The burden of respiratory syncytial virus associated with acute lower respiratory tract infections in Chinese children: a meta-analysis
Introduction
Acute lower respiratory tract infections (ALRTIs) present a persistent and pervasive problem in public health owing to the substantial burden they place on health-care services (1). ALRTI is one of the leading global causes of childhood morbidity and mortality, particularly in developing countries. Respiratory syncytial virus (RSV) is the most common viral pathogen identified in young children with ALRTI and primarily leads to pneumonia and bronchiolitis. In 2015, there were an estimated 33.1 million new cases of RSV-associated ALRTI diagnosed in young children around the world. Hospitalization was required in approximately 10% of these cases, which led to an estimated 59,600 in-hospital deaths (2). It is worth noting that, because of limited health care, more than 92% of all RSV-associated ALRI episodes and nearly 99% of related fatalities occur in developing countries; this places a great burden on patients, parents, and broader society (3). Thus, novel strategies focusing on children, who may have a naturally weak immune system compared to adults, should be developed to curb the burden imposed by RSV infection.
China is one of the biggest developing countries with the largest population in the world. China’s climate varies substantially from region to region in terms of temperature and rainfall. A previous meta-analysis by Zhang et al. (4), which summarized relevant studies published between January, 2010 and March, 2015, evaluated the potential epidemiology of RSV infections among ALRTI patients in China. It found RSV infection to be a leading cause of viral ALRTIs in China, comprising 18.7% (95% CI: 17.1–20.5%) of all ALRTI cases, with a positive rate higher in children than in adult patients (4). Since then, a number of new studies have been published, yielding substantial new data (5-7). However, local variations in climate and the characteristics of study populations (e.g., rural vs. urban) have led to dramatic differences in the positive rates of RSV infection reported in individual studies. To date, the epidemiology of RSV infections among Chinese children has not been systematically summarized in English. It is therefore of great significance that a comprehensive meta-analysis to evaluate recent epidemiological data of RSV infections in Chinese patients is conducted, with a particular focus on children with ALRTIs.
In this meta-analysis, we aimed to estimate the burden of RSV-associated ALRTI in Chinese children by analyzing available studies published between January 1, 2015 and December 31, 2018. Specifically, this study was conducted to pool the positive rate of RSV infection among children with ALRTI in China, and to examine the rate in subgroup analyses incorporating different parameters such as age distribution, seasonality, and locations.
We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/tp-20-148).
Methods
Eligibility criteria
Studies meeting the following criteria were included in the meta-analysis: (I) all patients met diagnostic criteria for ALRTIs; (II) Chinese children younger than 18 years old; (III) containing outcome data of positive rate of RSV infection or providing sufficient information (the number of patients infected with HRSV and the number of patients screened) to calculate effect sizes; (IV) cross-sectional design; (V) obtained respiratory tract specimens for the detection of RSV; and (VI) RSV infections were confirmed through immunofluorescence assay or polymerase chain reaction. Articles meeting any of the following criteria were excluded: (I) systematic reviews, narrative reviews, or comments; (II) non-human studies; (III) Chinese journals not included in the Chinese core journals (2017 edition) evaluated by the Library of Peking University (8). In the event of overlapping data on the same patient population being reported in more than one publication, only the most comprehensive study was included.
Literature search
Searches were implemented of the PubMed, Web of Science, China National Knowledge Infrastructure (CNKI), Wanfang, and Chinese BioMedical (CBM) databases to identify studies published between January 1, 2015 and December 31, 2018. The following search terms were used: (Respiratorysyncytial virus OR RSV) and (Chinese OR China). The reference lists of enrolled papers and recent reviews were also manually searched.
Data collection process
The data were separately extracted from all eligible studies by two reviewers using a pre-defined form. The information recorded from each study included the first author’s name, year of publication, patients’ age and gender distribution, sample size, study period and settings, recruitment locations, diagnostic criteria of ALRTIs, type of sample collected for all patients [e.g., nasopharyngeal aspirate, nasopharyngeal swab, or bronchoalveolar lavage fluid (BALF)], methods for detecting RSV, the number of participants screened, and the number of patients with RSV infection. Any conflicts were resolved through discussion until a consensus was reached.
Case definition
ALRTI was defined according to the guidelines of the World Health Organization (WHO) as the presence of manifestations of acute respiratory tract infection including fever, coughing, rhinorrhea, and headache, and lower respiratory symptoms such as tachypnea, dyspnea, and rales upon auscultation (3).
