Distress and adjustment among adolescents and young adults with cancer: an empirical and conceptual review
The adolescent and young adult (AYA) years are a time of complex developmental change. During this period, young people strive towards gaining autonomy and independence, whilst forming important adult social, emotional, and adaptive coping skills (1,2). A diagnosis of cancer at this stage can challenge and interrupt these aspects of development. Young people’s underdeveloped coping skills can also interfere with their capacity to successfully navigate the demands of the cancer experience. Combined, these factors may contribute to young people’s suboptimal treatment-related outcomes, as well as the documented challenges of long-term cancer survivorship (3,4). Given the many years of life that lie ahead for young people following successful cancer treatment, the manner in which AYAs adjust to the experience, and the subsequent quality of their survival, is important to understand.
In order to improve the psychological outcomes of this group, research must move beyond merely documenting the prevalence and nature of poor outcomes, to identifying factors that may underpin the emergence of these psychological outcomes (5). This review aimed to address several significant gaps in the current literature on the psychological outcomes in AYAs with cancer. In particular, the following research questions were posed:
Research question 1: what is the nature and prevalence of distress (and other psychological outcomes) among AYAs living with cancer?
The wide range of reported distress seen in AYAs with cancer has been frequently noted in the literature (6,7), although to date there has been no comprehensive review of psychological outcomes in this group. Empirical and clinical definitions of “AYA” also vary widely, ranging from 10-44 years across reports depending upon whether they are based on age, or developmental stage (8). For the purposes of this review, the broadest age range of AYAs living with cancer was used (i.e., AYAs could be current patients, recent, or long-term survivors of cancer) in order to capture data across the cancer trajectory within this developmental stage. Studies were included if participants were either (I) diagnosed with cancer during the AYA years; or (II) an AYA survivor of a pediatric cancer. All forms of psychological outcomes were examined in this review. Across studies, sample sizes have ranged from N=16 (9) to 9,126 (10), and in order to include all relevant studies, have included samples of young people from eight years old (11,12) and long-term survivors of cancer as old as 54 (13), from 4-8 weeks post-diagnosis (14) up to 41 years post-diagnosis (15). Table 1 presents the data extracted on prevalence of psychological outcomes, and echoes the wide range of findings.
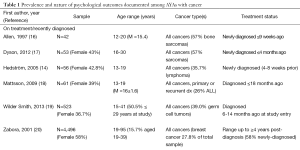
Full table
Clinical distress
Across the studies examined, ‘clinical’ levels of distress was variously defined as meeting criteria for the diagnosis of a mental disorder (e.g., post-traumatic stress disorder; PTSD) to scoring highly enough or beyond a clinical ‘cut-off’ score on a particular measure (e.g., anxiety or depression symptoms). Rates of clinical distress ranged from 5.4% (50) to 56.5% (27). A large proportion of studies reviewed (23/54) focused on post-traumatic stress symptoms (PTSS) to capture the occurrence of post-cancer distress. Of these studies, the prevalence of clinically elevated PTSS ranged from 4.8% partial PTSS combined with associated functional impairment or distress (47) to 78% with partial PTSS (30), and for diagnoses of PTSD to range from 0% (for PTSD specific to a cancer trauma) (31) to 29% PTSS indicative of possible PTSD among AYAs within 16 months of diagnosis (56). Several studies reported clinical PTSD in approximately one-fifth of their sample, however (23,25,37,42,56).
Estimated rates of clinical depression range from 5% moderate-severe depression symptoms (62) to 24% mild/major depression diagnoses (59). Reported rates of clinical anxiety range from 12% (14) to 23% among recently diagnosed AYAs (17). A growing number of studies (32,33,43,49,51,52,55,57) used the Brief Symptom Inventory-Short Form to measure distress (BSI-18) (63) which provides a composite distress score of depression, anxiety and somatic distress, and has a good factor structure in AYA survivors of childhood cancer (43). These studies found clinical distress ranged from 11% (51), to 22.2% (52) among long-term AYA cancer survivors, and up to 28% in AYAs within four months of diagnosis (57).
Trajectory of distress
Only a few studies compared AYAs’ psychological outcomes across different stages of treatment, or examined the trajectories of their distress over time (see Table 1). One group has reported heightened distress at diagnosis that reduced over the subsequent 18-month period to the point where AYAs showed better wellbeing than healthy controls (54,58) and was sustained at a 48-month post-diagnosis follow-up (58). However, in other studies, high rates of distress did not substantively decrease between a 6- and 12-month follow-up among newly diagnosed AYAs (56,57) or from pre- to post-chemotherapy administration (61). Additionally, studies examining distress across survivors differing lengths from treatment has found no differences in a range of distress levels according to time since diagnosis (9,53) or between on- versus off-treatment groups (60). Additionally, one study of long-term AYA survivors of childhood cancer found the highest rates of clinical distress among survivors diagnosed more than 20 years previously (55).
Distress in comparison to the norm, and to siblings
Adequately conceptualizing the impact of cancer on AYAs’ psychological outcomes also necessitates a comprehensive understanding of how these outcomes differ to what we might otherwise expect to see among AYAs without cancer. Several of the studies in this review compared AYAs’ outcomes either to sibling controls (13,29,32,46,50,51), general population/community norms or healthy matched peers (4,9,11,13,15,19,25,26,34,35,38,41,43,45,48,49,55,57,60,62,64-67), older cancer patients (24,43,68), comparison medical or mental health patient groups (9) or some combination of these (13,43). The majority of these studies report that AYAs demonstrated significantly higher rates and/or levels of distress relative to their comparison group (4,15,19,25,26,32,34,41,45,46,49-51,55,57,60,69).
Some studies documented levels of distress that were either not significantly different to, or were in fact lower than, their comparison group however (9,11,29,35,38,39,43,48,62,64-66). One study found that although long-term AYA survivors had significantly higher distress than their comparison siblings, both groups were less distressed relative to population norms (13). The studies finding similar or better adjustment among AYAs with cancer appeared to range widely in regards to their sample sizes, cancer types, age ranges, length of time since diagnosis, and outcome measures.
