
Attention-deficit/hyperactivity disorder: diagnostic criteria, epidemiology, risk factors and evaluation in youth
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a complex, chronic, and heterogenous developmental disorder with typical onset in childhood and known persistence into adulthood. It is the most common neurodevelopmental disorder with significant impact on the affected individual’s personal, social, academic, and occupational functioning and development. The levels of impairment are brought about by persistent displays of inattention, disorganization, and/or hyperactivity-impulsivity. In the absence of biological markers, the revised diagnostic criteria mainly focus on behavioral problems with new emphasis on manifestations in adolescents and young adults. Understanding the multifactorial risk factors associated with ADHD is necessary. Evidence-based recommendations highlight the importance of conducting a clinical interview and utilizing other approaches in aiding in diagnosis, especially if informants are not readily available or inconsistent. This review article highlights the revised diagnostic criteria, epidemiology, risk factors, and approaches to evaluation needed in assessing youth with ADHD.
Diagnostic criteria
In 2013, the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5th edition (DSM-5) diagnostic criteria for ADHD was revised to increase reliability in diagnosis (1). The fundamental feature of persistent impairment due to or combination of inattention, hyperactivity, and impulsivity, is essential in diagnosis (1). The nomenclature for ADHD has particularly evolved from conditions such as hyperkinetic disease in the 1900s and minimal brain dysfunction (DSM-I) which was coined by the Oxford International Study Group of Child Neurology in the 1970s. With the recognition of attention as an essential feature, the condition was renamed to hyperactive reaction of childhood (DSM-II), then attention deficit disorder with or without hyperactivity (DSM-III), and currently as ADHD (DSM-III-R) (2,3).
The core symptoms for the two domains (inattentive and hyperactive/impulsive) remain the same as outlined in Table 1, with more detailed descriptions of how symptoms can present in adolescents ≥17 years old and adults included (1). While the norm has been 6 (or more) symptoms in younger adolescents and children, at least 5 symptoms in either domain must be present to make the diagnosis in older adolescents and adults. All symptoms must be present in at least two settings, and must clearly impact functioning. Accurate diagnosis allows for timely and appropriate intervention (1,4). In adolescence, the presentation can vary, and the most noticeable symptom, hyperactivity, tends to decrease during this developmental period (5,6), though symptoms of inattention, impulsivity, restlessness, and disorganization persist and become more obvious (1,5-7).

Full table
Due to inaccurate recall of ADHD symptoms at younger ages and later presenting inattentive manifestations, the criterion for age-of-onset for ADHD symptoms was increased from age 7 to 12 years. This extension allows for increased diagnosis in more youth experiencing significant impairment (8). Several longitudinal studies have demonstrated that ADHD persists in many patients throughout adolescence and adulthood (9). Previously, ADHD and autism spectrum disorder could not be diagnosed together, but the DSM-5 now allows diagnosis of both conditions. Lastly, while the DSM-IV classifies “subtypes” of ADHD (combined, inattentive, or hyperactive/impulsive), the DSM-5 instead distinguishes these as “presentations” to reflect that current predominant symptomatology can change. For example, a child given the diagnosis of ADHD, predominantly hyperactive, when older, may manifest more inattentive symptomatology (4). Whether or not late-onset ADHD exists as a separate diagnostic entity remains to be determined (10). If the youth has fewer impairing symptoms in the past 6 months, partial remission should be specified. Current severity can be described as mild, moderate, or severe relying on symptoms present that result in functional or occupational impairment (1).
Inattention and impulsivity can be difficult to distinguish from typical age-appropriate behavior (11). ADHD can affect function at home, school, social gatherings, extracurricular, and job settings. With academic impact, adolescents with ADHD are at risk of not graduating high school or college, and will have difficulty sustaining good relationships with peers (12). Youths with ADHD are vulnerable to risk-taking behaviors, such as tobacco, alcohol, and drug use, compared to their typically developing peers, with significantly higher predilection in developing substance use disorders (13). One study found that risky sexual behaviors are likely in adolescents with ADHD and comorbid conduct problems (14).
