
Non-pharmacologic management of attention-deficit/hyperactivity disorder in children and adolescents: a review
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a very common neurobehavioral disorder that affects children and adolescents. ADHD can affect the ability of a child to grow academically and socially and can persist beyond adolescence into adulthood. A primary care provider (PCP) should identify ADHD as any other chronic condition and should apply the chronic care model in management and regard a child or adolescent with ADHD as one requiring special health care needs (1).
Based on 2016–2017 National Survey of Children Health survey, about 5.3 million children in the US were diagnosed as ADHD, which represented about 8.8% of the population aged 3–17 years. Out of them, 3.9 million are currently taking medication (2). This was a rise of 23% more children diagnosed with ADHD compared with 2003 (3). In a general population, there are about 9.2% males and 2.9% females that exhibit behaviors consistent of ADHD (4). This is a huge economic burden for the US health system as more children are diagnosed with ADHD; it was estimated that the adjusted total increase in cost of ADHD for a person yearly was about $949.24 (5) and cross-sector costs associated with ADHD in the US would likely exceed 52 billion (3).
The role of the PCP includes not only diagnosis and medication management but also referral for other resources, both educational and behavioral. Traditionally medications have been the cornerstone of treating ADHD, non-pharmacological treatments are also showing some promise (6-8).
The American Academy of Pediatrics (AAP) has recently updated guidelines in 2019 which has formed the basis of management of ADHD (1):
Preschool age group (4–5 years): first line treatment is evidence based parent training in behavior management (PTBM) and/or behavioral classroom interventions, methylphenidate may be considered if no improvement;
Elementary school-aged children (6–11 years): medications approved by Food and Drug Administration (FDA) along with PTBM and/or behavioral classroom interventions (preferably both);
Adolescents (12–18 years): FDA approved medications is preferred treatment. Evidence based training interventions and/or behavioral interventions should be encouraged.
The American Psychological Association (APA) Working Group on psychoactive medications for children and adolescents recommend psychosocial therapy first followed by medications if insufficient (9). However, the Multimodal Treatment of ADHD (MTA) Cooperative Group found that starting with medication was better than behavioral treatment (10). Pelham et al. did a multi-randomization study of treatment sequencing in ADHD and concluded that starting treatment with behavioral intervention showed better results than beginning with medications, while starting with medication and later adding behavioral therapy was found to be less effective option (11).
This article focuses on the non-pharmacologic management of ADHD and will be discussed under two broad headings: Psychosocial treatments and Integrative medicine.
Psychosocial treatments
Since 1998, there has been strong body of evidence that support using psychosocial treatments for ADHD in children and adolescents (6-8). There are 3 types of psychosocial treatments that can be recommended:
- Behavior management interventions (parent training, classroom interventions, peer-based interventions);
- Training interventions (cognitive training, neurofeedback, organization), cognitive behavior therapy (CBT);
- Physiological treatments (physical activity).
Behavior management interventions
Behavioral interventions rely on changing behavioral contingencies so that children increase desired behaviors and decrease undesirable ones. Parent-child therapy helps parents/caregivers to enhance their parenting techniques and foster better relationship between caregivers and children (12). Caregivers are taught to recognize problematic behaviors in their children and discourage unwanted behaviors through nonphysical means like timeouts and reward positive behaviors through positive attention and praise (13). PTBM sessions usually last 7–12 weeks or longer and can be provided by qualified behavioral health professionals. There are different structured and standardized approaches to PTBM which are highlighted in Table 1 (14,15).
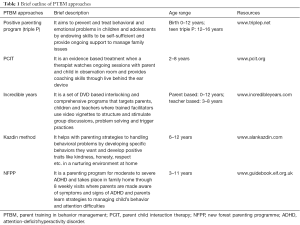
Full table
There have been few studies looking at comparative effectiveness of PTBM. Charach et al. examined about 55 studies involving PTBM and found overall strength of evidence was high for improved child behavior (14). A network meta-analysis of about 190 randomized control trails (RCT) showed stimulants were superior to behavior therapy but combination of both medication and behavior therapy together were superior to either one (16). Though studies by Fabiano et al. (17) and Evans et al. (18) found improved outcomes with behavioral therapy alone, most showed that behavioral therapy may improve behavior but not necessarily reduced overall symptoms of ADHD (19-21). A limitation is in the terminology of “parent training” as parents may perceive they may be at fault for the child symptoms (13). It is important to use family-centered language and advise caregivers on the evidence for such programs and parent satisfaction data that accompanies them (12).