Quality assessment
The methodological quality of the eligible cross-sectional studies was assessed using 11 items recommended by the Agency for Healthcare Research and Quality (AHRQ) (9). Each item was answered with “Yes”, “No”, or “Unclear”. An answer of “Yes” scored 1 point; otherwise, the score was “0”. The maximum score was 11, and studies with scores between 4 and 7 points were considered to be of moderate quality, while those with scores above 7 points were deemed to be of high quality.
Statistical analysis
The pooled positivity rate of RSV infections and the corresponding 95% confidence interval (CI) were calculated using R software (version 3.5.2, Auckland University, USA). Heterogeneity between included studies was determined by Chi-square-based Q-statistic test (statistical significance = P<0.10) and the I2statistic. When the heterogeneity between studies was not good (I2<50% and P>0.1), a fixed-effects model was adopted for the calculation of positivity rate; otherwise, a random-effects model was used. Moreover, subgroup analyses were conducted based on age distribution, study settings, publication language, method of detection for RSV infection, sample type, and seasonality. In the presence of significant heterogeneity, sensitivity analysis was carried out to test the stability of the overall results via eliminating individual studies in turn. Egger’s test was also employed to quantify publication bias. All P values were two-sided, with P<0.05 suggesting statistical significance.
Results
Study selection and characteristics
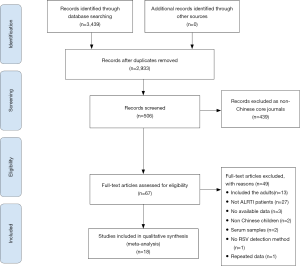
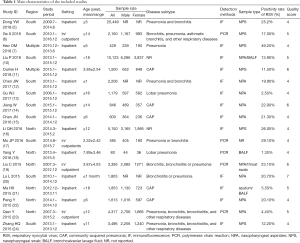
After the literature search and subsequent eligibility screening, 18 articles (5-7,10-24) comprising 66,799 ALRTIs cases were finally included in the meta-analysis. Figure 1 details the study selection process. The eligible articles were published between January 1, 2015 and December 31, 2018, with study periods ranging from January, 2006 to December, 2016. Of these studies, 6 were published in English (6,10,11,14,19,20) and the other 12 in Chinese. The ALRTIs cases were diagnosed as community-acquired pneumonia (CAP), lobar pneumonia, bronchitis, bronchiolitis, or other lower respiratory diseases. Respiratory specimens collected to test for RSV infection included nasopharyngeal aspirates (NPA), nasopharyngeal swabs (NPS), and BALF. RSV infections were assessed using immunofluorescence assays or polymerase chain reaction. All of the selected articles were of moderate quality according to the AHRQ recommended item checklist. Table 1 presents the characteristics and quality scores of all of the included studies.
Full table
Overall analysis
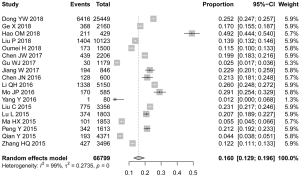
The positive rate of RSV infection among Chinese children in the enrolled studies ranged from 1.2% to 49.2% (Figure 2). In a pooled sample of the 66,799 ALRTI patients involved, the overall positive rate of RSV infection was 16.0% (95% CI: 12.9–19.6%). Substantial heterogeneity presented for combined effect size (Ph<0.01, I2=99.0%) (Table 2). Consequently, subgroup analysis was performed to explore the potential source of this heterogeneity.
Full table
Subgroup analysis
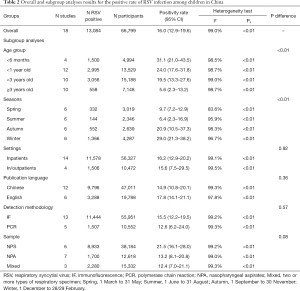
The detection rates for RSV infection varied considerably between groups of different age distributions, and decreased as the age rose (Table 2). Stratified analysis revealed that RSV infection was more frequently detected in children aged <3 years (19.5%, 95% CI: 13.3–27.6%) than in those aged ≥3 years (5.6%, 95% CI: 2.3–13.2%; P<0.01). Furthermore, the highest rate of RSV infection appeared among children <6 months (31.1%, 95% CI: 21.0–43.5%).