Epidemiology
Estimates of the prevalence of ADHD vary worldwide. The American Psychiatric Association estimated that 5% of children have ADHD with lower prevalence in adults (1). A 2015 meta-analysis of 179 prevalence estimates determined an overall pooled estimate of 7.2% (15). From a nationally representative data of children and adolescents in the United States, there is apparent increase of ADHD diagnosis in two decades from 6.1% in 1997–1998 to 10.2% in 2015–2016 (16). Recent estimates by the Centers for Disease Control and Prevention (CDC) found 6.1 million American children (9.4%) between the ages of 2–17 years had ever been diagnosed with ADHD, with approximately half belonging to ages 12–17 years (17). Rates have also been found to vary greatly by geographic region: Midwest (12.2%), South (11.1%), Northeast (10.3%), and West (7%) (16), and by state: Arkansas is estimated at 17.0%, while in Nevada, is it 5.6% (17).
There are some gender differences to consider when diagnosing ADHD with more males being diagnosed than females (ratio 2:1) (16). Males are more likely to manifest with hyperactive/impulsive symptoms, while females are more likely to have inattentive symptoms (18). With the extended age-of-onset criterion, prevalence of females with ADHD can potentially increase (8). Recent evidence suggests that notably increased emotional or behavioral problems must be seen in girls with ADHD before they meet criteria for the disorder (19). Additionally, parental perceptions of ADHD symptoms can differ based on the patient’s gender (19).
Racial/ethnic disparities exist in children and adolescents diagnosed with ADHD. The prevalence observed in the 20-year period identified 12.8% of non-Hispanic black, 12% of non-Hispanic white, and 6.1% of Hispanic youth diagnosed with ADHD (16). These rates are similar to recent reports from the CDC (17). When controlling for socio-demographics, ADHD symptoms, and comorbidities, African-American and Latino children were less likely to be diagnosed with ADHD and be medicated (20). Future screening materials and diagnostic criteria may need to account for these gender and racial/ethnic differences.
Variability of ADHD prevalence estimates could be due to methodological differences (21). A 2014 meta-regression analysis found no evidence to support the increasing number of children diagnosed with ADHD when standardized diagnostic procedures are followed (21). Cross cultural differences can also help explain the variability in prevalence. There is a tendency for parents to over-report symptoms in some countries (22,23). Providers should consider differences in cultural beliefs and expectations of behavior when collecting parental symptom reports. Most epidemiological studies to date focus on younger children with ADHD, with a lack of emphasis on studies in adolescents and adults (22,23). Further studies in these populations can help determine how often ADHD persists into adolescence and adulthood.
Risk factors
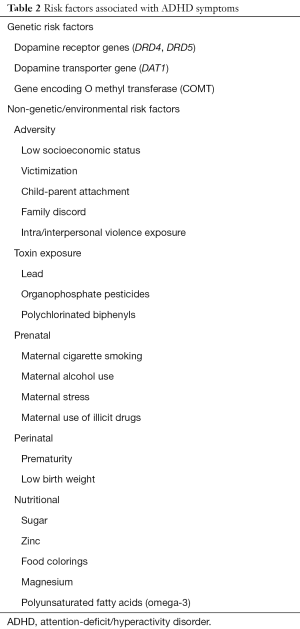
With the heterogeneity of ADHD, multiple risk factors have been identified as shown in Table 2. There is known increased genetic predisposition in the affected individual as observed in multiple family and twin studies. Candidate gene association studies had found dopamine D4 receptor gene (DRD4) and DRD5 variants with consistent associations with ADHD in several meta-analysis studies (24). There are several genome wide association studies in the early phases of discovery. One recent meta-analysis reported on 12 independent genome-wide significant loci and found that FOXP2 in chromosome 7 correlates with ADHD (25). While these loci do not yet have any identified diagnostic or clinical utility results, future studies in the neurobiology of ADHD may help elucidate the etiology of ADHD. From the same meta-analysis, genetic associations with other psychiatric conditions, such as major depressive disorder and risky behaviors like smoking have been observed, though these cannot be generalized to all settings (25).