Positive outcomes
Despite growing interest in concepts of positive outcomes such as post-traumatic growth (PTG) and benefit-finding (70-72), as seen in Table 1, few studies documented the prevalence of these outcomes alongside distress. These studies found that most AYAs experience some degree of PTG (22), AYAs are more likely to report a positive than negative or no change in PTG (21), and that the level of PTG among long-term survivors significantly exceeds healthy controls (34). The emergence of adaptive outcomes alongside clinical-level distress echoes qualitative explorations of AYAs’ cancer experiences (73-75). However, to date there has been little consensus regarding factors that underpin the level of distress or positive adaptation experienced by AYAs.
In the next stage of this review, the literature was examined for factors that had been linked with psychological outcomes among AYAs. Evidence related to individual factors, cancer- or treatment-related factors, and socio-demographic factors was examined in turn, and a summary of each follows.
Research question 2: what individual, cancer/treatment-related and socio-demographic factors have been identified as predictors of these outcomes?
Individual factors
Age
The impact of age at diagnosis on later psychological outcomes has been repeatedly examined. To date, the results have been mixed. One study highlighted that younger age at diagnosis predicted suicidal ideation in long-term survivorship, possibly due to later functional impairment (10). Several studies have found that age at diagnosis did not predict PTSS/PTSD (11,30,49), depression symptoms (50), general psychological distress (49-52) or QoL (68) in longer-term survivorship. The pattern of significant results supports the notion that a cancer diagnosis during the adolescent/emerging adult years is critical, however. That is, pediatric studies have tended to find that an older age at diagnosis (i.e., into adolescence) is predictive of adaptation, including both PTG and PTSS (22), and PTSD diagnoses (25), greater psychological distress, fewer positive health beliefs and a lower sense of cognitive competence (38), greater depression symptoms (52,60), anxiety (60), and worse QoL both on- and off-treatment (18,67) and into survivorship (76). By contrast, reports from the adult oncology sector have been mixed. Some have found that relative to older adults, younger adults experience greater distress, including higher fear of cancer recurrence (24), anxiety, depression, and somatization symptoms (20), while another demonstrated lower rates of distress among AYA long-term cancer survivors than in adult oncology (43).
The data on the impact of AYAs’ current age on psychological outcomes has shown that an older AYA age at follow-up is associated with poorer physical and mental adaptation (29), greater levels of PTSD (46) and cancer- and future-related worries (66) in longer-term survivorship. However, in many cases, an AYAs’ current age has not been found to predict psychological outcomes, including QoL or anxiety, regardless of time since diagnosis (9), distress (27), PTSS/PTSD (11,30,37), suicidal ideation (10), PTG (77), or benefit finding in long-term survivors (48). One study examining cross-sections of AYAs in different age brackets found that both ‘emerging adults’ (19-25 years old) and ‘young adults’ (26-39 years) had significantly higher general psychological distress and depression symptoms relative to adolescents aged 15-19, and the emerging adults also showed significantly greater anxiety than the adolescent group (55).
Gender
Studies that have examined the role of gender on psychological outcomes have fairly conclusively documented that, similar to general population findings (78,79), females report greater distress. As with general population data, researchers have suggested that this could reflect both a differential vulnerability to psychological distress, differences in the expression of this distress (e.g., PTS symptoms versus risk behaviors such as alcohol/substance abuse) or simply differences in the social acceptability of reporting this distress (39). In particular, studies to date have found that female gender is predictive of greater psychological distress (13,32,34,51,55,64), in particular persistent PTSS (12,39,47), poorer physical and mental health-related quality of life (HRQoL) (13,18,29,66,67), lower perceived social support (48), greater symptoms of depression and somatic distress (18,50,62), and anxiety/somatization (18,55,62) across the cancer trajectory.
However, some exceptions to this pattern have emerged. Some studies have documented that females and males showed similar levels of benefit finding in long-term survivorship (48), and not significantly different internalization or externalization symptoms (65), suicidal ideation (10), or PTG experiences (77). One recent study also found that male AYA survivors within five years post-treatment reported greater distress than did their female counterparts (27).
Cancer and treatment related factors
Much of the existing literature-in particular, survivorship research-has endeavored to identify risk and protective factors for psychological outcomes based on cancer and treatment-related factors. The rationale for much of this work has been to isolate easily identifiable, clinical or medical patient factors that may contribute to ‘profiling’ AYAs’ psychosocial risk, and thus facilitating more targeted intervention (13). In addition, the clear variability in the functional impact associated with different diagnoses and treatment regimens makes understanding their association with later adjustment an important aim.
Type of disease
A number of studies examining the impact of a young person’s specific cancer diagnosis on subsequent distress have found this to have no measurable impact on the incidence of PTSS/PTSD (25,31), depression symptoms (50), or psychological distress among either recently-diagnosed AYAs (57) or in long-term survivors (50-52). However, significant findings in this literature have tended to converge around a few cancer types. Sarcomas (bone and soft tissue tumors) have been associated with patients experiencing a poorer HRQoL (19,29,41), and a lower likelihood of endorsing PTG (21). This may be due in part to the impact of amputation on psychosocial functioning/QoL (64,69).
Brain and central nervous system (CNS) malignancies have also been identified as being associated with poorer physical and mental health HRQoL in longer-term survivorship (29,41,52) as well as a greater risk of suicidal ideation in long-term survivorship (10). Given the known higher incidence of late effects and impaired functioning among young survivors with bone and CNS malignancies in particular (80,81), these findings are perhaps not surprising. One study also identified higher rates of PTSD-specific distress, but not more general psychological distress, among solid tumor survivors relative to long-term leukemia/lymphoma survivors (49), while another study documented that survivors of leukemia/non-Hodgkins lymphoma who were not treated with cranial radiotherapy were more likely to experience PTSS, although there was no apparent reason for this result (39).