Classroom or school based interventions
Some children with ADHD may qualify for receiving special education services in school. In March 1999, ADHD was added to the list of conditions under Individual with Disabilities Education Act (IDEA) that could qualify child eligible for specialized interventions under the “Other Health impairment (OHI)” category (which generally includes medical conditions such as heart ailments, asthma, diabetes or rheumatic fever) (22). A group of people use a 2-pronged test to determine eligibility under IDEA, prong one—the child must have an eligible medical diagnosis (in this case, ADHD) and prong two—the child must need special education related services on account of that disability impairing educational functioning. An individualized education program (IEP) is then planned for that student and is used to deliver the individualized instruction that is then monitored periodically (23). If the child does not qualify under IDEA, it may be possible to qualify under Section 504 of Rehabilitation Act of 1973. For this, a child’s disability (in this case, ADHD) must substantially limit a major life activity like learning, walking, breathing, caring for oneself but also includes, concentrating, thinking, and communication with others. Under Section 504 Plan, there may be specific accommodations that might be provided for the child such as reducing the number of homework problems without decreasing content, providing a quiet place to study, providing simple and clear directions for assignments, providing tests in a quiet place, divide tests into smaller tests, modifying format of a test, providing more time, and creating communication notebook between parents and teachers (24).
A study by Sayal et al. did not find improvement in 4 and 5 years old with classroom based interventions (25), while another study by Charach et al. found enhanced academic performance but improvement lasted only as long as interventions were provided (26).
Peer based interventions
These are interventions based on peer relationships and interactions and are usually done in group based setting. Quality friendship has been important for any child’s development and it has been found that more than 50% of children with ADHD face problems with interaction with their peers (27). Three types of peer-based interventions have been described (28). The first is peer involvement where peers facilitate each other’s learning through social interaction strategies like sharing, helping, instructing, praising which are sometimes facilitated through instructors. The second is peer-mediated intervention where a peer is selected and trained to provide instruction and facilitate change in the target child. It helps to improve social skill integration and since it was found to be very effective in children with autism spectrum disorders; it has been used in ADHD as well. The third is peer-proximity intervention where a peer is chosen with increased skills to sit in close proximity to the child like same table in classroom. Pelham et al. showed that office based social skills training (SST) interventions have minimal effects in improving parent ADHD ratings (29) though another study by Tutty et al. showed positive effects in parent ratings when clinic-based SST and BPT were delivered (30). A study by Cordier et al. (28) concluded that peer inclusion interventions improved relationship between peers and also help increase social competence than those who received no treatment but also found that there needs to be more studies to look at peer based interventions.
Psychotherapy interventions
These interventions generally differ from behavioral parent interventions in that they focus on the child behavior and offer training to the child/adolescent. Some examples are cognitive behavioral therapy (CBT), cognitive training and play therapy.
CBT
CBT has been described as “a form of psychological treatment that is based on the principles that psychological problems are based, in part, on faulty or unhelpful ways of thinking, and learned patterns of unhelpful behavior, and can help them learn better ways of coping with them, thereby relieving their symptoms and becoming more effective in their lives” (31). CBT is conducted over a series of structured sessions and has been effective for depression, anxiety, eating disorders and severe mental illness. Results of 2 studies that involved adolescents receiving CBT found that parents had improved ratings of ADHD symptoms but found little evidence for benefits on functional impairment (9,32,33).
Cognitive training
Cognitive training helps to improve working memory and involves computerized training that can be administered with or without clinicians (16). Cogmed Working Memory Training (CWMT) is a training program given by using computers that is designed to enhance verbal and nonverbal memory. Braingame Brian is another 25-computerized training program for 8–12 years old children that focus in working memory, cognitive flexibility and inhibition (18). Steeger et al. found adolescents 11–15 years old who received CWPT had better verbal working memory than those who did not receive CWMT (34) while another study by van Dongen-Boomsma et al. showed that there was no statistical benefit who received CWMT compared to those who received similar placebo task (35). Both studies did not show any improvement in parent, teacher and clinician rated ADHD symptoms. Dovis et al. (36) who studied Braingame Brian found improved working memory but no change in parent or teacher rating in ADHD symptoms but Van Der Oord found significantly reduced parent rating ADHD symptoms (37).
Biofeedback and neurofeedback
Biofeedback is a technique using operant conditioning principles which helps patients learn to control certain bodily functions, such as their heart rate or breathing, while connected to sensors which send real-time information about those bodily functions, often via computer (38). For children in particular, biofeedback can be a useful therapy because many children view the biofeedback activities as a sort of computer game (39).
Neurofeedback is a subset of biofeedback that utilizes EEG (more commonly) or functional magnetic resonance imaging (fMRI) with patients attempting to modulate their brain activity in real time either visually or acoustically, and is showing promise in ADHD (39). Children with ADHD often have decreased beta activity, and increased theta activity. Beta activity is found to have positive relation to attention and theta activity is found to have negative relation to alertness (40). The aim of neurofeedback with these two variables is to reverse these relationships to improve attention and alertness. The thought is held that frequent use of neurofeedback will strengthen neural networks needed to sustain focus and improve executive function (39).