Full table
Identifying true causality of environmental risk factors for ADHD is difficult, as associations may be observed with several affecting variables. One of the known risk factors is related to maternal health during pregnancy, including maternal use of substances such as cigarettes and alcohol. Though evidence is inconclusive due to uncertain nature and level of exposure in-utero and the outcomes of having an offspring with ADHD. Exposure to toxins such as heavy metals (i.e., lead, mercury) and chemicals (i.e., organophosphate pesticides) has been implicated as well with growing evidence of strong linkage with ADHD. The role of nutrition in ADHD etiology has been widely studied with increased supportive literature of low zinc levels and omega-3 fatty acid levels found in ADHD individuals (24,26).
There is a positive association between media use and ADHD-related behaviors (26,27). Screen-based media consumption can adversely affect sleep-wake cycles and sleep duration (28). Internet addiction, increased media usage, poor sleep-wake cycles, and internet gaming have all been associated with ADHD among adolescents (29-31). Further research is required to determine whether the relationship between use of digital media and subsequent ADHD symptoms is causal (32).
Evaluation
Evaluating a child or adolescent with ADHD requires awareness of evidence-based practices, time availability, and access to materials to conduct the evaluation. The goal is to obtain necessary information about the medical and neurodevelopmental heath in relation to the individual’s education and psychosocial status and impairment.
In 2007, the American Academy of Child and Adolescent Psychiatry (AACAP) released its official action on practice parameters for assessment and treatment of youth with ADHD consistent with DSM-IV-TR terminologies. The AACAP recommends mandatory screening for ADHD during mental health evaluations and highlights the significance of clinical interviews with recommendations of assessing for comorbid psychiatric disorders (33). In 2010, the European Network Adult ADHD published its consensus statement on diagnosis and treatment ADHD in adults with recognition of its negative impact on the adult’s quality of life (34).
The recently updated clinical practice guidelines by the American Academy of Pediatrics (AAP) provides evidence-based recommendations in the diagnosis, evaluation, and treatment of ADHD in children and adolescents (35). The key action statements emphasize the role of the clinician in initiating evaluation for ADHD in any child age 4 and up with concurrent functional impairments secondary to existing core symptoms, using the diagnostic criteria while assessing potential physical, emotional, or behavioral comorbidities. It also emphasizes recognizing affected youth as those having special health care needs, and following treatment recommendations from initiation to titration and maintenance of appropriate medications and recommending psychosocial treatments (35). Revisions of existing guidelines by the AACAP are underway and the Society for Developmental and Behavioral Pediatrics will be releasing its own recommendations on “complex ADHD” soon.
The evaluative process generally begins with the parent or caregiver seeking evaluation for concerns related, but not limited, to poor academic performance or disruptive behaviors. These concerns either originate in the home, or are relayed to the caregivers by other personnel overseeing the child in educational or daycare environments. The clinician is expected to assess the presenting concerns and usually proceeds with gathering more information and using validated scales. One may opt to referral to the specialist. While there are no published studies comparing approaches in different clinical settings in diagnosing ADHD, one study looked at developmental-behavioral pediatricians in academic settings and found that the specialists used rating scales in addition to at least 1 developmental or academic skills evaluation, and made at least 1 diagnosis of a comorbid condition (36).
