Neonatal rhabdomyosarcoma: an unusual presentation
Introduction
Rhabdomyosarcoma (RMS) is a malignant mesenchymal neoplasm that exhibits striated muscle differentiation. It is the most common soft tissue sarcoma of childhood, accounting for 5-8% of all malignant solid tumors in children and third most common extracranial solid tumour of childhood after neuroblastoma and Wilms tumour (1). On the basis of histology RMS has five recognized types: embryonal, botryoid variant, spindle cell variant, alveolar and undifferentiated (2).
We are presenting a rare case of RMS with two very unusual features. First, the patient was a paraneonate and secondly presented as multiple subcutaneous nodules. Multiple skin nodules are present in many malignant and non-malignant conditions also, so it was very difficult to diagnose.
Case
A male baby was born of non-consanguineous marriage to a primigravida mother with normal birth weight. Perinatal period was uneventful. Mother was an unbooked case with no proper antenatal care. Since time of birth parents noticed a small neck swelling along with multiple tiny small swellings all over the body. As a baby was apparently asymptomatic, not much attention was paid to these swellings. After few days mother noticed progressive increase both in size and number of these swellings, especially swelling over neck and eyes.
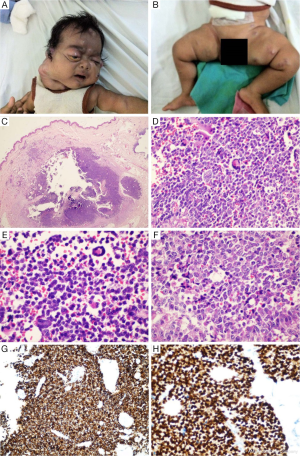
In our hospital, a patient was brought at the age of two months, with large neck swelling and multiple small swellings all over body and unilateral proptosis (Figure 1A,B). There was no history of hoarseness, dysphagia, epistaxis, unilateral nasal discharge, chronic suppurative otitis media, blood tinged ear discharge, hematuria, urinary retention, constipation, abdominal mass or jaundice. On examination, there was a very large 9 cm × 8 cm swelling in the right cervical region extending from right pinna to the midline in suprasternal region. There were also multiple small few mm to few cm sizes nodular, pinkish blue and purple color, shiny subcutaneous swellings all over body including eye swelling, giving the baby a blueberry muffin appearance.
Laboratory investigations like complete blood count, serum electrolytes, serum creatinine and liver function test were with in normal limits. X-ray chest and ultrasonography of abdomen showed no organomegaly and no other intrathorasic or intra-abdominal mass respectively. Such disseminated disease was ruled out.
Biopsy from right para umbilical swelling was taken. Pathological findings in the hematoxylin and eosin sections showed a nodular malignant round cell tumor infiltrating the superficial and deep dermis. The tumor cells showed round nuclei with vesicular nuclear chromatin, prominent nucleoli and eosionophilic cytoplasm, which in some of the cells imparted a distinct rhabdoid look. Intermixed with these tumor cells were seen ‘wreath-like’ giant cells (Figure 1C-F). On immunohistochemistry studies, the tumor cells showed strong cytoplasmic reactivity with Desmin (Figure 1G) and nuclear reactivity with Myogenin (Figure 1H) which confirmed the diagnosis as embryonal RMS.
We managed the patient with chemotherapy, VAC (vincristine, actinomycin D, cyclophosphamide) regime. After two cycles of chemotherapy nodules regressed both in size and number. Unfortunately patient was lost to follow up before completing the treatment.
Discussion
RMS is a common, highly malignant, childhood tumour, which is extremely rare in the neonates and paraneonates; constituting only 1-2% of all childhood RMS (3). There are only a few reports about this tumor in this age group. Of more than three thousand patients registered in the Intergroup Rhabdomyosarcoma Study (IRS) I-IV, only 14 were in the neonatal period at the time of diagnosis, showing rarity at this age group (4). In the first three IRS trials, about 35% to 40% of all tumors originated from the head or neck area, slightly less than 25% from the genitourinary tract, approximately 20% from extremity, 10% from trunk and the remaining 10% from other rare sites (5).
Primary cutaneous alveolar RMS accounts for 0.7% of RMS and tends to arise in the skin of the face (6). Rare cases of congenital alveolar RMS either presenting with multiple rashes or multiple cutaneous metastases have been reported, most with dismal outcome (1). Embryonal RMS presenting as multiple subcutaneous nodule is still a rare entity; even rarer than alveolar RMS. We report herein a case of embryonal RMS, possibly congenital in nature that presented in an unusual fashion and caused a clinical dilemma. Dilemma being to differentiate it from non-malignant causes of blueberry muffin like extramedullary hematopoesis, cutaneous vascular anomalies, langerhans histiocytosis and from other round cell tumors. Thorough literature search could reveal only few case reports mentioning RMS metastasizing to skin at multiple sites (7,8).
The management of childhood RMS includes all the three modalities of cancer treatment that is surgery, chemotherapy and radiotherapy; depending on the risk group to which patient belongs.
According to a review done by Hazime et al. (9), ten-year survival rates for RMS is 86.3% for patients in low-risk subgroup A, 80.7% for low-risk subgroup B, 62.7% for intermediate-risk subgroup A, 61.7% for intermediate risk subgroup B, and 38.1% for the high-risk group.
The correct identification of RMS is a substantial challenge. Using a central review mechanism for patients enrolled in IRS, up to 20% of children enrolled are found to be incorrectly diagnosed with RMS or have their histologic subtype reclassified.
This article emphasizes that in case of a round cell tumor, immunohistochemical studies are mandatory in order to rightly identify the tumor and differentiate amongst various malignancies like RMS, neuroblastoma, malignant lymphoma, small cell carcinoma and primitive neuroectodermal tumor which look similar on histopathological examination.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gong Y, Chao J, Bauer B, et al. Primary cutaneous alveolar rhabdomyosarcoma of the perineum. Arch Pathol Lab Med 2002;126:982-4. [PubMed]
- Lanzkowsky P. eds. Manual of pediatric hematology and oncology 4th ed. Burlington, Mass: Elsevier Academic Press, 2005:561-84.
- Weiss SW, Goldblum JR. Rhabdomyosarcoma. In: Weiss SW, Goldblum JR. eds. Enzinger and Weiss’s soft tissue tumors (4th edition). St Louis: CV Mosby, 2001:785-835.
- Lobe TE, Wiener ES, Hays DM, et al. Neonatal rhabdomyosarcoma: The IRS experience. J Pediatr Surg 1994;29:1167-70. [PubMed]
- Güra A, Tezcan G, Karagüzel G, et al. An unusual localization of embryonal rhabdomyosarcoma in a neonate. Turk J Pediatr 2007;49:82-4. [PubMed]
- Schmidt D, Fletcher CD, Harms D. Rhabdomyosarcomas with primary presentation in the skin. Pathol Res Pract 1993;189:422-7. [PubMed]
- Godambe SV, Rawal J. Blueberry muffin rash as a presentation of alveolar cell rhabdomyosarcoma in a neonate. Acta Paediatr 2000;89:115-7. [PubMed]
- Isaacs H Jr. Cutaneous metastases in neonates: a review. Pediatr Dermatol 2011;28:85-93. [PubMed]
- Hosoi H, Teramukai S, Matsumoto Y, et al. A review of 331 rhabdomyosarcoma cases in patients treated between 1991 and 2002 in Japan. Int J Clin Oncol 2007;12:137-45. [PubMed]