Disease severity
In line with findings related to several specific cancer types, objectively-rated cancer/disease severity per se has been repeatedly shown not to predict psychological outcomes among AYAs. In particular, studies have found that disease severity is not predictive of PTG or PTSS (22), fear of cancer recurrence among female cancer survivors (24), PTG in AYAs survivors (77), or general psychological distress among recently diagnosed AYAs (57). Furthermore, some studies have documented that having a cancer relapse, or a secondary malignant cancer is also not predictive of PTSD outcomes (25,46) or suicidal ideation in long-term survivorship (10).
Medical/physical burden
Consistent with an interpretation that specific cancer types might influence levels of distress via their impact on general functioning, a number of studies have found that experiencing a greater burden of medical side-effects during treatment, or late effects following treatment completion, is associated with greater psychological distress among AYAs. Experiencing ongoing physical symptoms could act as ongoing reminders of past traumatic experiences, and/or contribute to an ongoing sense of life threat (39).
Although there are some exceptions to this finding (25,51), many studies have found poorer physical health status/late effects (including cognitive/neurological late effects) to be associated with PTSS (31,39), clinically significant distress (13,27,32,38,49,51,52), poorer HRQoL (13,19,38,41,52,66,69,76), symptoms of anxiety and somatization (52), and beliefs about health-related competence (38) in long-term survivorship. One recent study also found that long-term survivors with poor self-reported physical health were almost three times more likely to report experiencing suicidal ideation (10). Of note, the association between poor physical health and suicidal ideation remained significant even after depression symptoms were controlled for (10). Longitudinal studies examining AYAs diagnosed within the past year found that greater reported treatment side-effects were associated with greater PTSS at a 6- and 12-month follow-up (56).
Treatment-related variables
The type, duration, and intensity of cancer treatment experienced by AYAs have repeatedly been examined as a potential modifier of later psychosocial outcomes. The combined results of these studies are mixed. A number of studies have documented that treatment-related factors are not predictive of depression, anxiety, or self-esteem either on- or off-treatment (60), PTSS/PTSD (25,31), higher psychological distress (51), suicidal ideation (10), or either parent- or teen-rated psychosocial QoL (82). By contrast, some studies have found treatment intensity to be associated with a significantly greater risk of PTSD (46,47), less positive health beliefs, and greater anxiety (38) and poorer general health and role functioning aspects of QoL (41) in long-term survivorship.
Studies exploring the impact of specific treatment modalities appear similarly inconclusive, with one apparent positive association for each null finding. For example, while surgical intervention was not related to levels of benefit finding in long-term survivorship in one study (48), in another, it predicted higher levels of PTSS at a 12-month follow-up, among AYAs diagnosed in the past year (56). Another study of young women with breast cancer also found that having radical surgery was associated with more body image concerns, which in turn was associated with greater symptoms of anxiety, depression, and fatigue (83). Similarly, intensive chemotherapy exposure predicted greater depressive symptoms in long-term survivorship in one study (50) but not psychological distress in another (51).
The associations appear clearest for cranial radiotherapy however, which appears predictive of a greater risk for PTSD (46), greater psychological distress and poorer HRQoL/wellbeing (13,64) in long-term survivorship, in particular when it occurred at <4 years of age (46). Again, like the findings for CNS malignancies, this is likely reflective of subsequent cognitive/neurological difficulties. Interestingly, one study found that not having a history of bone marrow transplantation was correlated with greater PTSS in longer-term survivorship (40). The authors speculated that this may be due to patients’ appraisals of a BMT being a near-miraculous ‘life saving’—rather than traumatic—procedure at the time.
Treatment status
Finally, treatment status (i.e., on versus off-treatment) and time since treatment completion have been examined across numerous studies. While in one study, being pre-treatment predicted depression and anxiety (17), being currently on-treatment has been found to be predictive of a poorer HRQoL (19,67), higher levels of PTSS (56) and significantly higher distress at any given point during a 12-month follow-up, while off-treatment status predicted lower distress (57) and HRQoL comparable to healthy controls (67).
A number of studies have also highlighted the occurrence of off-treatment distress among AYAs, however. One study comparing on- versus off-treatment adolescents found that the majority (86%) of the adolescents in their cohort who demonstrated clinical depression symptoms in their sample were off-treatment (60). Other studies have documented that in the off-treatment phase, being closer to the treatment-completion point (or fewer years post-diagnosis) predicted greater PTSS (12) and a greater likelihood of reporting depression symptoms and distress (52). A recent study examining AYAs cross-sectionally according to time since treatment found that the highest levels of distress were endorsed by AYAs who were 1-2 years post-treatment relative to AYAs who completed treatment either <1 year or 2-5 years ago, suggesting that the most vulnerable post-treatment period may be between 1-2 years since completing therapy (27).
Studies examining outcomes into longer-term survivorship have illustrated the potential longevity of AYAs’ distress, however. One study found that survivors within nine years of finishing treatment had significantly better mental health than did either survivors 9-18 years into survivorship, or those more than 18 years from diagnosis (29), while in another study, survivors reported greater cancer- and future-related worries the further in years they were from diagnosis (66). Symptoms of psychological distress, depression, and somatization, were significantly higher among one sample of survivors diagnosed >20 years previously, relative to AYAs diagnosed earlier than this (55). By contrast, several other studies have not found time since diagnosis or treatment to be predictive of later QoL or anxiety (9,52), PTSS/PTSD (11,25,30,31), depression symptoms or general psychological distress (50,52), however.
Socio-demographic factors
Increasingly, studies have turned their efforts towards identifying factors related to AYAs’ social standing (e.g., ethnicity, income, education, work status), that might influence their adaptation to cancer. These data suggest that AYAs who are socially disadvantaged in some way are likely to experience greater distress.
Educational status
Having a lower educational attainment has typically been found to be predictive of poorer physical HRQoL (13,19,52) and greater symptoms of PTSS/PTSD (39,46), depression and somatic distress (50,51), psychological distress (13,52) and suicidal ideation (10), in long-term survivorship. Relatedly, two North American studies documented Hispanic ethnicity to be predictive of poorer outcomes; in one, Hispanic ethnicity predicted poorer physical HRQoL (19), while another found that being English-speaking Hispanic was associated with lower PTG outcomes relative to either white non-Hispanics, or primarily Spanish-speaking Hispanics (21).