Clinical evaluation
Evaluation usually starts with a comprehensive clinical interview asking about the youth’s medical, developmental/behavioral, family, and social histories. Important aspects of the medical history must include infectious or drug exposures in-utero, any pregnancy and delivery complications, medication usage, chronic medical conditions, and previous assessment of hearing and vision abilities. The clinician should document developmental skills and challenges of the youth (particularly language, motor, and academic) and inquire into educational routine disruptions or significant absences. Due to the strong genetic predisposition of ADHD, family members with ADHD and other neurobehavioral disorders must be determined. Family-related impairments during ADHD assessments may be due to other factors such as developmental maladjustment (37). Social history should reflect concerns with school, work, and relationships with peers. Query on traumatic and adverse life events and disruptions to routine such as home or school moves and impactful loss or death of loved ones or pets must be done. Confidential interview with the adolescent may reveal risky health and sexual behaviors. Asking about sleeping and eating habits is important especially if one is considering medication treatments for ADHD.
One of the challenges in diagnosing ADHD in adolescents is that while they may exhibit significant impairment, they may not meet diagnostic criteria. Also, retrospective self-report by adolescents is comparable to parents’ recall of childhood symptoms (6). While adolescents have been found to be reliable self-reporters, they can have the tendency to underreport symptoms (38). Parents may also underreport symptoms as they tend to spend less time with adolescents than younger children (7). Observation of parent-adolescent interactions can also provide supporting information in evaluating ADHD.
Aside from parents, reporting of behaviors in the form of rating scales must be obtained from various sources including teachers, after school program staff, coaches, and employers for working adolescents. Review of prior report cards can also be helpful in establishing age of onset and mapping a trajectory of symptoms (39). A narrative summary produced by the school attended by the youth typically includes behavioral observations and functional impairments at baseline. Subsequent narrative reports are useful in understanding interventions and accommodations in place as part of assessing treatment progress. Psychological testing is often not required during the routine ADHD evaluation, but may be necessary in sorting out comorbid conditions such as learning or other emotional disorders.
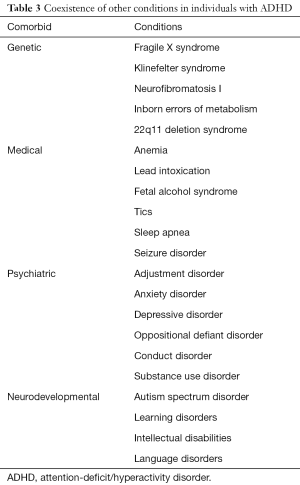
It is especially important to determine whether symptoms and problems are due to other potential causes. It is essential to screen for other disorders and factors that may contribute to ADHD-like symptoms, including poor sleep, depression, anxiety, learning disorders, and substance use disorder. Table 3 enumerates the different comorbidities that need to be identified in youth being evaluated for ADHD (1,40). Persistence of symptoms in adolescence and adulthood is significantly associated with a more severe presentation and comorbid mood, conduct, and substance use disorders (41,42). Screening for substance use is especially important in this population as persistent and adult forms of ADHD are often comorbid with substance use (41). Evaluation entails more than one office visit making it necessary for continued screening of risky and unsafe behaviors in all youth with ADHD.
Full table
Anthropometric measurements, such as weight, height, and body mass index, and vital signs, must be documented at every visit to monitor growth and pubertal development. Using age appropriate guide for blood pressure and pulse rate measurements is mandatory especially when the youth will be starting medications, particularly stimulants. The physical examination must always include a complete neurologic assessment. Close attention to any neuro-cutaneous and dysmorphic features is necessary, as certain genetic syndromes, like fragile X syndrome, neurofibromatosis, tuberous sclerosis, and 22q11 deletion syndrome, have high likelihood of presenting with ADHD-like manifestations (43).
Assessment scales/checklists
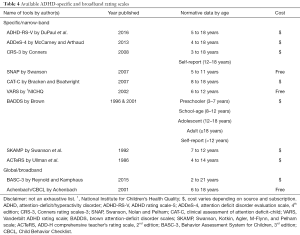
ADHD assessment scales/checklists are useful in providing more information about the youth’s problematic behaviors in confirming the diagnosis of ADHD. These are the most commonly used tools for assessment in different settings due to its ease. The 2019 AAP guidelines recommend that clinicians utilize validated rating scales to assist in the initial diagnosis, assessment for comorbid conditions, and monitoring of treatment progress (35). When choosing which rating scale to utilize, it is necessary to be aware of its limitations and variance in their normative data despite established validity, and results should be supplemental and must be interpreted in the context of integrating all the information about the individual being assessed. Table 4 shows the different specific/narrow-band and global/broadband rating scales that are available (40,44).