A 2014 study using neurofeedback in children with ADHD found significant improvement after three months of therapy, and the improvement was found to be even greater in children who used both biofeedback and a behavior intervention (41). A 2017 RCT that looked at effects of neurofeedback on beta and theta activity (40) in children with ADHD found the greatest effects in training on beta (attention), while there were no clear effects on theta (alertness). While there was significant improvement in beta frequency band, the study did not find any improvement in ADHD symptoms over time. Overall, biofeedback and its subset of neurofeedback is still an experimental therapy that requires further investigation to establish long-term effectiveness.
Organizational skills training
This intervention focuses on building organization skills, cooperation and time management skills in children with ADHD. It helps to build organization skills with daily planner, to-do lists or breaking tasks into parts. Bul et al. designed Plan-it Commander, a digital game for children aged 8–12 years with 65 min session that was given three times a week for duration of 10 weeks along with medication for ADHD. It was found to get higher rating from teacher and parent to their children on time management skills and working memory skills (42).
Physiological interventions
Physiological interventions are regular physical activity and they are hypothesized to help a child with ADHD. Guidelines from the US Department of Health and Human services recommend preschoolers should be active the whole day physically and 6-17-year-old should have at least 1 h of physical activity every day (43). PCPs also recommend 1 h of physical activity everyday as part of ‘5-2-1-0 rule’ for staying fit and reducing excess weight (44). It is believed that not only it improves overall well-being and health; it also helps cognitive function like improved memory, attention which should help a child with ADHD (43). Hoza et al. in 2015 studied 31 min of physical activity in the form of games vs. 31 min of sedentary activity where children got involved in art projects and found that group favored sedentary intervention over physical activity though both groups demonstrated lower parent and teacher rated ADHD symptoms (45). Pontifex et al. showed aerobic exercise improved neurocognitive function (46).
Integrative medicine
National Center for Complementary and Integrative Health (NCCIH) describes integrative health care as one that “emphasizes a patient-focused holistic approach to health care and wellness—often including mental, functional, emotional, spiritual, social, and community aspects—and treating the whole person rather than, for example, one organ system” (47). The different forms of integrative medicine are (I) biologically based systems which include herbal products and dietary supplements; (II) mind body practices like art/music/pet/aromatherapy, biofeedback, hypnotherapy, meditation/mindfulness, prayer, yoga etc.; (III) manipulative and body based systems like osteopathy, chiropractic; (IV) alternative whole medical systems like Ayurveda, homeopathy, naturopathy, traditional Chinese medicine; (V) energy/biofield therapies like acupuncture, healing touch. About 50% to 64% of parents of children with ADHD report using integrative medicine to treat ADHD symptoms (5).
Mind-body interventions
Meditation
Meditation is considered a viable option for ADHD as it enhances being attentive to the present moment using focus and sustained attention (48). A 2018 systemic meta-analysis of RCTs (49) found that “meditation-based therapies” (which included mindfulness, vipassana, yoga, among many others) resulted in a moderate effect size in improving childhood ADHD symptoms, with higher benefits in inattention than in hyperactive-impulsive symptoms. Though there were improvements in the ADHD symptoms in children, there was no improvement in inhibition and working memory, while adults benefitted in these realms.
Yoga
Yoga is a subset of mindful practice that requires those practicing to build control over their mental and physical activity simultaneously. It has become increasingly popular, with a 2012 estimate of 1.7 million US children participating in a yoga program (50). While effective for anxiety disorders in both adults and children, it can be helpful in other mental health disorders (51). Yoga offers strategies to increase attention regulation and emotion regulation skills, which are core to ADHD (52). It is believed that the posture control and motor skills required for yoga may improve ADHD symptoms by activating the prefrontal cortex (53). Other reported benefits of yoga include improved cardiovascular fitness, decreased depression and stress, and increased emotional self-regulation (54). In a study (55) of adolescent girls who were either randomly assigned yoga or physical training, there was improvement in executive function in the yoga group when compared with the physical training group. This suggests that yoga helps in planning, attentive behavior and helps in controlling emotional reactions. A RCT (56) which studied 6 weeks yoga training in preschoolers found a modest improvement on attention measures and some improvements in parent ratings as well.
