
Home-based health management needs of children with type 1 diabetes mellitus in China: an information platform-based qualitative study
Introduction
Type 1 diabetes mellitus (T1DM) affects approximately 500,000 children (<15 years) worldwide. With around 80,000 new cases diagnosed each year, T1DM has an annual increment rate of about 3.0% (1) . Pediatric T1DM patients in China have an average HbA1c value of 8.6−10.3% (2), and only 27.5% of these patients achieve qualified blood glucose control (3). Even in developed Western countries, the average HbA1c value is only 8.3−9.1% (4), which reflects the rarity with which children with T1DM achieve a ‘good’ standard of blood glucose control, despite advancements in technology. T1DM management needs adherence to a strict diet and insulin therapy 365 days per year. Optimal management necessitates adapting therapeutic regimens to different situations (5). One of the key challenges is helping patients and their families integrate diabetes into their everyday life (6). Most children’s time is spent at home or at school, so both environments (e.g., food eaten, exercise, sleep schedules) have a marked influence on blood glucose control and the concomitant necessity for insulin treatment (7). As the result of that, children with T1DM have been identified as a difficult age group to treat, especially school-age patients (4). In one control and complication trial, it stated that school-aged T1DM patients had the worst glycemic control because of increased caloric intake, a decline in physical activity and poor self-management (8). Home-based health management for patients with chronic disease based on information platforms can improve patient quality of life (9). The WeChat platform, for instance, allows access to online health information and education at any time, providing caregivers with the means of obtaining vital information as the need arises (10). However, the information quality of these platforms can only be improved by identifying the challenges frequently encountered by patients and caregivers. This study examined the problems faced by caregivers and patients in the home-based management of pediatric T1DM to provide improved professional health guidance on information platforms.
Methods
Design
This research adopted phenomenological research methods to perform qualitative analysis. Data was collected from the T1DM Doctor-Patient Communication WeChat Platform using a standardized literature review method (11), and the questions and comments from parents (or primary caregivers) on home-based health management were analyzed to identify common themes and content according to literature analysis procedures.
Data collection
A total of 10,938 original messages sent by 104 parents of pediatric T1MD patients between October 1, 2016 and September 30, 2017, were collected from the T1DM Doctor-Patient Home-Based Disease Management Communication Platform of a Class A tertiary specialized children’s hospital in Shanghai, China. Parents who expressed interest were screened for eligibility. Once consent was obtained, the parents were asked a series of questions about home-based management focusing on a retrospective look at their experience of taking care of children with T1DM (Table 1). They answered these questions in the WeChat platform. A total of 6,311 messages along with the information related to T1DM home-based disease management were analyzed according to literature analysis procedures.
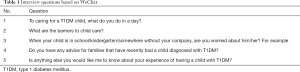
Full table
Data analysis
The data were analyzed according to the six steps of literature analysis: (I) problem identification: the purpose of this research was to identify problems in the home-based health management of children with T1DM. (II) Assumption drafting: we assumed that many problems exist in the home-based health management of pediatric T1DM, but that the specific problems are not defined, so all potentially relevant questions and comments should be included in the analysis. (III) Early preparation: we published the related statement on the WeChat T1DM Group to obtain the consent of the respondents (via message reply), and obtained the approval of the hospital’s ethics committee. We defined the research period as October 1, 2016 to September 30, 2017. (IV) Data collection: the WeChat messages sent by all parents in the WeChat T1DM Group within the research period were used as the primary sources and were collected by two researchers. (V) Data analysis: the data were preliminarily screened by the two researchers, and the messages irrelevant to the research theme were deleted, respectively. The researchers examined the retained messages, and after confirming there were no errors, omissions, or duplicates, jointly analyzed the data. (VI) Data induction: the two researchers jointly repeatedly read the data to identify the problems commonly encountered in the home-based disease management of pediatric T1DM patients. Finally, 16 problems in 5 themes were identified.