Full table
ADHD-specific scales are also referred to as narrow-band scales because of its focus mainly on the ADHD core symptoms. Their validity is dependent on the child’s age, what rating scale is being used, and the information provided by the source, either parent or teacher. The adolescent can be the informant as well (40,44). One of the widely used tools is the Conners rating scales (CRS), found to be reliable and valid in rating ADHD symptoms and in identifying comorbid conditions like oppositional defiant disorder (23). On the other hand, ADHD-global scales also referred to as broadband scales, uses a wider assessment including possible internalizing and externalizing behaviors. However, compared to the narrow-band scales, these have lower sensitivity and specificity in establishing the diagnosis, hence not a strong recommendation by the AAP (45). Although some studies had concluded that broadband scales, like the Child Behavior Checklist (CBCL) which covers the variable facets of childhood ADHD psychopathology, can be used for accurate diagnosis of ADHD. In a systematic review and meta-analysis looking at diagnostic accuracy of rating scales, the broadband CBCL-attention problem (CBCL-AP) and narrow-band CRS-revised (CRS-R) were both found to be comparable in their sensitivity and sensitivity in aiding diagnosis (46).
Continuous performance tests (CPTs)
Despite perceived limited sensitivity, specificity and validity, CPTs have been found to be strong and consistent tests with reliable results when determining the presence or absence of ADHD in the youth after inconclusive rating scales (47). There are several CPTs available with continued research in this field.
The test of variables of attention (TOVA®) is a lengthy computerized test that records one’s responses to visual or auditory stimuli and calculates results in comparison to matched non-ADHD and ADHD samples. In conjunction with the clinical interview and testing scales, it provides a comprehensive understanding of significant functioning impairment. TOVA can be used in all age groups (48). A similar test software is the integrated visual and auditory attention (IVA) with reported sensitivity of 92% of identifying children ages 7 to 12 years having ADHD (49). The Qbtest is a novel, commercially available computerized assessment combining CPT and high-resolution motion-tracking system. It provides an objective measurement of the core symptoms, but must be used in conjunction with the rest of the clinical evaluation (50).
Hall et al. conducted a systematic review on the clinical utility of commercially available CPTs and found that TOVA had the most evidence-based use clinically over IVA and Qbtest. They have noted that having objective activity measures and CPTs may be of value. More needs to be studied in CPTs role in pharmacologic treatment (51).
Electroencephalography (EEG)
Since ADHD is a known neurodevelopmental disorder, analyzing the brain’s electrical activity was thought to be promising. Almost 80 years ago, children found to be hyperactive, impulsive, and highly variable were found to have particular EEG findings in the fronto-central sensors (52). In a systematic review on the utility of quantitative EEG, studies have described higher theta/beta ratio in ADHD patients compared to healthy controls (53). However, this is not routinely recommended in ADHD diagnosis, although the US Food and Drug Administration did approve a medical device, called Neba®, that uses EEG testing in “diagnosing children and adolescents ages 6 to 17 years (54). One review looked at the role of EEG as a diagnostic tool for ADHD which was determined to be questionable, yet recognizing the potential utility with continued technological advancements (55).