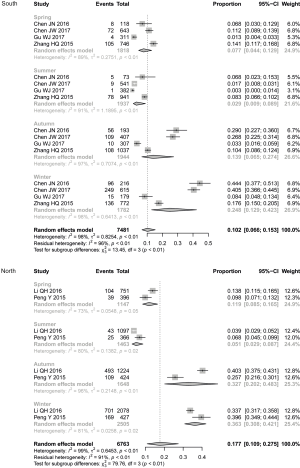
There were 6 studies that accounted for the seasonality of RSV infections (12,13,15,16,22,24). Our subgroup analysis showed that the positive rate of RSV infection was significantly associated with season. Winter had the highest rate (29.0%, 95% CI: 21.3–38.2%), followed by autumn (20.9%, 95% CI: 10.5–37.3%), while summer had the lowest rate (6.4%, 95% CI: 2.3–16.9%) (Table 2). When stratified according to location (southern and northern China), the seasonality characteristics of RSV infection still existed (Figure 3). Clear seasonal peaks occurred in winter (South: 24.8%, 95% CI: 12.9–42.3%; North: 36.3%, 95% CI: 30.8–42.1%) and autumn (South: 13.9%, 95% CI: 6.5–27.4%; North: 32.7%, 95% CI: 20.2–48.3%). Two studies (12,16) reported monthly isolation rates. There was an obvious increase in the positive detection rate for RSV infection from September, peaking in November (49.4%, 95% CI: 29.0–70.0%). Meanwhile, June had the lowest positive rate of RSV infection (1.3%, 95% CI: 0.6–2.8%) (Figure 4). No obvious differences were found by stratification according to study settings, publication language, detection methodology, and sample type. The main results are summarized in Table 2.

Sensitivity analysis and publication bias
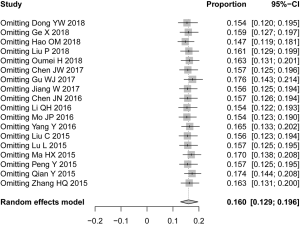
The overall results were not obviously changed after each individual study was omitted, which confirmed the stability of the results of our meta-analysis (Figure 5). Moreover, calculated the pooled proportion of studies with moderate-poor quality (scoring 4), and the results were not substantially different (19.0%, 95% CI: 15–24%). Egger’s linear regression test was performed to test for publication bias, and no obvious publication bias was detected (P=0.06) among the publications that reported RSV positive rates for all patients.
Discussion
We conducted a meta-analysis to pool the positive rate of RSV infection among children with ALRTIs in China. After rigorous screening, 18 articles including 66,799 ALRTI cases were deemed to be eligible and included in the meta-analysis. Among these patients, the overall positive rate of RSV infection was 16.0% (95% CI: 12.9–19.6%). Moreover, RSV infection was significantly associated with season and age.
The prevalence of RSV infections among ALRTI patients varies in different countries around the world. For instance, a meta-analysis of 67 studies involving 154,000 ALRTIs participants showed that the pooled prevalence of RSV infection was 14.6% (95% CI: 13.0–16.4%) in Africa, and found that RSV prevalence was not associated with gender, study setting, seasonality, or subregion (25). In their meta-analysis of 74 studies, Bardach et al. (26) found that the pooled percentage of RSV infection in LRTI patients varied between children (41.5%) and elderly people (12.6%) in Latin America. Another meta-analysis with 4,140 cases, yielded a prevalence of 18.7% in Iran (27). Zhang et al. (4) explored RSV prevalence and clinical manifestations of RSV infection-related ALRTI and discovered that the overall positive rate of RSV in patients with ARTIs was 18.7% (95% CI: 17.1–20.5%). In our meta-analysis, 13,084 (16.0%) of 66,799 cases were positive for RSV infection. The positive rates of RSV infection for the included studies ranged from 1.2% to 49.2%. The considerable discrepancy between these rates might be attributed to the different years in which the analyses were conducted and differences in the study populations. During sensitivity analysis, each study was omitted in turn, and no substantial change was observed in the overall estimates, even when the study with the lowest positive rate was removed.
