Case report on a misleading case of appendiceal perforation presented with severe generalized convulsion
Introduction
Acute appendicitis is a common occurrence that affects 5.7 to 57 per 100.000 peoples annually and a large portion of them are children and adolescents (1). Besides this convulsion is often an expected symptom in the case of children for various underlying pathologies and a febrile convulsion is a common neurologic disorder in children (2). But a case of appendicitis led to rupture and peritonitis that presented with generalized convulsion as an early symptom is highly uncommon and has not been reported till now. We describe a misleading case of appendiceal perforation in a young boy who presented with generalized convulsion, almost no abdominal symptoms and had a recent history of minor gastrointestinal problems. Due to the sudden neurological presentation (Generalized convulsion), absence of other complains and the examination along with the laboratory findings the case was primarily diagnosed as a neurological phenomenon. Besides, recent ensuring ultrasound findings also played a role. This patient had no previous or family history of convulsion; no history of severe abdominal pain or other major illness.
Case presentation
A 5-year-old boy was admitted to the Shenmu Hospital Pediatric department on the 16th of July morning with severe convulsion, history of vomiting and fever. He had no family history and no attack of convulsion before this. His recent disease history evaluated that, he had a history of vomiting for 3/4 times associated with mild abdominal pain after having an ice cream one day before on 15th July. He was brought to the pediatric outpatient department on the same day (15th July). His abdomen was soft and mild tenderness and discomforts were noted. The routine blood test evaluated mild neutrophilic leucocytosis. An abdominal ultrasound was performed and revealed no abnormality except Bowel gas. OPD treatment was given with domperidone tablets, and intravenous ceftriaxone sodium, cimetidine and IV fluid. Following treatment, his symptoms were relieved and oral medications were prescribed. But on the 16th July morning at 7:00 am the patient had a fever (39 °C) and severe convulsion. He was brought to the pediatric emergency instantly and was later admitted to the pediatric high dependency unit (HDU). An IV dose of midazolam 2 mg was given to control the convulsion. But as the convulsion continued compound aminophylline barbital injection IM was further administered. Then the convulsion gradually subsided. Other than the convulsion the patient was lethargic with poor appetite; no history of trauma, rash; no presenting complain of diarrhea or vomiting, abdominal pain, and breathing difficulty. Differential diagnosis was included febrile convulsion, viral meningitis, Epilepsy, and Hyponatremia.
On general examination, all the neurological findings were found intact. He was feverish (Temperature 39.1 °C), Pulse: 140 times/min; Respiration: 36 times/min; Weight: 22 kg and Bp: 96/41 mmHg. The abdomen was soft, non-tender bowel sound was detected; urine and stool output was normal. Treatment was started immediately with IV fluid, a broad-spectrum antibiotic, Mannitol, and antipyretic; to prevent further convulsion he was given injection diazepam 12 hourly. A CT scan of the brain, blood routine test, urine routine test, ECG, and CSF analysis (following a lumbar puncture) was done. The hematological report showed neutrophilic leucocytosis (91.20%) and Hyponatremia (Sodium 122.00 mmol/L). All other examinations including CT and CSF study (including culture) were normal. Due to under sedation and acuteness of condition EEG was not done. At night (16th July) the patient complained of mild abdominal pain which was subsided following NSAID intake. After 24 hours of hospitalization, the patient did not have further convulsion or vomiting. But the general condition was not improved.
Among other several cases, this case was presented to the Visiting keynote speakers and experts of the “Asia-Europe Medical Summit forum 2019 and Children’s Asthma salon in Yulin (July 17th, 2019)” at Shenmu County Hospital (Shaanxi, China) in the “Case discussion and diagnosis session”. A group was formed with a Neonatologist and a pediatric Neurologist (from Russia), a Gastroenterologist (from Bangladesh) and a General Surgeon (from Nepal) along with two senior Pediatric consultants of Shenmu hospital and was proceeded for patient examination.
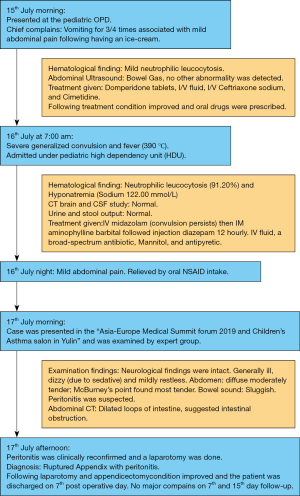
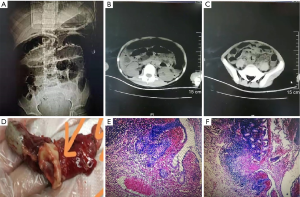
On examination, the patient was found generally ill, dizzy (due to sedative) and mildly restless. Because of sedation the patient was unable to respond and cooperate properly while examination, this created confusion regarding the degree of presenting features, especially abdominal findings. Neurological examination revealed no significant abnormality. But the abdomen was diffuse moderately tender on palpation and tympanic on percussion. Sluggish bowel sound was noted. On deep palpation, the McBurney’s point found most tender, signs of peritonitis were also noted (but not confirmed). Appendicitis was clinically suspected. An abdominal CT scan was advised urgently. The CT scan evaluated dilated loops of intestine, suggested features of intestinal obstruction (Figure 1A,B,C). The Chief Surgeon of the institute was immediately consulted and the diagnosis of Peritonitis was clinically reconfirmed. An emergency laparotomy was performed under general anesthesia. A large amount of yellow purulent fluid was visualized in the abdominal cavity. The appendix was enlarged, inflamed, gangrenous and perforated; Histopathology was done for further confirmation (Figure 1D,E,F). An appendicectomy with abdominal lavage was done; a pelvic drainage tube was retained following procedure. Following the operation, the patient’s condition was improved. There was no further attack of convulsion, even after the postoperative withdrawal of sedatives. The patient was discharged on the 7th postoperative day. On his 7th and 15th day follow-up following discharge, there were no significant complaints (Figure 2).