Neuroimaging
Magnetic resonance imaging (MRI) has been used in determinations of brain finding in ADHD. Initially reductions in the basal ganglia volume and changes in shape have been described, while later studies have also noted changes in the cerebellum and frontal lobe regions (2). One recent study found widespread differences in terms of lower surface area and thickening in the frontal cortical areas of children with ADHD, but not of affected adolescents and adults (56). On functional MRI, one review study noted that affected children and adolescents show hypoactivation in frontal regions, with certain areas hyperactivated thought be a compensatory mechanism as a result of the abnormal fronto-striatal systems. There is also evidence showing parietal and temporal regional dysfunction in ADHD (57). Majority of these findings have been described from male population, with very limited longitudinal studies looking into the neurobiology of females. However, there are inconsistencies with neuroimaging and results should be interpreted in the context of the affected individual (57).
Summary
ADHD continues to be a highly prevalent neurodevelopmental disorder with multiple identified risk factors. The significant impairment in different aspects of the affected individual’s life is pronounced and well established. There is no single test that is definitive and evaluation entails a multi-step process that can be time consuming. The clinical interview is the most important step of the evaluation, yet can be challenging with unreliable and unavailable informants. Different evaluative methods, such as CPTs and neuroimaging, may be valuable in validating the diagnosis of ADHD. With the revised diagnostic criteria, there is potential increase in identifying adolescents and adults with hopes in receiving prompt treatment to allow better quality of life.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- American Psychiatric Association. Neurodevelopmental disorders: Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Washington: American Psychiatric Association, 2013. Available online: https://doi.org/ [Crossref]
- Mahone EM, Denckla MB. Attention-deficit/hyperactivity disorder: a historical neuropsychological perspective. J Int Neuropsychol Soc 2017;23:916-29. [Crossref] [PubMed]
- Lange KW, Reichl S, Lange KM, et al. The history of attention deficit hyperactivity disorder. Atten Defic Hyperact Disord 2010;2:241-55. [Crossref] [PubMed]
- Epstein JN, Loren RE. Changes in the definition of ADHD in DSM-5: subtle but important. Neuropsychiatry (London) 2013;3:455-8. [Crossref] [PubMed]
- Holbrook JR, Cuffe SP, Cai B, et al. Persistence of parent-reported ADHD symptoms from childhood through adolescence in a community sample. J Atten Disord 2016;20:11-20. [Crossref] [PubMed]
- Sibley MH, Pelham WE, Molina BSG, et al. Diagnosing ADHD in adolescence. J Consult Clin Psychol 2012;80:139-50. [Crossref] [PubMed]
- Wolraich ML. Attention-deficit/hyperactivity disorder among adolescents: a review of the diagnosis, treatment, and clinical implications. Pediatrics 2005;115:1734-46. [Crossref] [PubMed]
- Vande Voort JL, He JP, Jameson ND, et al. Impact of the DSM-5 attention-deficit/hyperactivity disorder age-of-onset criterion in the US adolescent population. J Am Acad Child Adolesc Psychiatry 2014;53:736-44. [Crossref] [PubMed]
- Agnew-Blais JC, Polanczyk G, Danese A, et al. Persistence, remission and emergence of ADHD in young adulthood: results from a longitudinal, prospective population-based cohort. JAMA Psychiatry 2016;73:713-20. [Crossref] [PubMed]
- Agnew-Blais J, Arseneault L. Late-onset ADHD: case closed or open question? Am J Psychiatry 2018;175:481-2. [Crossref] [PubMed]
- Brahmbhatt K, Hilty DM, Hah M, et al. Diagnosis and treatment of attention deficit hyperactivity disorder during adolescence in the primary care setting: a concise review. J Adolesc Health 2016;59:135-43. [Crossref] [PubMed]
- Feldman HM, Reiff MI. Clinical practice. Attention deficit-hyperactivity disorder in children and adolescents. N Engl J Med 2014;370:838-46. [Crossref] [PubMed]
- Franke B, Michelini G, Asherson P, et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol 2018;28:1059-88. [Crossref] [PubMed]
- Sarver DE, McCart MR, Sheidow AJ, et al. ADHD and risky sexual behavior in adolescents: conduct problems and substance use as mediators of risk. J Child Psychol Psychiatry 2014;55:1345-53. [Crossref] [PubMed]
- Thomas R, Sanders S, Doust J, et al. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 2015;135:e994-1001. [Crossref] [PubMed]
- Xu G, Strathearn L, Liu B, et al. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA Netw Open 2018;1:e181471. [Crossref] [PubMed]
- Data and statistics about ADHD. Centers for Disease and Control Prevention, 2019. Available online: https://www.cdc.gov/ncbddd/adhd/data.html
- Barkley RA. Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment. 4th ed. New York: Guilford Publications, 2014.