Integrity
The research team comprised 10 endocrinology specialist physicians, 4 diabetes mellitus specialist nurses, and 1 nutritionist, who helped to guarantee the accuracy and reliability of the data. The researchers all participated in the diagnosis, treatment, and nursing of T1DM patients, and had been in communication with the respondents for a long period of time prior to the commencement of the study, so they had gathered a good understanding of the cultural backgrounds and language styles of the patients and parents . To guarantee authenticity, respondents were asked to clarify any communications for which there were differences in opinion among the researchers during data analysis.
Ethics
The research protocol was examined and approved in writing by the Ethics Committee of the Children’s Hospital of Shanghai (approval number 2017R012-E01). Written informed consent for the publication of anonymized quotes was obtained from all of the respondents.
Results
Demographic data
The respondents were 104 parents or other family members of 68 children aged between 6 and 18 years old who met the diagnostic criteria for T1DM. Of the respondents, 61 (58.65%) were the patients’ mothers, 41 (39.42%) the fathers, and 2 (1.92%) were other family members.
Home-based health management need
Through data analysis, the 16 most frequent home-based health management problems of T1DM children were identified and classified into 5 themes (Table 2).
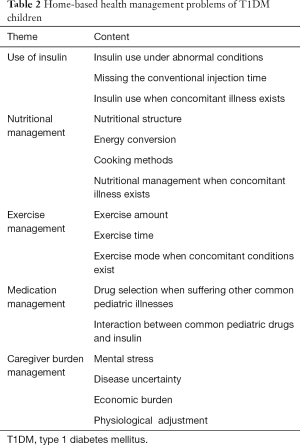
Full table
Use of insulin
Insulin use under abnormal conditions
During insulin control, patients frequently exhibit irregular blood glucose (sudden hyper- or hypoglycemia) due to changes in diet or work-rest habits. Parent 003: “If blood glucose is low before sleep, should I ask my child to drink some milk or eat some cookies to prevent hypoglycemia in the morning?” Parent 004: “Sometimes the blood glucose level is higher before sleep after a greasy evening meal, so I consider increasing the injection dose of insulin before sleep. Is that right?” Parent 005: “Sometimes my child gets up late at the weekend, so we inject insulin just before sleep to guarantee the insulin is sufficient during sleep. I am not sure if this is right or not.” Parent 041: “When my child goes on an outing in the spring/autumn, we inject the insulin in the morning before lunch to avoid having to inject at noon, but we keep the night injection the same. Is this OK?”
Missing the conventional injection time
When the patient misses the conventional injection time, parents often do not know how to deal with it. Parent 006: “Doctor, our child just went out, he missed our meal time and his insulin injection. What should we do?” Parent 007: “My child gets up late during the holidays. We inject the same dose of insulin, but the mealtime is later. Is this OK?” Parent 042: “Sometimes we have supper later than usual, but we have to inject the intermediate-acting insulin four hours later, so we let the child sleep for a while first, and then inject the insulin at the right time. Do you do this, too?” Parent 027: “If we forget to inject the long-acting insulin at night, should we give a supplementary shot the next morning?”
Insulin use during concomitant illness
When pediatric T1DM patients have a cold or suffer inflammatory reactions, their blood glucose level is higher. Parent 005: “When our child has a cold, their blood glucose increases to a particularly high level, and it is difficult to know what insulin dose to give.” Parent 014: “When our child has a cold, they have a higher blood glucose level. We supplement a quick-acting insulin, but we do not know whether a dose of long-acting insulin needs to be given at nighttime or not.” Parent 058: “When our child has a cold, we give an extra injection, but the measured blood glucose is still high.” Parent 039: “My child has been vomiting for several days and does not want to eat. Should we measure the blood glucose first, and then use insulin according to the blood glucose level?”