Economic factors
Indices of potential economic hardship and burden echo this pattern. Having a lower income has been associated with greater symptoms of PTSD (46), depression and somatic distress (50), and psychological distress (13,51,52,55), suicidal ideation (10), as well as poorer HRQoL (13,52) in long-term survivorship [cf: (27)]. North American studies that have documented health insurance status have also found that not having health insurance was associated with PTSS (40), and greater psychological distress and poorer HRQoL (13) in longer-term survivorship.
Occupational status
Data pertaining to AYAs’ study/work status appears to reflect the combined impact of pre-existing psychosocial vulnerabilities, together with the cumulative negative impact of significant study/career disruption. One early study documented that higher vocational satisfaction was associated with greater psychological wellbeing, while increased sick-leave from work was significantly related to lower wellbeing and a greater stress reaction among young survivors (64). Since then, numerous studies have linked current unemployment to more severe symptoms of depression and somatic distress (50), PTSS/PTSD (39,47), general psychological distress (13,51,52), suicidal ideation (10), poorer HRQoL (13,52,66), and a greater degree of cancer- and future-related worries (66) in longer-term survivorship, though one recent study did not replicate this finding among Korean survivors (55).
Two recent longitudinal studies have further highlighted the potentially protective aspects of being engaged in study/work: one study of recently diagnosed AYAs found that those who remained engaged with work/study post-diagnosis reported slight decreases in PTSS over time, those who stopped work due to cancer/treatment (but had been recently studying/working prior to diagnosis) showed no increases in distress, but that unemployment/not studying prior to diagnosis was a risk factor for increasing PTSS between a 6- and 12-month follow-up, regardless of changes in their employment/study status (56). Another longitudinal study of recently diagnosed AYAs followed up 6- and 12-month later found that being in school/employed at any given point was associated with lower distress (57). Finally, a study examining AYA outcomes across stages of post-treatment survivorship found that although there were no significant associations between cancer-related work/study interruption and distress in the first 12 months post-treatment, survivors who had finished treatment 1-5 years, and who reported educational/work interruption, reported significantly more psychological distress (27).
Research question 3: what mechanisms of action have been suggested by relevant theoretical models of AYA psychological adaptation to cancer, and what available evidence is there for these?
The preceding review documented several individual, cancer/treatment-related, and socio-demographic factors that tended to lead to a pattern of poorer functioning. These included female gender, a diagnosis during the adolescent/young adult years, a diagnosis of a more highly impairing cancer (e.g., CNS malignancy, Sarcoma), more substantial medical/late effects, as well as lower educational attainment, and significant, ongoing interruptions to study/work functioning. Beyond simply identifying these factors as a ‘profile’ of AYAs more vulnerable to distress, research efforts need to highlight potential pathways to intervention. Theoretical models may be useful in identifying putative causal mechanisms that can then be examined [e.g., see (5,46,84,85)]. Unfortunately, two recent reviews of psychological interventions for AYAs with cancer found few studies are anchored in a theoretical framework (86,87). A failure to identify the psychological mechanisms critical to cancer-related adjustment among AYAs in a theoretically-driven, evidence-based, manner is likely to hamper both screening efforts (i.e., the identification of distress) as well as the effectiveness of intervention (5,87).
A brief review of theoretical models relevant to AYAs follows, including the basic tenets and available evidence for each.
Developmental models
The theory
Developmental accounts of distress and psychological adaptation of AYAs highlight that the challenges involved in the cancer experience occur against a developmental trajectory—that of the movement towards independent functioning as an adult member of society (88). Consequently, as seen through the lens of developmental models, the emergence of distress or resilience is a function of the extent to which the illness interrupts key developmental tasks, and/or the extent to which the young person is able to negotiate these hurdles to normal, age-appropriate development.
Arnett’s [2000] model of emerging adulthood (89) is a particularly relevant example. ‘Emerging adulthood’ (the years from 18-25) is proposed to be a distinct period in which young people must focus on four key developmental tasks, including accepting responsibility for oneself, making independent decisions, establishing a relationship with one’s parent(s) as an equal adult, and being financially independent from one’s parent(s). During this period, young adults try on ‘possible selves’ as they move towards making commitments particularly in the areas of love, study and work (89). Consequently, the extent to which a cancer experience interferes with young people’s achievement of these goals-and their related activities-is likely to determine distress/adjustment thereafter.
The evidence
Much of the evidence for a developmental account of AYAs’ adjustment to illness is qualitative or descriptive in nature. The challenges involved with negotiating autonomy versus parental dependence, the distress related to the impact of cancer on sexuality/romantic relationships, and the importance of peer-related concerns all highlight the developmental impact of cancer (75,88,90). One recent study found that a number of the unmet needs reported by emerging adult cancer survivors related to these key developmental tasks (e.g., loss of independence) and in turn, having more unmet needs was associated with greater levels of anxiety and stress (91). Unlike younger cancer patients, AYAs also tend to grapple with the meaning of their cancer experience in the context of ‘who they are’, and this factor uniquely relates to their distress (36). Further, consistent with the functional goals of this period, the reviewed evidence linking study/work disruptions with distress seems compelling evidence to support the importance of being engaged with developmentally-appropriate tasks.
While this account of distress in AYAs is consistent with the unique issues that face AYAs, used in isolation, the developmental framework appears to lack some degree of explanatory power in accounting for psychological outcomes. That is, while cancer presumably disrupts the developmental goals of all AYAs to at least some degree, only a minority develop clinically relevant distress (92). Whether, and how, the disruption of identity development during the AYA years by cancer impacts long-term adjustment also remains poorly understood. Further, difficulty achieving a developmental task (e.g., being able to work/study) could both drive ongoing distress (as an underlying mechanism), or simply be a symptom of this maladaptation (an outcome). Consequently, although developmental models provide a useful backdrop to understanding the key issues facing AYAs living with cancer, they may not be able to fully account for individual differences in the development of distress due to their lack of identifiable, testable mechanisms.