A systemic review (57) performed by Evans et al. found improvement in ADHD symptoms in studies that focused on child yoga and parent-child yoga. In addition, self-esteem of child was found to be improved with a medium to large effect in patent reporting compared to no improvement in child reporting. There was also found to be a modest improvement in parent-child relationships, possibly related to improved parental stress and mood in addition to effect on the child’s behavior. However, the study acknowledged that was a large possibility of bias across studies that studied yoga or similar meditation-based interventions as management for ADHD, particularly because of the difficulty in creating randomized controlled trials and due to lack of attention to this domain overall.
Tai chi
Traditional Chinese medicine for ADHD is wide encompassing, and includes therapies such as Chinese herbal medicine, acupuncture,), Yaoshan (diet therapy), Tui na (Chinese medical massage and Tai chi chuan (also known as tai chi or Taiji). A combined form of traditional Chinese medicine, which utilizes multiple therapies concurrently, has been found by a systematic review of 34 trials (58), to be equivalent to methylphenidate for use in treatment of ADHD in children for shorter duration, and had a more stable effect in long-term treatment. However, the studies included were all of low methodological quality and many had a potential bias. Tai chi has been gaining popularity in western culture and it is considered a practice of yin-yang balance by using slow movements of dynamic and static forms along with breathing techniques (59). Long-term practice of tai chi alone has been found to improve attention, reduces emotional outbursts, irritability, and anxiety in adults (59). One clinical trial (60) randomized thirty children with ADHD into a tai chi and control group and was found to have reduced hyperactivity and aggressiveness and improved learning abilities. Another trial (61) found that adolescents also had improvements in anxiety, hyperactivity, and inappropriate emotions that persisted 2 weeks after the cessation of twice weekly tai chi practice. A very small trial (62) in Portugal with four children, between ages 6 and 10, showed moderate improvements in hyperactive-impulsive symptoms with very minor improvements in inattentive symptoms. All studies were limited in size and were not blinded, but their findings were notable for improvement for some of the behavioral and regulation difficulties in children with ADHD. Some of the benefits of Tai Chi include the low-impact nature of the exercise and ability to practice nearly anywhere with no need for equipment. In addition, unlike Chinese herbal medicine, it is unlikely to negatively impact the concurrent pharmacotherapy treatment of ADHD.
Mindfulness
The practice of mindfulness has its roots in Buddhist tradition, but, like many other meditative practices, is also becoming more widely used in the western world. It is based on the principle of being nonjudgmental in accepting and being aware of each moment as it comes, which requires focus and attention (63). Neuroimaging supports this, as changes in the brain have been found in regions associated with attention immediately after practicing mindfulness (64). Mindfulness-based interventions are gaining widespread use and have also shown to help in adults with depression, stress and pain (65). However, the impact of mindfulness on attention is what would be beneficial to patients with ADHD, particularly those with the inattentive type of ADHD.A 2017 systemic review (66) attempted to look at benefits of mindfulness in both children and adults who had ADHD, and found that in adults, mindfulness-based interventions had significant improvement in attention. There were not enough studies to find a significant benefit in children as well, however considering that it has been shown that mindfulness training does impact healthy children’s school function, it is likely that these benefits would extend to children with ADHD as well.
Hypnotherapy
Clinical hypnotherapy is the utilization of therapeutic suggestions during a state of altered consciousness within a focused state to facilitate the mind-body connection, quite similarly to other self-regulatory methods discussed previously (67). There has been very limited research into hypnotherapy’s impacts on ADHD, particularly in children, although it has been found that patients with ADHD who were taking methylphenidate were found to be more susceptible (68).
Dietary interventions
One of the earliest treatments for ADHD comes from Hippocrates, who described patient with features similar to ADHD as having “quickened responses to sensory experience, but also less tenaciousness because the soul moves on quickly to the next impression”. His treatment suggested various dietary interventions and physical activities (69). Modern day dietary interventions for ADHD include restricted elimination diets (eliminating food associated with hypersensitivity), avoidance of artificial food color and supplementation of free fatty acid.
A study by Patrick has shown that Vitamin D and omega-3 fatty acids have improved cognitive function and behavior in adults with ADHD, schizophrenia, bipolar disorder, and impulsive behavior (70), though it is not fully understood why. It has been postulated that this may be because of lower vitamin D level in children with ADHD than in healthy children and insufficient levels of these substances during critical periods of neurodevelopment may be to blame (70,71). In addition, perinatal suboptimal vitamin D levels have also shown some association with a higher risk of developing ADHD later in life (72). It is not yet clear, however, at which point (or points) during development this association is strongest. There is also a possibility that the link between ADHD and low levels of vitamin D and may be due to sunlight exposure and possible circadian clock disturbances in regions with less sunlight intensity (73).