Discussion
A case of appendicitis typically presents with acute abdominal pain, occasional vomiting, and fever. Though there might be differences in the presenting symptoms depending on the type of appendix and severity of the condition. But almost every case has common presenting features and physical examination findings. In most cases diagnosis are confirmed by combine clinical, hematological and CT or ultrasonographic findings. Though an ultrasonogram or a CT report sometimes can be misleading, and might not conclude appendicitis or even appendiceal perforation. Almost 79% of such cases were diagnosed by physical findings and clinical judgment; besides this, children ≤6 years of age that went through a CT had a higher percentage of perforated appendix in the final diagnosis (3). Although studies have reported perforated appendicitis rates to range 30–45% among all the diagnosed cases (4). Such cases are mostly due to atypical history and unreliable examination results in very young children’s (5,6).
In our patient the history was clear and the primary physical findings were not in favor of appendicitis. The confusion was why the symptoms of peritonitis due to appendiceal perforation developed so late and suddenly. Moreover severe generalize convulsion, history of vomiting, recent abdominal ultrasound finding, the clinical and examination findings mislead the diagnosis towards neurological illness and electrolyte imbalance and endangered the patient’s life.
The multidisciplinary team (MDT) has discussed the following issues regarding this patient.
The general appearance of the patient was unwell despite 24 hours of no convulsion and the patient seemed a bit restless. The body temperature was normal, the pulse rate was 126/min. and respiration rate was 24/min. The abdomen was soft and moderately diffuse tender. The most prominent tenderness over McBurney’s point and sluggish bowel sound on auscultation were noted. On detail neurological examination, no abnormality was detected, except the dizziness. Which was due to the sedative. Besides, the CT brain and the CSF studies were also normal. The MDT team concluded that this was a case of Appendicitis and peritonitis was suspected. The lack of rigidity of the abdominal muscle and the lack of precise symptoms of appendicitis created confusion. But this was explained as an effect of the sedative therapy given and continued to control and to prevent further convulsion. All the members agreed that this was a highly uncommon and misleading case of a ruptured appendix that presented with neurological features rather than typical abdominal pain and has not been encountered or heard by them till now. This caused the mislead and delay to the accurate diagnosis also endangered the patient. So the MDT team suggested to pay high attention for an abdominal evaluation at the same time of the neurological evaluation by CT or MRI in patients of convulsion, those have even a minor history of gastrointestinal or abdominal symptoms as a presenting feature or as recent history.
This case report has limitations, namely, this is a single incidence also this occurrence and suggestion for abdominal evaluation are based on our observation in the pediatric age group.
On the basis of the described case though there was no clear notable point to differentiate peritonitis at the first impression, but we believe an abdominal evaluation (CT/MRI) should be done besides neurological evaluations as an initial investigation of patients presents with convulsion who had a recent sudden history of gastrointestinal symptoms or even mild abdominal complains. We hope this report will help to avoid further complications and unwanted situations, also to keep a differential diagnosis regarding such misleading and confusing neurological presentations of underlying disease in the case of pediatric populations.
Acknowledgments
The authors are thankful for the cooperation of the Department of Pediatrics, Shenmu County Hospital, Shaanxi, China.
Funding: Key and R & D projects of Shaanxi Province (Key project- Social Development areas: 2017ZDXM-SF-065).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Viniol A, Keunecke C, Biroga T, et al. Studies of the symptom abdominal pain—a systematic review and meta-analysis. Fam Pract 2014;31:517-29. [Crossref] [PubMed]
- Pechmann A, Wellmann S, Stoecklin B, et al. Increased von Willebrand factor parameters in children with febrile seizures. PLoS One 2019;14:e0210004. [Crossref] [PubMed]
- Luo CC, Chien WK, Huang CS, et al. Trends in diagnostic approaches for pediatric appendicitis: nationwide population-based study. BMC Pediatr 2017;17:188. [Crossref] [PubMed]
- Acheson J, Banerjee J. Management of suspected appendicitis in children. Arch Dis Child Educ Pract Ed 2010;95:9-13. [Crossref] [PubMed]
- Garcia Peña BM, Mandl KD, Kraus SJ, et al. Ultrasonography and limited computed tomography in the diagnosis and Management of Appendicitis in children. JAMA 1999;282:1041-6. [Crossref] [PubMed]
- Bonadio W, Peloquin P, Brazg J, et al. Appendicitis in preschool aged children: regression analysis of factors associated with perforation outcome. J Pediatr Surg 2015;50:1569-73. [Crossref] [PubMed]