Socio-ecological and family systems models
The theory
Not unlike developmental models, both socio-ecological and family systems models suggest that the quality of functioning within a family will be associated with, or even predictive of, the extent to which the young person is themselves able to adjust (93-95). Family-level factors such as communication (including appraisal of stressors and coping capacity), cohesiveness (emotional connection, support), flexibility/adaptation (responsiveness to change) and reciprocity within relationships, as well as effective coping skills, distress (and its expression), and resources are implicated as important determinants of how a family negotiates stressful events, and how the young person adapts. In a similar way, models accounting for the impact and importance of peer systems on AYA outcomes highlight the impact of both the structure (e.g., size, availability, frequency of contact) and function (e.g., subjective perceptions of supportiveness) of peer networks as predictors of AYA adjustment (86). The Adolescent Resilience Model (96) incorporates both social and family support as protective factors that assist young people in negotiating illness-related risks (illness uncertainty, disease and symptom-related distress).
The evidence
Of the reviewed studies, some found concordance between reports of parent and child distress, QoL and family functioning (82,97). Further, poorer family functioning/support (including single parent status) was associated with greater distress and worse psychological outcomes in AYAs (32,60,82). In fact, one study showed that adolescents with PTSD were over five times more likely to come from a poorly functioning family (28). Poorer communication, cohesion, and role-delineation factors in adolescent-parent relationships were also implicated in some studies, and were associated with worse mental health, self-esteem, and global competence (88), and worse psychosocial QoL for the adolescent (82). However, some studies have found that greater perceived family/social support actually predicted higher persistent PTSS (11,12), and worse depression symptoms among female AYAs (98) in survivorship, indicating that the link between family processes and psychological outcomes of AYAs may not be straightforward or completely understood. It is possible that these latter findings reflect distress associated with greater parental dependence, given that this is at odds with the developmental goal of the period (98).
Other forms of support also emerged as important in this review. Among older AYAs, being unmarried/not in a relationship predicted poorer physical aspects and mental health HRQoL (13,19,52), PTSD (46,47), greater psychological distress (13,49,51,52), and suicidal ideation (10), while living alone has been associated with PTSS in long-term survivorship (40). In support of functional models of social support, greater perceived social support was also associated with better perceived HRQoL (99), lower depression and anxiety symptoms (98), improved sexual functioning, self-worth, benefit finding, and depression symptoms in survivorship (48) and with better psychological and existential QoL, and less severe grief symptoms among AYAs with advanced cancer (100). Consequently, the pattern of evidence highlights the importance of social support in adjustment. The directionality of some of these findings may be difficult to determine, however, as just as a lack of social support may fuel symptoms of depression, so might distress (e.g., depression or PTSD) interfere with the behaviors needed to make friends, get married, and so forth.
Stress-coping models
The theory
Models of stress and coping have particularly dominated the psycho-oncology literature [e.g., (101-106)]. Typically, these are variants of Lazarus and Folkman’s (107) Transactional Model of Stress and Coping, which proposes that adjustment to a stressor such as cancer is mediated both by primary appraisals (evaluation of the implications of the threat), and secondary appraisals (evaluation of available coping resources). A person’s coping is thus determined by the interaction between their appraisal of the stressor being manageable (or not) given their available resources (e.g., family/friends, coping strategies, practical resources). Self-efficacy models extend these stress-coping formulations by specifying that in order to enact coping behaviors, an individual must appraise themselves as having coping skills or mastery within the specific problem situation (108).
Whilst these types of appraisals are taking place in a continuous manner, people are assumed to behaviorally respond either using problem-focused coping strategies (e.g., trying to directly solve/change the problem causing their distress) or by using emotion-focused coping (trying to regulate their distress surrounding a situation), and many people might use both approaches. These behavioral responses have also been conceptualized as approach/avoidance (109,110) or ‘primary’ and ‘secondary’ control (111) in other models. The adaptability of these coping styles may depend on the stage of the cancer trajectory. For example, more avoidant strategies (e.g., wishful thinking or denial) may be adaptive during the early stages of cancer treatment as an emotion regulation strategy, while persistent avoidance is likely to perpetuate distress due to ‘traumatic’ or distressing material not being processed and integrated into autobiographical memory (30,49,112).
The evidence
Studies that have examined coping styles among AYAs have found that having a greater cancer-related burden or ‘intrusion’ on functioning (e.g., longer treatment duration, experiencing radiotherapy/chemotherapy, being older at diagnosis) predicted AYAs’ using more passive/avoidant and less active coping strategies (113). In another study, coping factors explained significant portions of variance in anxiety, depression and somatization symptoms on the BSI-18 (38%), and rendered the relative contribution of medical late-effects non-significant, suggesting that cognitive variables may be more critical in determining how young people adjust than the impact of medical factors (49).
Across these studies, findings suggest that avoidant coping and emotion-focused coping strategies (e.g., optimism, perceived consequences, and perceived treatment control) and having a negative emotional representation of the illness, were related to distress (49), and worse HRQoL (113). Low optimism about the future course of the disease (49,113), and having a tendency to suppress negative thoughts (49) were also strongly predictive of poorer adaptation. This pattern of results portrays a profile of survivors vulnerable to ongoing distress about past experiences (via thought suppression strategies) and future-related hopelessness (via pessimism). These findings echo previous studies which found that more avoidant/repressive coping styles were associated with greater PTSD/distress (30), as lower wellbeing and higher stress (64), and greater self-reported fatigue (114), while enacting goal re-engagement and approach coping strategies (e.g., by using positive reappraisal) is associated with reporting positive changes since cancer (115,116). The importance of AYAs’ perceived self-efficacy to engage in such goal re-engagement and problem-solving behaviors is perhaps supported by one study which found that lower self-esteem was linked with greater cancer- and future-related worries (66).
Given that several studies suggest that using more proactive, problem-focused coping strategies are adaptive, stress and coping frameworks are intuitively appealing. However, although these studies highlight coping ‘profiles’ or styles associated with adaptation, they do not account for how AYAs might ‘arrive’ at the maladaptive coping appraisals, or why they might engage in an avoidant coping style that seems critical to their distress. Other authors have also noted that the tendency in the coping literature to align cognitive and behavioral ‘coping strategies’ as different options along a single continuum across a diversity of situations may not be particularly useful, and obscures the fact that cognitive factors (e.g., levels of emotional avoidance, active problem-solving) may in fact mediate behavioral outcomes (e.g., engagement in pleasant activities, information seeking) (117,118).