In both developed and developing countries, RSV infections are one of the major causes of hospitalizations and in-hospital deaths among children (2,3). In this meta-analysis, we attempted to obtain a comprehensive epidemiological picture of RSV infection among children in China from the data available. Our results show that RSV infection was most frequently detected in children younger than 6 months (31.1%, 95% CI: 21.0–43.5%). From this finding, it can be concluded that infants have higher susceptibility to RSV, and efforts to prevent RSV infections among infants may help to reduce the associated medical costs in China. As for prognosis, hypoxemia is an important risk factor of Children ALRTI. About 20% of all children admitted to hospital with RSV-ALRI have hypoxemia. Moreover, our results showed that the detection rate of RSV varied by season and was highest in winter. With regional variations taken into consideration, the seasonality characteristics of RSV infection in southern and northern China were analyzed, and similar results were obtained. It is well known that changes in climate in the winter, like wet and cold weather, are key elements affecting pathogen transmission. We also reported the distribution of the monthly detection rate for RSV infection among Chinese children, but these results need further verification in future studies covering more comprehensive information. Although PCR-based diagnostic testing is more sensitive than other methods for detecting respiratory viruses, immunofluorescence assay was used for RSV detection in the majority of the included studies. No significant difference was found between the two methods for RSV detection, which was consistent with the findings of Zhang et al. (4).
This study had some limitations that should be noted when applying its findings. First, the identified eligible articles were published between January, 2015 and December, 2018, but the study periods ranged from January 2006 to December 2016. Moreover, due to limited data, the annual positive rate of RSV infection could not be evaluated. Second, substantial heterogeneity existed between the enrolled studies. Limited information restricted further evaluation on risk factors such as patients’ gender, severity, and subtypes of ALTIs, which may have been sources of the heterogeneity. Third, the retrospective nature of this meta-analysis means that it is subject to any methodological deficiencies of the included studies. Fourth, the participants in all of the included studies were enrolled from hospitals, so they might not be representative of the general population. Fifth, there are some well-known risk factors associated with RSV infection such as premature birth, chronic lung disease, and congenital heart disease (28). Due to insufficient data in the original studies, we could not extract the relevant data to perform subgroup analysis of children with congenital heart disease, down syndrome, preterm birth, and other chronic conditions with impairment of lung function.
Despite the above-mentioned limitations, this study has a number of strengths. Relevant reports were identified through a systematic search strategy and selected according to predefined inclusion criteria, which ensures the reliability and scientific nature of this work. Moreover, subgroup and sensitivity analyses were performed to explore potential sources of heterogeneity and to test the stability of the results. The results of sensitivity analysis were similar to those of the overall analysis, thus indicating the robustness of our findings.
Conclusions
Our meta-analysis showed that the distribution of RSV-associated ALRTIs in Chinese children varies with age and season. Further studies to identify RSV-associated ALRI mortality (in community and hospitals) are called for. Moreover, regional estimates of the burden of RSV infection on health-care systems are required to develop policies for the introduction of RSV vaccines as well as to assess the effect of these vaccines on the rates of morbidity and mortality in young children.
Acknowledgments
We would like to thank all of the people involved in our study.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/tp-20-148
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-20-148). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mizgerd JP. Acute lower respiratory tract infection. N Engl J Med 2008;358:716-27. [Crossref] [PubMed]
- Tao Y, Tang M, Luo L, et al. Identification of etiologic agents and clinical characteristics for patients suspected of having pertussis in a large Children’s Hospital in China. Ann Transl Med 2019;7:443. [Crossref] [PubMed]
- Gkentzi D, Dimitriou G, Karatza A. Non-pulmonary manifestations of respiratory syncytial virus infection. J Thorac Dis 2018;10:S3815-8. [Crossref] [PubMed]
- Zhang Y, Yuan L, Zhang Y, et al. Burden of respiratory syncytial virus infections in China: Systematic review and meta-analysis. J Glob Health 2015;5:020417. [Crossref] [PubMed]
- Dong YW, Dai LH, Ye WJ, et al. Molecular Epidemiology of Respiratory Syncytial Virus in Southern Zhejiang from 2009 to 2014. Zhongguo Dang Dai Er Ke Za Zhi 2018;20:904-10. [PubMed]
- Ge X, Guo Y, Chen J, et al. Epidemiology and Seasonality of Respiratory Viruses Detected from Children with Respiratory Tract Infections in Wuxi, East China. Med Sci Monit 2018;24:1856-62. [Crossref] [PubMed]
- Hao OM, Wang XF, Zhao M, et al. Analysis of pathogens in 429 pneumonia children. China Journal of Traditional Chinese Medicine and Pharmacy 2018;33:1353-6.
- The Library of Perking University. Chinese core journals (2017 edition). Available online: http://www.zzqklm.com/w/hxml/23761.html. Accessed: 2 November 2018.