A systematic review of studies involving free fatty acid supplementation found that there was a significant reduction in ADHD symptoms (74). Another RCT which was double blind, placebo-controlled evaluated the effectiveness of supplementation of Vitamin D to methylphenidate found significant improvement in ADHD symptoms, particularly in the evening, although there isn’t yet sufficient evidence to support monotherapy with vitamin D (75).
A 2004 meta-analysis that involved placebo-controlled double-blind studies found a significant linkage between synthetic colors to ADHD symptoms by parent ratings, but the same was not found in teacher or observer ratings (76). Since that time, there have been more studies evaluating the effectiveness of synthetic color elimination on ADHD symptom improvement, although nearly all of them rely on parent ratings, or physician ratings which rely on parent reports, of children’s symptoms (77). Results of elimination diet studies have been mixed overall, and there is currently no clear relationship between artificial food coloring or particular foods and ADHD symptoms, except possibly in a minority of children who suffer from significant food intolerance or allergies (77). There is also ongoing research evaluating the impact of antioxidant supplementation on ADHD symptoms, as it is known that oxidative stress can cause neuronal damage and immune dysfunction and eventually to neurodevelopmental disorders (78).
Herbs such as Ginkgo biloba, a tree native to China, and St. John’s wort have been studied in ADHD. St Johns wort is an herb that is often used in depression as a form of alternative medicine. A 2010 RCT with 50 children with ADHD found that Ginkgo tablets were less effective than methylphenidate in treating the symptoms of ADHD (79). It is unclear if Ginkgo treatment is superior to placebo (80). A 2008 RCT (81) with 54 children with ADHD found that 8 weeks of treatment with St. John’s wort did not find improvement in symptoms of ADHD. Additionally, as a CYP 450 inducer, the treatment may have significant interactions with many other medications and can cause a variety of unpleasant side effects (82).
Conclusions
ADHD is a chronic condition that impacts functioning throughout the span of life. It requires multimodal interventions and though medications approved by FDA form the cornerstone of treatment of ADHD, many studies have shown non-pharmacological interventions also have become helpful to overall management of ADHD. Though many parents use some form of integrative medicine in ADHD, there are mixed results from studies. More research is needed in the mind-body, herbal and other integrative interventions for ADHD.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest:DRP serves as the unpaid Deputy Editor-in-Chief of TP and the unpaid Guest Editor of the focused issue “Neurodevelopmental and Neurobehavioral Disorders in Children”. TP. Vol 9, Supplement 1 (February 2020). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wolraich ML, Hagan JF Jr, Allan C, et al. Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics 2019;144:e20192528. [Crossref] [PubMed]
- Child and Adolescent Health Measurement Initiative. 2016-2017 National Survey of Children’s Health (NSCH) data query, supported by Cooperative Agreement from the U.S. Department of Health and Human Services. (cited 09/23/2019). Available online: www.childhealthdata.org
- Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry 2014;53:34-46.e2. [Crossref] [PubMed]
- Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. American Academy of Pediatrics. Pediatrics 2000;105:1158-70. [Crossref] [PubMed]
- Gupte-Singh K, Singh RR, Lawson KA. Economic Burden of Attention-Deficit/Hyperactivity Disorder among Pediatric Patients in the United States. Value Health 2017;20:602-9. [Crossref] [PubMed]
- Pliszka S. Practice Parameter for the Assessment and Treatment of Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry 2007;46:894-921. [Crossref] [PubMed]
- Evans SW, Owens JS, Wymbs BT, et al. Evidence-Based Psychosocial Treatments for Children and Adolescents With Attention Deficit/Hyperactivity Disorder. J Clin Child Adolesc Psychol 2018;47:157-98. [Crossref] [PubMed]
- Pfiffner LJ, Haack LM. Behavior management for school-aged children with ADHD. Child Adolesc Psychiatr Clin N Am 2014;23:731-46. [Crossref] [PubMed]
- APA Working Group on Psychoactive Medications for Children and Adolescents. Psychopharmacological, psychosocial, and combined interventions for childhood disorders: Evidence base, contextual factors, and future directions. Washington: American Psychological Association, 2006.