Cognitive appraisal models
The theory
Cognitive models extend stress-coping type formulations by focusing on how adaptive an individual’s appraisal of the illness event is. Such models argue that cognitive mechanisms which allow the cancer survivor to actively reconcile their ‘new knowledge’ of the world with their pre-existing assumptive structures may ultimately lead to a reduction in distress after the trauma, and more adaptive outcomes long-term. Across cognitive appraisal models, a common assumption is that a health crisis prompts patients to develop illness representations influenced by pre-existing belief structures. For example, Mishel’s (119) Uncertainty in Illness model predicts that the extent of people’s distress and/or adaptive coping in response to a serious illness is dependent upon their interpretations (or appraisals) of the inherent uncertainty involved in this illness as either (I) a threat or danger; or (II) a positive opportunity.
A set of cognitive models have also conceptualized cancer as a ‘trauma’ (12,120,121). In these models, distress (post-traumatic stress; PTS) and adaptation (PTG) is a function of the appraisals a person has about the trauma, and about the world/self in its aftermath. Meaning making theory proposes that confrontation with a severe stressor often leads to a shattering of global life assumptions, initiating cognitive processing to rebuild their meaning systems (122). According to Tedeschi and colleagues (123-125), the destruction of core schemas leads to a loss of coherence, perceived control and self-esteem regarding identity. The subsequent inability to reconcile the thoughts, images, and memories related to the trauma (e.g., cancer) with core beliefs, results in post-traumatic processes of intrusion and avoidance (122). By contrast, the process of making meaning is assumed to lead to better adjustment, although whether this occurs via a process of effortful, positive reappraisal (and suffering) (125), or simply via positive reinterpretations of the cancer experience (126) is a topic of contention in the literature (71).
The evidence
Given the potential relevance of cognitive models to explain psychological outcomes in AYAs, the number of studies exploring the relationship between such variables and psychological outcomes is small. Several studies have linked the experience of prior/concurrent life stressors (e.g., school difficulties; parental separation/divorce) to PTSS (12) and distress in survivorship (32). However, most studies have focused on the relationship between illness-related cognitions and distress. Optimism about prognosis predicted improved HRQoL among AYA cancer survivors in one study, independent of actual health status (69). Additionally, survivors who have had PTSD since completing treatment have shown perceptions of greater current life threat, and of cancer treatment intensity (23,44), as well as perceiving a greater, more negative impact of stressful/traumatic life events, cancer-related late effects, and impact on life goals, relative to survivors without PTSD (44). Appraisals regarding the extent to which treatment was difficult, ‘scary’, or life-threatening, have been shown to predict PTSS (12), PTG (22) and distress in survivorship (49), while perceptions of cancer having had a generally more negative impact have been linked to distress (27), poorer psychosocial functioning (52), worse anxiety and self-esteem (127), and QoL (52) as have perceptions of having more unmet needs (17), even years into survivorship. These associations may reflect broader alterations to AYAs’ beliefs about the world, their life, or their future; however this were not measured in these studies.
The impact of illness-related appraisals on adjustment may be particularly marked among AYAs because of their age. That is, AYAs may be prone to experiencing cancer as more life-threatening, inexplicable, and burdensome than their younger counterparts, who may lack the cognitive capacity for this level of existential/abstract thought (2,89), or older adults, who are likely to have more life experience with illness (and for whom illness is a more expected event) (24). Consistent with this, recent research has found that the intrusiveness of illness-related thoughts was predictive of fear of cancer recurrence symptoms among younger women with breast cancer, and consistently explained the relationship found in this study between younger age and distress (24). The authors hypothesized that the developmental incongruity of the cancer diagnosis in the young adult years may make this reality seem more unexpected, which could lead to difficulty integrating this reality into new beliefs about the world.
Relatedly, recent studies have highlighted that AYAs who identify more strongly with a ‘survivor’ identity show better psychological well-being and PTG, than those who describe themselves as a cancer ‘victim’ (128). This finding suggests that AYAs may need to first integrate and process their cancer experience (and put it in their past, as a ‘survivor’) before growth can take place. The cognitive processes involved in AYAs reaching this ‘identity’ remain a little unclear, however. One study found that engaging in thought suppression strategies for negative thoughts was associated with significantly higher psychological distress in long-term survivorship (49), while another found that individuals’ propensity to engage in either positive or negative cancer-related attentional biases and rumination was associated with subsequent psychological outcomes (where negative rumination partially mediated PTSD outcomes, and ‘positive rumination’ partially mediated PTG outcomes) (129). Such cognitive processes may account for the impact of medical factors (e.g., illness severity), individual characteristics (e.g., previous experience) and the generation of adaptive cognitive appraisals and integration of the cancer experience (130,131).
In sum, cognitive models of adaptation indicate that several types of cognitive appraisals are linked with maladaptation, such as greater perceptions of burden, life threat, and illness severity. However, much of this literature has been descriptive or cross-sectional. Given the lack of longitudinal or experimental data, it is unclear (I) to what extent these types of appraisals may reflect actual, objective burdens; and (II) to what extent such appraisal processes might be causal mechanisms, or simply a symptomatic facet of a post-cancer distress syndrome. Evidence for the relationship between ‘positive’ and ‘negative’ facets of adjustment also remains mixed.
In the midst of a developmental period where AYAs are forming a sense of self and future life goals, the present review highlights that how they appraise their cancer experience, how they view themselves as cancer patients/survivors, and how well they are able to problem-solve and re-engage with goals, is associated with their subsequent adaptation. These converging lines of evidence point to the potential importance of understanding how autobiographical memory and future thinking mechanisms might shape the psychological outcomes of AYAs living with cancer. The potential role of such mechanisms remains understudied and poorly understood within the current literature, however. The next section of this review examines empirical advancements in non-oncology fields that may be relevant in identifying and testing mechanisms of adaptation among AYAs.
