular anastomosis is produced in the new urethra, lowering the risk of urethral stricture (8). Based on this concept, many surgeons have attempted to combine a transected urethral plate with TPIF in urethroplasty to improve the procedure.
Our previous study reported on the application of onlay-tube-onlay in treating severe hypospadias with obvious chordee. Using the advantages of both Duckett and Onlay, this technique used the dorsal TPIF and the transected urethral plate to form a new urethra (9,10). According to our previous study, only 9.3% developed urethral stricture among the 32 pediatric patients who received one-stage repair for severe hypospadias, which was significantly lower than that of Duckett (11). Huang et al. improved the Duckett technique by creating a V-shaped anastomosis (connecting the two ends of the TPIF with the proximal and the distal ends of the preserved plate) to avoid urethral stricture at the anastomotic sites (12). The above evidence suggests that reconstruction of the urethral plate avoids the occurrence of urethral stricture and diverticulum, but the risk of urethral fistula remains high. The reoperation may also result in the recurrence of complications, such as urethral fistula.
Recently, the incidence of hypospadias and its postoperative complications have been increasing, giving rise to the practice of staged surgery for hypospadias. Previously, surgeons had resorted to staged surgery due to a lack of understanding of the disease and a lack of effective surgical techniques. Nevertheless, at present, staged surgery has been adopted for specific types of hypospadias because it simplifies complex surgical procedures and lowers the incidence of postoperative complications. The most commonly used surgical techniques for the first stage are: Byars procedure, in which the dorsal prepuce is used preposition the urethral bed in the ventral penis shaft and the defective area in the glans is filled in; Bracka procedure, in which the preputial graft is used to preposition the urethral bed and the defective area in the glans is filled in; and partial urethroplasty. In both the Byars and Bracka procedures, either the preputial flap or preputial graft is used to preposition the urethral bed, and the defective area in the glans is filled in. Then, urethroplasty is completed in-situ or through longitudinal incised flap tubularization during the second stage. Although both procedures present fewer obstacles during surgery, the postoperative complication rates remain high after the second surgery due to severe urethral defects in patients. Faure reported that after Bracka, the incidence of the postoperative fistula was 5.7–15.3%, the incidence of urethral stricture was 3–16%, and the overall complication rate was 18–38% (2). Yang reported that for the Byars procedure, the overall complication rate was 11.8% and the incidence of granular dehiscence was 3.9% (3). For the Bracka procedure, the incidence of granular dehiscence was 5% (13). Zheng et al. compared the one-stage (Duckett) and staged (Byas/Bracka) procedures for proximal hypospadias with severe chordee and found no significant difference in the complication rate but a higher incidence of urethral stricture after Duckett (14). The third type of staged procedure, a partially staged procedure, in which partial urethroplasty is conducted during the first stage, has been inadequately reported on.
Chen et al. reported on a partially staged procedure using Duckett, in which the proximal end of the skin tube and the native urethral opening were used as the stoma at the penile scrotal junction (15). This procedure that resulted in a success rate of 90.5%, showed a significantly lower risk of urethral fistula than the staged Byars procedure. However, no statistically significant difference was found in the incidence of urethral stricture, granular dehiscence, or diverticulum. In our clinical practice, we found that postoperative complications, such as urethral stricture and diverticulum were rarely reported after urethroplasty in patients who developed urinary fistula, while the urethra distal to the stoma also healed well. Based on the literature and our clinical experience, we presumed that the staged surgery could reduce the risk of complications, such as urinary fistula, and the reconstruction of the urethral plate could lower the incidence of urethral stricture. Hence, we adopted the third type of staged procedure to avoid coronal sulcus fistula, which often occurs during one-stage urethral plate reconstruction.
Unlike the Duckett procedure, in which TPIF was tubularized to form the new urethra, in our procedure, the transected urethral plate was preserved and used to construct the new urethra. The advantages of our procedure are as follows: First, the transected urethral plate was sutured with the TPFI, forming a V-shaped insertion with both TPFI ends. This avoided the need of a circular suture between the native-new urethral anastomotic stoma and the external urethral orifice. It also lowered the incidence of urethral stricture, simplified the construction of the external urethral orifice, and offered a superior cosmetic result. Second, the preserved urethral plate could support the new urethra and corpus cavernosum and reduced the risk of neourethral distortion. Third, the tubularized suture faced the ventral side, making it easier for suturing and setting up an indwelling fistula, unlike that which was observed using the Duckett procedure.