- A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry 1999;56:1073-86. [Crossref] [PubMed]
- Pelham WE, Fabiano GA, Waxmonsky JG, et al. Treatment Sequencing for Childhood ADHD: A Multiple-Randomization Study of Adaptive Medication and Behavioral Interventions. J Clin Child Adolesc Psychol 2016;45:396-415. [Crossref] [PubMed]
- Kaplan A, Adesman A. Clinical diagnosis and management of attention deficit hyperactivity disorder in preschool children. Curr Opin Pediatr 2011;23:684-92. [Crossref] [PubMed]
- Young S, Amarasinghe JM. Practitioner review: nonpharmacological treatments for ADHD: a lifespan approach. J Child Psychol Psychiatry 2010;51:116-33. [Crossref] [PubMed]
- Charach A, Carson P, Fox S, et al. Interventions for preschool children at high risk for ADHD: a comparative effectiveness review. Pediatrics 2013;131:e1584-604. [Crossref] [PubMed]
- Gleason MM, Goldson E, Yogman MW, et al. Addressing Early Childhood Emotional and Behavioral Problems. Pediatrics. 2016. Available online: https://pediatrics.aappublications.org/content/138/6/e20163025.long
- Catalá-López F, Hutton B, Núñez-Beltrán A, et al. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents:A systematic review with network meta-analyses of randomised trials. PLoS One 2017;12:e0180355. [Crossref] [PubMed]
- Fabiano GA, Pelham WJ, Coles EK, et al. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clin Psychol Rev 2009;29:129-40. [Crossref] [PubMed]
- Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol 2014;43:527-51. [Crossref] [PubMed]
- Brown RT, Amler RW, Freeman WS, et al. Treatment of attention-deficit/hyperactivity disorder: overview of the evidence. Pediatrics 2005;115:e749-57. [Crossref] [PubMed]
- Zwi M, Jones H, Thorgaard C, York A, et al. Parent training interventions for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev 2011;7:CD003018. [PubMed]
- Storebø OJ, Skoog M, Damm D, et al. Social skills training for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev 2011.CD008223. [PubMed]
- U.S. Department of Education. Children with ADD/ADHD— Topic Brief. 1999. (cited 24/09/2019). Available online: https://www2.ed.gov/policy/speced/leg/idea/brief6.html
- U.S. Department of Education, Office of Special Education and Rehabilitative Services. A Guide to Individualized Educational Program. 2000. (cited 24/09/2019). Available online: https://www2.ed.gov/parents/needs/speced/iepguide/index.html
- U.S. Department of Education, Office for Civil Rights, Free Appropriate Public Education for Students with Disabilities. (cited 24/09/2019). Available online: https://www2.ed.gov/about/offices/list/ocr/504faq.html
- Sayal K, Owen V, White K, et al. Impact of early school-based screening and intervention programs for ADHD on children's outcomes and access to services: follow-up of a school-based trial at age 10 years. Arch Pediatr Adolesc Med 2010;164:462-9. [Crossref] [PubMed]
- Charach A, Dashti B, Carson P, et al. Attention Deficit Hyperactivity Disorder: Effectiveness of Treatment in At-Risk Preschoolers; Long-Term Effectiveness in All Ages; and Variability in Prevalence, Diagnosis, and Treatment. Rockville: Agency for Healthcare Research and Quality, 2011 Oct. Report No.: 12-EHC003-EF.
- Tur-Kaspa H. Social Functioning of Children With Attention Deficit Hyperactivity Disorder. In: Gozal D, Molfese DL. editors. Attention Deficit Hyperactivity Disorder. Humana Press, 2005:317-36.
- Cordier R, Vilaysack B, Doma K, et al. Peer Inclusion in Interventions for Children with ADHD: A Systematic Review and Meta-Analysis. Biomed Res Int 2018;2018:7693479. [Crossref] [PubMed]
- Pelham WE Jr, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Psychol 1998;27:190-205. [Crossref] [PubMed]
- Tutty S, Gephart H, Wurzbacher K. Enhancing behavioral and social skill functioning in children newly diagnosed with attention-deficit hyperactivity disorder. J Dev Behav Pediatr 2003;24:51-7. [Crossref] [PubMed]
- What is Cognitive Behavioral Therapy. American Psychological Association. (cited 24/09/2019). Available online: https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- Boyer BE, Geurts HM, Prins PJ, et al. Two novel CBTs for adolescents with ADHD: The value of planning skills. Eur Child Adolesc Psychiatry 2015;24:1075-90. [Crossref] [PubMed]
- Sprich SE, Safren SA, Finkelstein D, et al. A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. J Child Psychol Psychiatry 2016;57:1218-26. [Crossref] [PubMed]
- Steeger CM, Gondoli DM, Gibson BS, et al. Combined cognitive and parent training interventions for adolescents with ADHD and their mothers: A randomized controlled trial. Child Neuropsychol 2016;22:394-419. [Crossref] [PubMed]
- van Dongen-Boomsma M, Vollebregt MA, Buitelaar JK, et al. Working memory training in young children with ADHD: A randomized placebo-controlled trial. J Child Psychol Psychiatry 2014;55:886-96. [Crossref] [PubMed]