Research question 4: what empirical advancements in adjacent, non-oncology fields have been made that might improve our understanding of psychological outcomes in AYAs living with cancer?
Researchers have recently highlighted that endeavours to identify and test mechanisms will necessarily involve a greater degree of cross-pollination between those conducting clinical-level interventions research, and those conducting experimental manipulations of putative mechanisms (5). Given the developmental relevance of how AYAs process and integrate their cancer experience into their past, draw from it in their present, and incorporate it into their future goals, it seems appropriate to draw from recent developments in the broader psychology literature pertaining to autobiographical memory, future imaginings, and the self.
Recent models of the self and its roots in autobiographical memory may be used to explain how the disruption of cancer may affect a person’s ongoing goals and sense of self. Two recent models of autobiographical memory may be particularly relevant. The Self-Memory System (132) highlights that a person’s current goals and assumptions about the world provide a stable lens for their current sense of self, goals, and predictions for the future. Consequently, according to this model, negative psychological outcomes may emerge when young people selectively draw upon memories/future imaginings consistent with current psychological concerns (e.g., past cancer threat, fear of future cancer recurrence, sense of personal vulnerability). This model highlights the importance of the content of memory/future thinking–what young people remember and imagine (e.g., preoccupied with illness). The CaR-FA-X theory (which identifies ‘capture and rumination, functional avoidance, and executive control’ processes) (133) recently built upon this by emphasizing the role of memory specificity-the way people remember the past or imagine the future.
According to the CaR-FA-X theory, overgeneral, categorical memories (e.g., “All of the times chemotherapy was hard.”) which are summaries of events across time, rather than specific, episodic memories that occurred on a particular day (e.g., “That afternoon last month where my friend came and chatted to me in hospital.”). Specific memories are associated with psychological functioning outcomes as people use these situational memories as useful analogues from which to imagine their future, and draw alternative, useful solutions to problems. Consequently, overgeneral memory has been shown to impair people’s current ability to problem-solve (134,135) and their capacity to imagine the future in a clear, concrete manner (136). These effects have been shown among clinically depressed (137,138), complicated grief (139-141), and PTSD samples (142,143), as well as among healthy student AYA populations (144). Memory specificity has also been shown to be responsive to ruminative thinking processes (137,138,144), which has been hypothesized as an important factor in the maintenance of fear of cancer recurrence (145,146). Importantly, the mechanisms outlined in these models can be examined empirically using tasks such as the Autobiographical Memory Test and the Future Imaginings Task (136), while related outcomes of interest, such as social problem-solving, have been previously studied outside of oncology using the Means-Ends Problem-Solving Task (147).
In taking such a lateral, process-based approach to experimentally investigating suggested mechanisms of adjustment, a second important component is to devise non-clinical (e.g., non-cancer/illness) paradigms in which to test psychological mechanisms related to adjustment. For example, otherwise healthy young people who show significant preoccupation with, and anxiety about, their health and the potential for future illness (i.e., health anxious young people) may provide an useful analogue sample in which to study processes related to how young people with active illness-related concerns process both illness- and non-illness-related tasks, remember illness-related events, and imagine their futures.
Such an analogue sample removes the actuality of ‘cancer’ from the picture, and yet in both samples, young people perceive their risks of future illness to be high, are anxious about this, and exhibit cognitive and behavioral responses driven by this. Removing the impact of physical illness on outcomes is a benefit of experimental studies, as the preceding review indicates that distress long into survivorship is not solely accounted for by late effects/physical health. Understanding the maintenance of distress with the ‘noise’ of physical symptoms removed from the data may be an important step towards understanding distress in long-term cancer survivorship.
This approach rests on a number of important assumptions. The first is that it is possible to examine illness-concerns in the laboratory (with some degree of ecological validity). Secondly, that the way in which young people process illness-concerns in the laboratory has important implications for how they process illness-concerns in a real-life situation (generalizability). Finally, that the processes involved in managing illness concerns (e.g., thinking styles, avoidance behaviors) are likely to be common, whether or not someone actually has an illness (i.e., the way our minds work doesn’t fundamentally change once we are diagnosed with cancer). These assumptions are supported by analyses indicating that health/illness concerns vary on a continuum of severity, with common mechanisms driving these concerns along this continuum (148).
Such experimental paradigms are already emerging. Among healthy AYA analogue samples, studies have shown that ‘bracing’ for an imminent medical test result impairs the ability to process important information both immediately before and after receiving it (149), while a self-affirmation intervention prior to giving individuals feedback about their vulnerability to a health-risk reduces both their defensiveness in receiving this information, and their subsequent self-reported health-risk behaviors (150). Recent studies using experimentally-induced ‘mortality salience’ (awareness of one’s own eventual death) have found that individuals who are led to perceive that they are at high risk of cancer will first tend to engage in thought suppression of cancer/death-related thoughts (presumably as an emotion regulation strategy); yet, when this is prevented, they report decreased cancer-related self-examination intentions (151).
Taking such an approach has the advantage of enabling us to strengthen the science behind the interventions that we believe, for many other reasons, are likely to be useful among AYAs (e.g., cognitive-behavioral therapy, mindfulness) (87). By identifying, manipulating, and testing cognitive and behavioral processes important to adjustment in AYAs, such interventions can be tailored to the specific mechanisms that appear important for AYAs. In turning to process-focused, empirical studies to spotlight processes potentially involved in cancer-related adaptation among AYAs, we also address clinical considerations, such as the desire not to overwhelm an already vulnerable population with research study requests. This kind of approach—studying the hypothesized process, rather than solely studying the population—may be especially important in AYAs given their scarcity as a sample to study, among other challenges (152).
Future research directions
To date, the body of evidence on the psychological outcomes of AYAs highlights a number of factors that may play a role. There is, however, a paucity of evidence relating to modifiable processes, such as cognitive or behavioral factors, that may impact the psychological adjustment of AYAs through their cancer trajectory. Understanding better how people manage to engage in processes of reappraisal, meaning making, and goal readjustment under these circumstances seems critical to explaining why some cancer survivors fare better psychologically into survivorship.