Among the 35 patients who received partially staged surgery in our study, none developed urethral fistula, urethral stricture, or diverticulum, and only 4 showed neourethral dehiscence in the glans. In contrast, among the 56 patients who underwent one-stage urethroplasty, no urethral stricture was found, although urethral fistula was the most frequent complication. Compared with the one-stage group, the partial staged group showed a significantly lower incidence of urethral fistula, which could be attributed to the following factors: the postoperative urethral secretions can be drained from openings at both ends of the penis without any retention in the new urethra, which lowers the risk of incision infection and urinary fistula; while patients with severe hypospadias are more prone to postoperative urethral rupture because they tend to have a smaller glans and a shallower groove. Bush et al. found that a glans diameter of <14 mm was an independent risk factor for complications after urethroplasty (16). The cases included in our present study had a mean glans diameter of 12 mm (range: 8–15 mm), which may account for the high complication rate in the one-stage group. After partially staged surgery, draining the urine from the fistula at the penile fistula could reduce the stimulation of urine flowing into the new urethra in the glans and the coronal sulcus, inducing better healing of the distal neourethra and a lower incidence of urinary fistula.
The partially staged procedure integrates the strengths of both one-stage and staged procedures, presenting advantages in distinctly lowering the incidence of urethral fistula and stricture, improving curative effects, and enriching choices available during surgical planning. Compared with the staged and one-stage procedures, the two-stage procedure has a low incidence of postoperative urinary fistula, which is preferred by the parents of patients. However, the two-stage procedure has its limitations. Patients may lose the chance of being cured by a single surgery and some may even have to receive three or more surgeries, increasing the cost of hospitalization and the use of medical resources. Currently, an essential issue for the application of the partially staged procedure is its cost-effectiveness, i.e., to identify patients who can benefit the most from this procedure. According to Springer et al., 43.3–78.6% of urologists chose staged surgery to repair proximal hypospadias (17), suggesting that the choice of surgical procedure is mostly based on personal preference. Based on the development of glans, the urethral plate and groove, positioning of the urethral opening, and the severity of chordee, a GMS hypospadias scoring system was established to grade hypospadias. The total score ranges from 3 to 12, and a higher score indicates more severe hypospadias (18). Huang et al. randomized patients with GMS hypospadias score of 10–12 and performed one-stage or staged (Byars) urethroplasty on them, and then analyzed the postoperative complications. The analysis showed a significantly lowered complication rate in the staged group than the one-stage group, suggesting that GMS can guide the choice of the most suitable surgical method (19). Nevertheless, compared with other countries, China has a larger proportion of severe hypospadias patients with poorly developed glans and severe chordee (1). Furthermore, unlike the evaluation of the urethral opening and chordee, the scoring of the glans and urethral plate in GMS is rather subjective. For these two reasons, a scoring system for hypospadias patients in China is needed to determine whether one-stage or staged surgery would be most suitable. At present, we are conducting a prospective randomized control study, in which data (including length, diameter, and width of glans, curvature degree, and length of the urethral defect) of the hypospadias of patients who have undergone either one-stage or staged surgeries are being collected to establish a specific scoring system for these Chinese patients.
The limitations of this study include the inclusion of only a limited number of patients and a relatively short follow-up period during which outcomes and complications were observed. Studies conducted on a larger sample size and for a longer follow-up duration are warranted to evaluate the different types of urethroplasty. To provide additional reasons that favor this novel modification, a prospective study needs to be conducted. The results of a prospective study will certainly be more convincing than the retrospective analysis conducted in this study.
Conclusions
Both the transected urethral plate and TPIF are ideal materials to be used to repair urethral defect. partially staged urethroplasty using the transected urethral plate and TPIF is the most advancement in hypospadias repair and results in an outcome similar to that of the one-stage procedure. Indications for two-stage urethroplasty are controversial. In clinical practice, the choice of procedure is determined based on glans development, the degree of chordee, and the length of the urethral defect, as well as the preference of the parents of the patient after informing them of the advantages and disadvantages of the different procedures. Furthermore, a prospective randomized control study is warranted to guide the choice of urethroplasty for severe hypospadias.
Acknowledgments
We thank Dr. Fang Chen for his assistance with the manuscript and the surgical procedures. We thank the parents of all patients enrolled in this study. We also thank all members of the Department of Urology at Nanjing Children’s Hospital.