- Mowlem F, Agnew-Blais J, Taylor E, et al. Do different factors influence whether girls versus boys meet ADHD diagnostic criteria? Sex differences among children with high ADHD symptoms. Psychiatry Res 2019;272:765-73. [Crossref] [PubMed]
- Coker TR, Elliott MN, Toomey SL, et al. Racial and ethnic disparities in ADHD diagnosis and treatment. Pediatrics 2016. [Crossref] [PubMed]
- Polanczyk GV, Willcutt EG, Salum GA, et al. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol 2014;43:434-42. [Crossref] [PubMed]
- MacDonald B, Pennington BF, Willcutt EG, et al. Cross-country differences in parental reporting of symptoms of ADHD. J Cross Cult Psychol 2019;50:806-24. [Crossref] [PubMed]
- Thorell LB, Chistiansen H, Hammar M, et al. Standardization and cross-cultural comparisons of the Swedish Conners 3® rating scales. Nord J Psychiatry 2018;72:613-20. [Crossref] [PubMed]
- Thapar A, Cooper M, Jefferies R, et al. What causes attention deficit hyperactivity disorder? Arch Dis Child 2012;97:260-5. [Crossref] [PubMed]
- Demontis D, Walters RK, Martin J, et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet 2019;51:63-75. [Crossref] [PubMed]
- Froehlich TE, Anixt JS, Loe IM, et al. Update on environmental risk factors for attention-deficit/hyperactivity disorder. Curr Psychiatry Rep 2011;13:333-44. [Crossref] [PubMed]
- Nikkelen SW, Valkenburg PM, Huizinga M, et al. Media use and ADHD-related behaviors in children and adolescents: a meta-analysis. Dev Psychol 2014;50:2228-41. [Crossref] [PubMed]
- LeBourgeois MK, Hale L, Chang AM, et al. Digital media and sleep in childhood and adolescence. Pediatrics 2017;140:S92-6. [Crossref] [PubMed]
- Wang BQ, Yao NQ, Zhou X, et al. The association between attention deficit/hyperactivity disorder and internet addiction: a systematic review and meta-analysis. BMC Psychiatry 2017;17:260. [Crossref] [PubMed]
- Stavropoulos V, Adams BLM, Beard CL, et al. Associations between attention deficit hyperactivity and internet gaming disorder symptoms: is there consistency across types of symptoms, gender and countries? Addict Behav Rep 2019;9:100158. [Crossref] [PubMed]
- Thoma VK, Schulz-Zhecheva Y, Oser C, et al. Media use, sleep quality, and ADHD symptoms in a community sample and a sample of ADHD patients aged 8 to 18 years. J Atten Disord 2020;24:576-89. [Crossref] [PubMed]
- Ra CK, Cho J, Stone MD, et al. Association of digital media use with subsequent symptoms of attention-deficit/hyperactivity disorder among adolescents. JAMA 2018;320:255. [Crossref] [PubMed]
- Pliszka S. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2007;46:894-921. [Crossref] [PubMed]
- Kooij SJJ, Bejerot S, Blackwell A, et al. European consensus statement on diagnosis and treatment of adult ADHD: the European Network Adult ADHD. BMC Psychiatry 2010;10:67. [Crossref] [PubMed]
- Wolraich ML, Hagan JF Jr, Allan C, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 2019. [Crossref] [PubMed]
- Feldman HM, Blum NJ, Gahman AE, et al. Diagnosis of attention-deficit/hyperactivity disorder by developmental pediatricians in academic centers: a DBPNet study. Acad Pediatr 2015;15:282-8. [Crossref] [PubMed]