Nutritional management
Nutritional structure
Families have different attitudes towards diet, and most caregivers still express that they do let their children eat certain kinds of food. Parent 057: “I haven’t let my child eat a banana since they were diagnosed with this disease because I am worried that bananas will increase their blood glucose to a higher level.” Parent 059: “I strictly control my child’s diet at present. I seldom give them fruit, and especially not bananas or oranges. Dragon fruit and kiwi fruit are the fruits we eat the most.” Parent 003: “I let my child eat whatever he wants, but he has to eat breakfast and lunch, and not too large an amount – an appropriate small amount is good.” Parent 068: “My child always eats according to the normal amount, to support his development. But we never give him snacks, and eating fruit greatly increases his blood glucose level, so we don’t allow him to eat it.” Parent 072: “I cook a different lunch every day. I want her to try every food I can make, so we can find out what food is safe.”
Energy conversion
Many parents do not know how to accurately convert energy and distribute the carbohydrates allowed in a day among meals to maintain steady blood glucose. Parent 003: “I want give my child various fruits, but I don’t know how to replace carbohydrates, and on the spur of the moment, I calculate the carbohydrate amount of snacks according to the outer package when she wants to eat.” Parent 010: “When my child was young, I used to weigh the rice and extra fruits. Now that he is growing up, I have stopped weighing the rice and have changed to visual measurement, and I give him an appropriate amount of other food.” Parent 057: “As parents, we know more about the acting time of insulin, so our child can eat whatever he wants if the food matches the insulin.”
Cooking methods
Even if the foods are the same, different cooking methods can influence blood glucose. Parent 010: “I often make different breakfasts for my child, and I find that fermented flour is more likely to increase blood glucose than unfermented flour. I really don’t know why this is.” Parent 002: “The carbohydrate ratio in flour is almost the same as in rice, and the blood glucose increases slowly if a lot of oil is added and increases faster with less oil.” Parent 068: “In my house, each meal contains 8 g of oil, and if I add oil to salad, I put less oil in the other dishes.” Parent 003: “Sugar-free food is useless; the key is carbohydrate content.”
Nutritional management during concomitant illness
Parents are more cautious with the child’s diet during concomitant illness. Parent 045: “When my child got fever or cold, we hardly ever give him medicine. Instead, we give him some chrysanthemum tea or orange peel water to drink.” Parent 003: “When my child is sick, I make him have some porridge even if he has no appetite, and then give the medicine or injection as usual.” Parent 027: “When my child catches a cold, his blood glucose is higher. I make some bitter gourd for him.” Parent 044: “When my child catches a cold, I make foreign ‘cold tea’ for him. This is not a drug, and I don’t know whether it is useful, but it does not influence blood glucose.”
Exercise management
Exercise amount
Most caregivers recognize the importance of appropriate exercise for blood glucose control, but there are still some parents who worry that strenuous exercise will cause hypoglycemia. Parent 057: “At present, our child does not take medicine or insulin, and we control his blood glucose through his diet and exercise.” Parent 005: “My child takes part in long-distance running in PE class, but I won’t allow him to sprint which with heavy amount of exercise” Parent 026: “My child does not attend PE class, but we allow him to ride a bicycle and play badminton at home. But I really don’t know how long I should allow him to ride or play?” Parent 019: “We know that children can do some aerobic exercise that isn’t too strenuous, such as jogging and walking, and we also allow swimming. Is that OK?”
Exercise duration
Knowing the appropriate duration period for each type of exercise is also problematic for parents. Parent 026: “Back when my child was just falling ill, we used to jog for several kilometers every day. But now, although it takes only thirty minutes to get to school every day, I’m afraid he will be too tired and drive him.” Parent 019: “We basically let our child exercise during PE class, which lasts for about 40 minutes, and we allow him to attend every PE class. But the teacher was afraid that this would cause him problems, so he did not let him do the entire course.” Parent 010: “We allow our child to exercise normally, as well as to play basketball or football with the other boys, but only for a short amount of time. Now, the problem is that his playmates tease him and make him feel inferior if he quits halfway. I don’t know what to do about it.”
Exercise mode when colds or allergies exist
Concomitant conditions can cause large fluctuations in blood glucose, and some parents cannot accurately adjust the insulin amount, so they choose exercise as an auxiliary mode of blood glucose regulation. Parent 068: “When my child has a cold, his blood glucose can easily increase, so we let him exercise more to decrease it.” Parent 044: “If the blood glucose is higher after eating too much or eating a greasy supper, we will let our child go out and do some exercise before sleep.” Parent 045: “My child has allergies, and his blood glucose increases when his allergies flare up, so we let him do more exercise to prevent his blood glucose from increasing.”