- Dovis S, Van der Oord S, Wiers RW, et al. Improving executive functioning in children with ADHD: training multiple executive functions within the context of a computer game. a randomized double-blind placebo controlled trial. PLoS One 2015;10:e0121651. [Crossref] [PubMed]
- van der Oord S, Ponsioen AJ, Geurts HM, et al. A pilot study of the efficacy of a computerized executive functioning remediation training with game elements for children with ADHD in an outpatient setting: Outcome on parent- and teacher-rated executive functioning and ADHD behavior. J Atten Disord 2014;18:699-712. [Crossref] [PubMed]
- Gevensleben H. The usage of neurofeedback in children with ADHD: the method and its evaluation. Prax Kinderpsychol Kinderpsychiatr 2011;60:666. [Crossref] [PubMed]
- Gevensleben H. Neurofeedback in ADHD: further pieces of the puzzle. Brain Topogr 2014;27:20. [Crossref] [PubMed]
- Janssen TWP, Bink M, Weeda WD, et al. Learning curves of theta/beta neurofeedback in children with ADHD. Eur Child Adolesc Psychiatry 2017;26:573-82. [Crossref] [PubMed]
- Piek JP, Dyck M, Nieman A, et al. The relationship between motor coordination, executive functioning and attention in school aged children. Arch Clin Neuropsychol 2004;19:1063-76. [Crossref] [PubMed]
- Bul KCM, Doove LL, Franken IHA, et al. A serious game for children with Attention Deficit Hyperactivity Disorder: Who benefits the most? PLoS One 2018;13:e0193681. [Crossref] [PubMed]
- Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA 2018;320:2020-8. [Crossref] [PubMed]
- Rogers VW, Motyka E. 5-2-1-0 goes to school: a pilot project testing the feasibility of schools adopting and delivering healthy messages during the school day. Pediatrics 2009;123 Suppl 5:S272-6. [Crossref] [PubMed]
- Hoza B, Smith AL, Shoulberg EK, et al. A randomized trial examining the effects of aerobic physical activity on attention-deficit/hyperactivity disorder symptoms in young children. J Abnorm Child Psychol 2015;43:655-67. [Crossref] [PubMed]
- Pontifex MB, Saliba BJ, Raine LB, et al. Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. J Pediatr 2013;162:543-51. [Crossref] [PubMed]
- Complementary, Alternative or Integrative Health: What’s In a name? (cited 09/23/2019). 2019. Available online: https://nccih.nih.gov/health/integrative-health
- Meppelink R, de Bruin EI, Bögels SM. Meditation or Medication? Mindfulness training versus medication in the treatment of childhood ADHD: a randomized controlled trial. BMC Psychiatry 2016;16:267. [Crossref] [PubMed]
- Zhang J. Meditation-based therapies for attention-deficit/hyperactivity disorder in children, adolescents and adults: a systematic review and meta-analysis. Evid Based Ment Health 2018;21:87. [Crossref] [PubMed]
- Black LI, Clarke TC, Barnes PM, et al. Use of complementary health approaches among children aged 4-17 years in the United States: National Health Interview Survey, 2007-2012. Natl Health Stat Report 2015;10:1-19. [PubMed]
- Weaver LL, Darragh AR. Systematic Review of Yoga Interventions for Anxiety Reduction Among Children and Adolescents. Am J Occup Ther 2015;69:6906180070p1-9.
- Bögels SM, de Bruin EI, Van der Oord S. Mindfulness-based interventions in child and adolescent psychopathology. In: Graham P, Reynold S. editors. Cognitive behaviour therapy for children and families.New York: Cambridge University Press, 2013:371-84.
- Peck HL, Kehle T, Bray MA, et al. Yoga as an intervention for children with attention problems. School Psych Review. 2005;34:415-24.
- Diamond A, Lee K. Interventions shown to aid executive function development in children 4 to 12 years old. Science. 2011;333:959-64. [Crossref] [PubMed]
- Manjunath NK, Telles S. Improved performance in the Tower of London test following yoga. Indian J Physiol Pharmacol 2001;45:351-4. [PubMed]
- Cohen SC, Harvey DJ, Shields RH. Effects of Yoga on Attention, Impulsivity, and Hyperactivity in Preschool-Aged Children with Attention-Deficit Hyperactivity Disorder Symptoms. J Dev Behav Pediatr 2018;39:200-9. [Crossref] [PubMed]
- Evans S, Ling M, Hill B, et al. Systematic review of meditation-based interventions for children with ADHD. Eur Child Adolesc Psychiatry 2018;27:9-27. [Crossref] [PubMed]
- Lan Y, Zhang LL, Luo R. Attention Deficit Hyperactivity Disorder in Children: Comparative Efficacy of Traditional Chinese Medicine and Methylphenidate. J. Int Med Res 2009;37:939-48. [Crossref] [PubMed]
- Ni X, Zhang-James Y, Han X, et al. Traditional Chinese medicine in the treatment of ADHD: a review. Child Adolesc Psychiatr Clin N Am 2014;23:853-81. [Crossref] [PubMed]
- Wen HX. Study of the effect of Taijiquan on children who have a tendency to ADHD. Fuzhou: Fujian Normal University, 2009.