- Vazquez AL, Sibley M, Campez M. Measuring impairment when diagnosing adolescent ADHD: differentiating problems due to ADHD versus other sources. Psychiatry Res 2018;264:407-11. [Crossref] [PubMed]
- Smith BH, Pelham WE, Gnagy E, et al. The reliability, validity, and unique contributions of self-report by adolescents receiving treatment for attention-deficit/hyperactivity disorder. J Consult Clin Psychol 2000;68:489-99. [Crossref] [PubMed]
- Lijster JM, Dierckx B, Utens EM, et al. The age of onset of anxiety disorders. Can J Psychiatry 2017;62:237-46. [Crossref] [PubMed]
- Floet AM, Scheiner C, Grossman L. Attention-deficit/hyperactivity disorder. Pediatr Rev 2010:56-69. [PubMed]
- Moffitt TE, Houts R, Asherson P, et al. Is adult ADHD a childhood-onset neurodevelopmental disorder? Evidence from a four-decade longitudinal cohort study. Am J Psychiatry 2015;172:967-77. [Crossref] [PubMed]
- Caye A, Spadini AV, Karam RG, et al. Predictors of persistence of ADHD into adulthood: a systematic review of the literature and meta-analysis. Eur Child Adolesc Psychiatry 2016;25:1151-9. [Crossref] [PubMed]
- Lo-Castro A, D’Agati E, Curatolo P. ADHD and genetic syndromes. Brain Dev 2011;33:456-61. [Crossref] [PubMed]
- Collett BR, Ohan JL, Myers KM. Ten-year review of rating scales. V: scales assessing attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2003;42:1015-37. [Crossref] [PubMed]
- Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. American Academy of Pediatrics. Pediatrics 2000;105:1158-70. [Crossref] [PubMed]
- Chang LY, Wang MY, Tsai PS. Diagnostic accuracy of rating scales for attention-deficit/hyperactivity disorder: a meta-analysis. Pediatrics 2016;137:e20152749. [Crossref] [PubMed]
- Tallberg P, Råstam M, Wenhov L, et al. Incremental clinical utility of continuous performance tests in childhood ADHD - an evidence-based assessment approach. Scand J Psychol 2019;60:26-35. [Crossref] [PubMed]
- Greenberg, LM. The test of variables of attention (version 8.0). Los Alamitos: The TOVA Company, 2011.
- Integrated visual and auditory CPT (IVA-2). Available online: https://www.braintrain.com/iva2/
- . Available online: https://www.qbtech.com/QbTech.
- Hall CL, Valentine AZ, Groom MJ, et al. The clinical utility of the continuous performance test and objective measures of activity for diagnosing and monitoring ADHD in children: a systematic review. Eur Child Adolesc Psychiatry 2016;25:677-99. [Crossref] [PubMed]
- Jasper HH, Solomon P, Bradley C. Electroencephalographic analyses of behavior problem children. Am J Psychiatry 1938;95:641-58. [Crossref]
- McVoy M, Lytle S, Fulchiero E, et al. A systematic review of quantitative EEG as a possible biomarker in child psychiatric disorders. Psychiatry Res 2019;279:331-44. [Crossref] [PubMed]
- NEBA health. 2019. Available online: https://nebahealth.com/
- Lenartowicz A, Loo SK. Use of EEG to diagnose ADHD. Curr Psychiatry Rep 2014;16:498. [Crossref] [PubMed]
- Hoogman M, Muetzel R, Guimaraes J, et al. Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. Am J Psychiatry 2019;176:531-42. [Crossref] [PubMed]
- Weyandt L, Swentosky A, Gudmundsdottir BG. Neuroimaging and ADHD: fMRI, PET, DTI findings, and methodological limitations. Dev Neuropsychol 2013;38:211-25. [Crossref] [PubMed]