Medication management
Selecting drugs for common illnesses
The immune systems of pediatric T1DM patients are not fully developed, making them more likely to suffer from colds or other concomitant illnesses. During this period, the child’s blood glucose will often fluctuate. Therefore, parents have the additional problem of choosing medicines for the concomitant disease that will avoid exacerbating blood glucose fluctuations. Parent 027: “Our child is very young, so we buy ibuprofen liquid medicine when she catches a cold or has a fever. But I don’t know if it affects her blood sugar.” Parent 068: “Our child caught a cold recently. After taking anti-inflammatory drugs and cold medicine, his blood glucose fluctuated massively, so we dare not give him cold medicine again.” Parent 058: “When our child catches a cold, we give him Pudilan or Child Chiqiao Qingre Granules, and he recovers after several days.” Parent 044: “When our child catches a cold, we give them Meilin together with a fever cooling patch. I think on these occasions, we shouldn’t really care whether blood sugar is affected or not; after all, high fever can cause convulsions.”
Interaction between common drugs and insulin
Medicines for other common illnesses can influence blood glucose in children, so the parents may need to adjust the insulin dose accordingly. Parent 003: “Sometimes after taking the dissolved medicines dispensed by the hospital, the blood glucose increases sharply, so we have to temporarily add some quick-acting insulin.” Parent 068: “Last time our child caught a cold, we bought “999” drug for cold. Their blood glucose increased to an extremely high level after taking one packet, and so we had to inject quick-acting insulin. We will never use that drug again.” Parent 078: “Our child once went out for an autumn outing. We could not measure his blood glucose and inject the insulin, so we left the quick-acting insulin and let him take Metformin orally instead.” Parent 054: “If the blood glucose is stable, and there is no infection, preventive inoculation can normally be given.”
Caregiver burden management
Mental stress
At present, many schools and employers still discriminate against and misunderstand the needs of T1DM patients. Many people believe that T1DM is a genetic disease and that the children will have difficulty finding a spouse or being accepted by the family of their spouse. Parent 048: “Every night, I set my alarm clock to measure my child’s blood glucose level, and I cannot sleep if his blood glucose is unstable.” Parent 061: “My child had only been in the nursery for one and a half months, and was discouraged by the nursery after they found out about the diabetes. I was bitterly disappointed!” Parent 068: “No other children in our town suffer from diabetes, and since finding out my child has this disease, his teachers have shown more attention on him.” Parent 057: “When I registered for a chronic disease card, people watched me with strange eyes.” Parent 062: “I dare not tell other people that my child has diabetes, because I am afraid of frightening them.” Parent 044: “Now, my child plays games about falling ill and taking injections or medicine; she says her toys are sick every day, and I feel devastated when I see this.”
Disease uncertainty
The clinical manifestations of T1DM are complex and diverse, and the lack of typical diabetes symptoms impedes early diagnosis. In addition, clinicians may have insufficient understanding of diabetic ketoacidosis, consider the problem one-sidedly, or fail to consider T1DM in differential diagnosis, leading to misdiagnosis. In turn, caregivers of diabetic children may be unable to accept the illness. Parent 024: “When our child was sent to the hospital for emergency treatment for ketoacidosis, and was then diagnosed with diabetes, I felt like I was dreaming. It didn’t feel real.” Parent 068: “After obtaining the confirmed diagnosis, I have searched various data and considered traditional Chinese medicine and many other methods of regulation, which have turned out to be useless.” Parent 025: “Now, when I see my child losing so much hair, I worry that it is caused by diabetes.” Parent 059: “I was hopeful about recovery at the start, but after fully comprehending this disease, I have no choice but to slowly accept it.” Parent 035: “Sometimes, when I find that the scientists have discovered a new method to treat T1DM on the internet, I hope it is true and can be clinically popularized soon.”