- Hernandez-Reif M, Field TM, Thimas E. Attention deficit hyperactivity disor-der: benefits from tai chi. J Bodyw Mov Ther 2001;5:120-3. [Crossref]
- Rodrigues JM, Mestre MI, Matos LC, et al. Effects of taijiquan and qigong practice over behavioural disorders in school-age children: A pilot study. J Bodyw Mov Ther 2019;23:11-5. [Crossref] [PubMed]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Deltacorte Press, 1990.
- Lutz A, Slagter HA, Dunne JD, et al. Attention regulation and monitoring in meditation. Trends Cogn Sci 2008;12:163-9. [Crossref] [PubMed]
- Hofmann SG, Sawyer AT, Witt AA, et al. The effect of mindfulness- based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol 2010;78:169-83. [Crossref] [PubMed]
- Lee CSC, Ma MT, Ho HY, et al. The Effectiveness of Mindfulness-Based Intervention in Attention on Individuals with ADHD: A Systematic Review. Hong Kong J Occup Ther 2017;30:33-41. [Crossref] [PubMed]
- Sawni A, Breuner CC. Clinical Hypnosis, an Effective Mind-Body Modality for Adolescents with Behavioral and Physical Complaints. Children (Basel) 2017;4:19. [Crossref] [PubMed]
- Lotan A, Bonne O, Abramowitz EG. Methylphenidate facilitates hypnotizability in adults with ADHD: a naturalistic cohort study. Int J Clin Exp Hypn 2015;63:294-308. [Crossref] [PubMed]
- Baumgaertel A. Alternative and controversial treatments for attention-deficit/hyperactivity disorder. Pediatr Clin North Am 1999;46:977. [Crossref] [PubMed]
- Patrick RP, Ames BN. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. FASEB J 2015;29:2207-22. [Crossref] [PubMed]
- Saedisomeolia A. Vitamin D's Molecular Action Mechanism in Attention-Deficit/ Hyperactivity Disorder: A Review of Evidence. CNS Neurol Disord Drug Targets 2018;17:280. [Crossref] [PubMed]
- Goksugur SB, Tufan AE, Semiz M, et al. Vitamin D status in children with attention-deficit-hyperactivity disorder. Pediatr Int 2014;56:515. [Crossref] [PubMed]
- Arns M, van der Heijden KB, Arnold LE, et al. Geographic variation in the prevalence of attentiondeficit/ hyperactivity disorder: the sunny perspective. Biol Psychiatry 2013;74:585-90. [Crossref] [PubMed]
- Sonuga-Barke EJS. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry 2013;170:275. [Crossref] [PubMed]
- Mohammadpour N. Effect of vitamin D supplementation as adjunctive therapy to methylphenidate on ADHD symptoms: A randomized, double blind, placebo-controlled trial. Nutr Neurosci 2018;21:202. [Crossref] [PubMed]
- Schab DW, Trinh NH. Do artificial food colors promote hyperactivity in children with hyperactive syndromes? A meta-analysis of double-blind placebo-controlled trials. J Dev Behav Pediatr 2004;25:423-34. [Crossref] [PubMed]
- Nigg JT. Restriction and elimination diets in ADHD treatment. Child Adolesc Psychiatr Clin N Am 2014;23:937. [Crossref] [PubMed]
- Verlaet AA, Maasakkers CM, Hermans N, et al. Rationale for Dietary Antioxidant Treatment of ADHD. Nutrients 2018;10:405. [Crossref] [PubMed]
- Salehi B, Imani R, Mohammadi MR, et al. Ginkgo biloba for attention-deficit/hyperactivity disorder in children and adolescents: a double blind, randomized controlled trial. Prog Neuropsychopharmacol Biol Psychiatry 2010;34:76-80. [Crossref] [PubMed]
- Bloch MH, Mulqueen J. Nutritional supplements for the treatment of ADHD. Child Adolesc Psychiatr Clin N Am 2014;23:883-97. [Crossref] [PubMed]
- Weber W, Vander Stoep A, McCarty RL, et al. Hypericum perforatum (St John's wort) for attention-deficit/hyperactivity disorder in children and adolescents: a randomized controlled trial. JAMA 2008;299:2633-41. [Crossref] [PubMed]
- ADHD and Complementary Health Approaches: What the Science Says. 2009. (cited 09/21/2019). Available online: https://nccih.nih.gov/health/providers/digest/adhd-science