Funding: This research received funding from the Science and Technology Development Project of Nanjing Medical University (2017NJMUZD052) and the SEU-NMU Cooperation Project (2242018K3DN02).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tp-20-392
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tp-20-392
Peer Review File: Available at http://dx.doi.org/10.21037/tp-20-392
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-20-392). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the study in ensuring that questions related to the accuracy or integrity of any part of the study are appropriately investigated and resolved. The study was conducted following the Declaration of Helsinki (as revised in 2013). The study was approved by the local Ethics Committee of Nanjing Medical University affiliated with Nanjing Children’s Hospital (NO. 201801172-1) and informed consent was obtained from the parents or guardians of all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li Y, Mao M, Dai L, et al. Time trends and geographic variations in the prevalence of hypospadias in China. Birth Defects Res A Clin Mol Teratol 2012;94:36-41. [Crossref] [PubMed]
- Faure A, Bouty A, Nyo YL, et al. Two-stage graft urethroplasty for proximal and complicated hypospadias in children: A retrospective study. J Pediatr Urol 2016;12:286.e1-7. [Crossref] [PubMed]
- Yang T, Zou Y, Zhang L, et al. Byars two-stage procedure for hypospadias after urethral plate transection. J Pediatr Urol 2014;10:1133-7. [Crossref] [PubMed]
- Pfistermuller KL, McArdle AJ, Cuckow PM. Meta-analysis of complication rates of the tubularized incised plate (TIP) repair. J Pediatr Urol 2015;11:54-9. [Crossref] [PubMed]
- Hueber PA, Salgado Diaz M, Chaussy Y, et al. Long-term functional outcomes after penoscrotal hypospadias repair: A retrospective comparative study of proximal TIP, Onlay, and Duckett. J Pediatr Urol 2016;12:198.e1-198.e1986.
- Andersson M, Sjöström S, Doroszkiewicz M, et al. Urological results and patient satisfaction in adolescents after surgery for proximal hypospadias in childhood. J Pediatr Urol 2020;16:660.e1-8. [Crossref] [PubMed]
- Erol A, Baskin LS, Li YW, et al. Anatomical studies of the urethral plate: why preservation of the urethral plate is important in hypospadias repair. BJU Int 2000;85:728-34. [Crossref] [PubMed]
- Myers JB, Porten SP, McAninch JW. The outcomes of perineal urethrostomy with preservation of the dorsal urethral plate and urethral blood supply. Urology 2011;77:1223-7. [Crossref] [PubMed]
- Huang Y, Xie H, Lv Y, et al. One-stage repair of proximal hypospadias with severe chordee by in situ tubularization of the transverse preputial island flap. J Pediatr Urol 2017;13:296-9. [Crossref] [PubMed]
- Huang LQ, Wang J, Ge Z, et al. Comparative study of urethroplasties to reduce urethral strictures in patients with severe hypospadias. J Int Med Res 2019;47:1620-7. [Crossref] [PubMed]
- Nuhoğlu B, Ayyildiz A, Balci U, et al. Surgical treatment options in proximal hypospadias: retrospective analysis of 171 cases at a single institution. Int Urol Nephrol 2006;38:593-8. [Crossref] [PubMed]
- Huang LQ, Guo YF, Ge Z, et al. A new modification of the Duckett technique for one-stage repairing urethral plate transected hypospadias: Another option for severe hypospadias?. Int Urol Nephrol 2017;49:2091-7. [Crossref] [PubMed]
- Johal NS, Nitkunan T, O'Malley K, et al. The two-stage repair for severe primary hypospadias. Eur Urol 2006;50:366-71. [Crossref] [PubMed]
- Zheng DC, Yao HJ, Cai ZK, et al. Two-stage urethroplasty is a better choice for proximal hypospadias with severe chordee after urethral plate transection: a single-center experience. Asian J Androl 2015;17:94-7. [Crossref] [PubMed]
- Chen C, Yang TQ, Chen JB, et al. The Effect of Staged Transverse Preputial Island Flap Urethroplasty for Proximal Hypospadias with Severe Chordee. J Urol 2016;196:1536-40. [Crossref] [PubMed]
- Bush NC, Villanueva C, Snodgrass W. Glans size is an independent risk factor for urethroplasty complications after hypospadias repair. J Pediatr Urol 2015;11:355.e1-355.e5. [Crossref] [PubMed]
- Springer A, Krois W, Horcher E. Trends in hypospadias surgery: results of a worldwide survey. Eur Urol 2011;60:1184-9. [Crossref] [PubMed]
- Merriman LS, Arlen AM, Broecker BH, et al. The GMS hypospadias score: assessment of inter-observer reliability and correlation with post-operative complications. J Pediatr Urol 2013;9:707-12. [Crossref] [PubMed]
- Huang J, Rayfield L, Broecker B, et al. High GMS score hypospadias: Outcomes after one- and two-stage operations. J Pediatr Urol 2017;13:291.e1-4. [Crossref] [PubMed]