Economic burden
After a diagnosis of T1DM, the child requires hospitalization roughly once every two years on average, with hospitalizations gradually becoming more frequent as the disease progresses. The injection dose of insulin also increases with age, and, consequently, the cost of treatment rises too. The blood glucose level of children with T1DM needs to be every day, and the expenses associated with consumables (testing kits, etc.) further increase the economic pressure on parents. Parent 068: “We have registered a chronic disease card, through which the cost of insulin can be partially reimbursed, and more expense can be reimbursed for hospitalization, so we don’t need outpatient services as much.” Parent 077: “Aside from the instrument for dynamic monitoring, we have to partially pay for the costs of insulin and disposable syringe needles, which amounts to at least 1,000 Yuan every month.” Parent 001: “The insulin our child needs cannot be bought at the county hospital, and we have to travel to Shanghai to buy it.” Parent 068: “The insulin cannot be used up within one month, and the remaining insulin can only be discarded, which is a waste of money.”
Physiological accommodation of caregivers
After gradually accepting their child’s illness, caregivers start to realize that their emotions have an influence on the child’s attitude toward the disease, so they try to maintain an optimistic outlook. Parent 003: “The child sometimes endures more than lots of adults and so the parent needs to be mindful of what they do.” Parent 010: “Actually, our diabetes-suffering child is no worse off than other children. Lots of diabetes-suffering children do really well. They take part in various activities at school, and they are as good as the other children.” Parent 032: “Apart from having to take insulin injections before meals, our child is just a normal child. We know that our moods and attitudes influence our children.” Parent 059: “I also suffer diabetes, and I cry every day that my child is like me. I was in a passive state for a year before walking out of the shadows.” Parent 068: “Now, I feel anxious every day, and I feel I am abnormal too. I have to adjust myself first, and then give better care to my child.”
Discussion
Instruct caregivers to use insulin correctly
After receiving health education from doctors, nurses, and nutritionists, most caregivers of T1DM patients understand the importance of insulin in blood glucose control and can inject insulin according to the doctor’s recommendation. However, children and adolescents with T1DM are in important stages of physiological and psychological transition (12). Hormonal changes, body growth, changing diet preferences, changing sleep-wake schedules, and disease progression as well as other concomitant conditions can all influence blood glucose, so controlling blood glucose in this population is particularly challenging. When the child’s blood glucose fluctuates abnormally by a large margin, caregivers generally feel at a loss and cannot determine the correct dose or take other appropriate treatment measures to control it. Therefore, the medical staff could be responsible for teaching the caregivers to inject insulin at the right time with the appropriate dose and type of insulin. It can avoid the large fluctuations of blood glucose and help caregivers to use insulin in a correct way. The frequency of blood glucose measurement should be increased to avoid hypoglycemia. Additionally, the instructions of insulin use need to be further refined and improved, and can be sent to the caregivers through WeChat platform as an evidence when they have questions.
Formulate individualized recipe
China Medical Nutrition Therapy Guideline for Diabetes defines nutritional management objectives as ‘balancing the diet and rational nutrition requirements, and under the premise of guaranteeing the appropriate energy supply ratio of macronutrients, formulating individualized diet structure in combination with the metabolism goal and personal preference of the patient, controlling the blood glucose and blood fat, supplementing high-quality protein, reducing the load of pancreatic β cells, and controlling the occurrence and progress of diabetic complications’ (13). This study reveals that the biggest difficulty in home-based diet management of children with T1DM is calculating the right amount of food to serve. Currently, diabetic diet education mainly focuses on calculating carbohydrates. Research shows that maintaining the same total amount of carbohydrates ingested at each meal can keep blood glucose stable, especially after-meal blood glucose, and can increase food choices (14). However, each child has different insulin requirements and sensitivity, which may result in great differences in response (15), so caregivers are required to closely monitor the child’s blood glucose changes following the ingestion of certain foods, and adjust the child’s diet based on experience. Only in this way can the child develop good nutritional habits. Persisting with such habits is beneficial to controlling the illness as well as the growth and development of the child. Children are prone to develop rebellious attitudes toward disease treatment and, therefore, may not comply with nutritional advice. Age, stage of development, disease severity, and psychological and physiological characteristics must be considered when formulating a child’s diet plan (16).