- Ma LL, Wang YY, Yang ZH, et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 2020;7:7. [PubMed]
- Liu P, Xu M, He L, et al. Epidemiology of Respiratory Pathogens in Children with Lower Respiratory Tract Infections in Shanghai, China, from 2013 to 2015. Jpn J Infect Dis 2018;71:39-44. [Crossref] [PubMed]
- Oumei H, Xuefeng W, Jianping L, et al. Etiology of community-acquired pneumonia in 1500 hospitalized children. J Med Virol 2018;90:421-8. [Crossref] [PubMed]
- Chen JW, Gu WJ, Zhang XX, et al. Comparison of clinical features between respiratory syncytial virus and human rhinovirus lower respiratory tract infection in infants between 2013-2015 in Suzhou. Chinese Journal of Applied Clinical Pediatrics 2017;32:1239-43.
- Gu WJ, Zhang XX, Chen ZR, et al. Etiological analysis of lobar pneumonia in hospitalized children in Suzhou area from 2006 to 2015. Chinese Journal of Infectious Diseases 2017;35:93-8.
- Jiang W, Wu M, Zhou J, et al. Etiologic spectrum and occurrence of coinfections in children hospitalized with community-acquired pneumonia. BMC Infect Dis 2017;17:787. [Crossref] [PubMed]
- Chen JN. Analysis of the etiological characteristics of community-acquired pneumonia in 600 children. Journal of Parasitic Biology 2016;11:1126-30.
- Li QH, Gao WJ, Li JY, et al. Detection of respiratory viruses in children with acute lower respiratory tract infection: an analysis of 5150 children. Zhongguo Dang Dai Er Ke Za Zhi 2016;18:51-4. [PubMed]
- Mo JP, Pan W. Analysis of the characteristics of viral etiology in 585 cases of children with an acute lower respiratory tract infection. Journal of Parasitic Biology 2016;11:79-81,86.
- Yang Y, Zhang W, Wang YX, et al. Analysis of pathogen in bronchoalveolar lavage fluid and its clinical features in 80 children with lobar pneumonia. Journal of Clinical Pediatrics 2016;34:348-50.
- Liu C, Xiao Y, Zhang J, et al. Adenovirus infection in children with acute lower respiratory tract infections in Beijing, China, 2007 to 2012. BMC Infect Dis 2015;15:408. [Crossref] [PubMed]
- Lu L, Yan Y, Yang B, et al. Epidemiological and clinical profiles of respiratory syncytial virus infection in hospitalized neonates in Suzhou, China. BMC Infect Dis 2015;15:431. [Crossref] [PubMed]
- Ma HX, Sun L, Wu XR, et al. The etiology of community-acquired pneumonia in hospitalized children of single center in Beijing. Chinese Journal of Evidence Based Pediatrics 2015;10:361-5.
- Peng Y, Shu C, Fu Z, et al. Pathogen detection of 1613 cases of hospitalized children with community acquired pneumonia. Zhongguo Dang Dai Er Ke Za Zhi 2015;17:1193-9. [PubMed]
- Qian Y, Xie Z, Ren L, et al. Detection and clinical analysis of human coronavirus in children with acute lower respiratory tract infection in Beijing from 2007 to 2015. Zhonghua Er Ke Za Zhi 2015;53:707-11. [PubMed]
- Zhang HQ, Yu XZ. Viral etiology analysis of 3496 hospitalized children with lower respiratory tract infection. Modern Preventive Medicine 2015;42:437-439,444.
- Kenmoe S, Bigna JJ, Well EA, et al. Prevalence of human respiratory syncytial virus infection in people with acute respiratory tract infections in Africa: A systematic review and meta-analysis. Influenza Other Respir Viruses 2018;12:793-803. [Crossref] [PubMed]
- Bardach A, Rey-Ares L, Cafferata ML, et al. Systematic review and meta-analysis of respiratory syncytial virus infection epidemiology in Latin America. Rev Med Virol 2014;24:76-89. [Crossref] [PubMed]
- Salimi V, Tavakoli-Yaraki M, Yavarian J, et al. Prevalence of human respiratory syncytial virus circulating in Iran. J Infect Public Health 2016;9:125-35. [Crossref] [PubMed]
- Fattouh AM, Mansi YA, El-Anany MG, et al. Acute lower respiratory tract infection due to respiratory syncytial virus in a group of Egyptian children under 5 years of age. Ital J Pediatr 2011;37:14. [Crossref] [PubMed]
(English Language Editor: J. Reynolds)