Instruct individualized exercise
Exercise duration, intensity, and frequency interact to influence blood glucose. Regular exercise confers many benefits to pediatric T1DM patients, including the promotion of better blood glucose control, growth and development, and physiological adaptability (17). To date, no specific exercise guidelines have been devised to assist parents and T1DM children with maintaining blood glucose at or close to the normal range during exercise (17). According to this analysis, caregivers implement different limits on duration and modes of exercise at home. The exercise duration and mode most suitable for the child can be established after repeated trials, thus maintaining the blood glucose within a normal range. Therefore, the child’s exercise regimen must be individualized, and each child should try regimens of different intensity and duration to achieve the best effects on blood glucose regulation. The total amount of exercise (duration × intensity × frequency) should be determined based on age and individual experience, and it is suggested that a trial-and-error method be used to find the optimal mode, duration, and intensity most suitable for each child (18).
To help select the right medication for the associated disease
This study showed that caregivers lack of experience of medication using when T1DM patients with other diseases. When children with T1DM are accompanied by other diseases, their blood glucose often fluctuates. If they take medications blindly, their blood glucose is not easy to control. Through the WeChat platform, caregivers can inform the medical staff the condition change immediately so that the medical staff can give the response in real time. Or the medical staff can ask them to the hospital to avoid delayed treatment. After medication, it guides the caregivers to use insulin to control blood glucose.
Caregivers support
Caring for a child with T1MD carries a physical, economic, and psychological burden (19). Children and adolescents may develop a rebellious attitude toward treatment and caregivers, which may be compounded by shame. This can negatively influence disease control behavior and place an additional burden on the caregiver. Caregivers may encounter problems acquiring, understanding, mastering, and applying disease-related information. Indeed, “financial difficulty”, “mental stress”, “other non-care-based responsibilities” and “sleep disorders” were prevalent problems reported by caregivers. In families, childcare is mainly the responsibility of the mother. When other family members cannot comprehend a child’s condition, or when a child’s condition is misunderstood or discriminated against by society or at school, mothers are more likely to generate negative emotions. The high long-term cost of medical care is a heavy burden for most families reliant on full self-payment. In the WeChat platform, all caregivers can empathize with each other. When caregivers show negative emotions, other caregivers can give support to them. It was stated that family behavior intervention can improve blood glucose control and the quality of life. It was suggested that the medical staff could talk with caregivers with relaxed and humorous language in order to alleviate the stress of caregivers. Other family members are also encouraged to participate in the home-based management, promote mutual understanding between family members and cooperation.
Limitations
Due to the characteristics of qualitative study, the sample size of this study was limited. Firstly, the participants included were who used WeChat platform and in our WeChat group. The experiences of other caregivers with T1DM children need to be further explored. Secondly, this study was a single-centered study, multi-centered studies including quantitative and qualitative methods about T1DM home-based management are needed in the future. Additionally, opportunities for future research in this area are numerous, especially because the management of chronic disease in pediatrics can be an eternal topic. This study took an inductive approach, a deductive approach using a quantitative instrument would increase the generalizability of these findings and further our understanding of what factors are relevant to outcomes of children with T1DM.
Conclusions
This study summarized the experiences of home-based disease management among T1DM patients’ caregivers through the WeChat platform. The major problems encountered by caregivers in home-based disease and health management of pediatric T1DM in China are appropriate insulin adjustment in cases of abnormal blood glucose, nutritional control and management, controlling the mode of exercise, drug selection, combining the use of different drugs, and the psychological burden of the child’s illness. Professional health guidance of these problems is stated in this study which can be sent through WeChat. The evaluation of home-based management of pediatric T1DM is the goal of our further research.
Acknowledgments
Funding: The study was supported by National Natural Science Foundation of China (NSFC) (No. 71774117) and Shanghai Municipal Education Commission-Gaoyuan Nursing Grant Support (No. hlgy16051kygg).
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tp-20-118
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-20-118). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The research protocol was examined and approved in writing by the Ethics Committee of the Children’s Hospital of Shanghai (approval number 2017R012-E01). Written informed consent for the publication of anonymized quotes was obtained from all of the respondents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Castellanos L, Tuffaha M, Koren D, et al. Management of Diabetic Ketoacidosis in Children and Adolescents with Type 1 Diabetes Mellitus. Paediatr Drugs 2020;22:357-67. [Crossref] [PubMed]
- Li J, Yang D, Yan J, et al. Secondary diabetic ketoacidosis and severe hypoglycaemia in patients with established type 1 diabetes mellitus in China: a multicentre registration study. Diabetes Metab Res Rev 2014;30:497-504. [Crossref] [PubMed]
- Maksoud AA, Sharara SM, Nanda A, et al. The renal resistive index as a new complementary tool to predict microvascular diabetic complications in children and adolescents: a groundbreaking finding. Ann Transl Med 2019;7:422. [Crossref] [PubMed]
- Guo J, Whittemore R, Grey M, et al. Diabetes self-management, depressive symptoms, quality of life and metabolic control in youth with type 1 diabetes in China. Journal of Clinical Nursing 2013;22:69-79. [Crossref] [PubMed]
- Landau Z, Lebenthal Y, Boaz M, et al. Observational study of diabetes management in type 1 diabetic school-age children during holiday versus school days. J Pediatr Endocrinol Metab 2013;26:1083-6. [Crossref] [PubMed]
- Channon S, Hambly H, Robling M, et al. Meeting the psychosocial needs of children with diabetes within routine clinical practice. Diabet Med 2010;27:1209-11. [Crossref] [PubMed]
- Gupta OT, MacKenzie M, Burris A, et al. Camp-based multi-component intervention for families of young children with type 1 diabetes: A pilot and feasibility study. Pediatr Diabetes 2018;19:761-8. [Crossref] [PubMed]
- Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. J Pediatr 1994;125:177-88. [Crossref] [PubMed]
- Wang Y, Meng Z, Huang Y, et al. Application of network platform tracking management in the continuous nursing of type 1 diabetes mellitus adult patients. Chinese Journal of Nursing Education 2016;13:655-8.
- Luo Z. Analysis of the role and application of physical examination center building Wechat Official Platform for Health Education. China Health Industry 2014;(36):132-3.
- Colaizzi P. Psychological research as the phenomenologists view it. New York: Oxford University Press, 1978:48-71.
- Elissa K, Bratt EL, Axelsson ÅB, et al. Societal norms and conditions and their influence on daily life in children with type 1 diabetes in the West Bank in Palestine. Journal of Pediatric Nursing 2017;33:16. [Crossref] [PubMed]
- Chinese Diabetes Society, Dietician Specialized Committee of Chinese Medical Doctor Association. China Medical Nutrition Therapy Guideline for Diabetes (2010). Beijing: People’s Military Medical Press, 2010:121.
- Lopes Souto D, Lopes RE. Use of carb counting in the nutritional treatment of diabetes mellitus. Nutr Hosp 2010;25:18-25. [PubMed]
- Chinese Diabetes Society. Chinese Type 1 Diabetes Mellitus Diagnosis and Treatment Guideline: Insulin Therapy, Medical Nutrition Therapy, Exercise Therapy, and Other Therapies. Chinese Journal of the Frontiers of Medical Science 2013;5:48-56.
- Mao F, Li D. Nutrition therapy for type 1 diabetes mellitus children and adolescents. Chinese Journal for Clinicians 2015.9-12.
- Du K, Kuang H. Blood glucose management of type 1 diabetes mellitus patients when exercising. Diabetes World 2015;9:572-6.
- Li F, Liang X, Gong C. Exercise therapy for type 1 diabetes mellitus. Diabetes World 2015;9.
- Gui Y, Hai J, Jin S. Main caregiver burdens and their influencing factors of type 1 diabetes mellitus patients. Chinese General Practice Nursing 2016;14:902-5.