Much research has explored the way in which the cancer experience can shatter peoples’ global assumptions, related to the self, others, and the world (153). These models implicate peoples’ constructed identities as a focus of reconstruction in the aftermath of cancer. This biographical disruption is especially challenging for AYAs, for whom a sense of self may be still fluid and in the process of development (89). Adjusting and integrating useful appraisals regarding the threat of cancer to the self has been conceptualized as an ongoing struggle for the cancer survivor, in response not only to internal discrepancies in assumptions about the world, but also the ubiquitous reminders of this threat (131). Whilst integrating the cancer experience, the survivor must nevertheless avoid it overshadowing their sense of ‘self’. Recent theoretical models have begun to incorporate such processes in their accounts of adaptation (154), however the manner in which patients arrive at this identity, or maintain this sense of self, remains largely unstudied.
Further, although numerous studies have documented the impact of cancer on AYAs’ qualitative narratives, no studies have experimentally examined the impact on particular cognitive or behavioral processes on how AYAs integrate cancer-related cognitions into autobiographical memory, on how they imagine their future lives, and how they subsequently craft life goals for themselves in the aftermath of the cancer experience. These processes are not only critical to adaptation, but are also amenable to intervention (141). Future experimental studies isolating and exploring processes of memory, future thinking, goal-setting, and the navigation of challenges through problem-solving, may be important. Studies of psychological processes that may have a maladaptive impact on these psychological efforts (e.g., cancer-related worry, rumination, or behavioral aspects such as avoidance and withdrawal) are also needed in the oncology domain.
Focusing on common psychological mechanisms that may underpin both distress and adaptation may also help to integrate the range of findings by moving away from disorder-specific of adaptation. Current models of psychological distress and adaptation have frequently centered on a trauma-model of distress, despite the fact that studies consistently find that only a minority (typically, not more than 20-30%) meet criteria for clinically-significant PTSS. There are also important conceptual distinctions that make a trauma framework an imperfect ‘fit’ for accounting for post-cancer psychological reactions (121,155). Consequently, while a trauma framework might account for the responses of a minority, it does not advance our understanding of how the remainder of these samples of AYAs adjust to their cancer experience. By contrast, processes such as autobiographical memory, future thinking, problem-solving, and goal-setting are universally important processes to psychological functioning among both well-functioning and various distressed populations (133,156-159). Given the universality of these psychological processes, understanding how they can be both maladaptive and adaptive will enable the shift from a body of research focused on psychopathology, to a focus on the dual outcomes of distress and resilience (160).
The recent international spotlight on AYAs with cancer is juxtaposed with the reality of increasingly resource-constrained healthcare settings worldwide (161). Given this, honing the science behind our efforts to assist AYAs to adjust to cancer is crucial. In this context, tightening approaches to effective intervention becomes even more important. Identifying theoretically-grounded mechanisms, testing these, and building a body of evidence around psychological processes using experimental settings (and possibly, analogue samples of healthy AYA populations) will facilitate the development of more effective psychosocial interventions for AYAs living with cancer.
Acknowledgements
Ms Ursula Sansom-Daly is supported by Leukaemia Foundation of Australia PhD Scholarship. Dr Wakefield is supported by a Career Development Award from the National Health and Medical Research Council (ID 1067501) and an Early Career Development Award from the Cancer Institute of NSW (ID 11/ECF/3-43). The Behavioural Sciences Unit at Sydney Children’s Hospital is supported by the Kids with Cancer Foundation. This project was supported by a project grant awarded by Cancer Australia and Beyond Blue. The authors also wish to acknowledge A/Prof Richard Cohn, Ms Sarah Ellis, Ms Sanaa Mathur, Ms Emma Doolan, Ms Helen Wilson, and Ms Brittany McGill from the School of Women’s and Children’s Health, The University of New South Wales.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Erikson EH. eds. Identity and the life cycle. New York, NY: Norton, 1980.
- Havighurst RJ. eds. Developmental tasks and education. 3rd ed. New York, NY: David McKay Co, 1972.
- Butow P, Palmer S, Pai A, et al. Review of adherence-related issues in adolescents and young adults with cancer. J Clin Oncol 2010;28:4800-9. [PubMed]
- Phillips-Salimi CR, Lommel K, Andrykowski MA. Physical and mental health status and health behaviors of childhood cancer survivors: findings from the 2009 BRFSS survey. Pediatr Blood Cancer 2012;58:964-70. [PubMed]
- Stanton AL, Luecken LJ, MacKinnon DP, et al. Mechanisms in psychosocial interventions for adults living with cancer: opportunity for integration of theory, research, and practice. J Consult Clin Psychol 2013;81:318-35. [PubMed]
- Zebrack BJ. Psychological, social, and behavioral issues for young adults with cancer. Cancer 2011;117:2289-94. [PubMed]
- Seitz DC, Besier T, Goldbeck L. Psychosocial interventions for adolescent cancer patients: a systematic review of the literature. Psychooncology 2009;18:683-90. [PubMed]
- Aubin S, Barr R, Rogers P, et al. What should the age range be for AYA oncology? J Adolesc Young Adult Oncol 2011;1:3-10.
- Oren A, Benoit MA, Murphy A, et al. Quality of life and anxiety in adolescents with differentiated thyroid cancer. J Clin Endocrinol Metab 2012;97:E1933-7. [PubMed]
- Recklitis CJ, Diller LR, Li X, et al. Suicide ideation in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 2010;28:655-61. [PubMed]
- Kazak AE, Barakat LP, Meeske K, et al. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. J Consult Clin Psychol 1997;65:120-9. [PubMed]
- Stuber ML, Kazak AE, Meeske K, et al. Predictors of posttraumatic stress symptoms in childhood cancer survivors. Pediatrics 1997;100:958-64. [PubMed]
- Zeltzer LK, Lu Q, Leisenring W, et al. Psychosocial outcomes and health-related quality of life in adult childhood cancer survivors: a report from the Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev 2008;17:435-46. [PubMed]
- Hedström M, Ljungman G, von Essen L. Perceptions of distress among adolescents recently diagnosed with cancer. J Pediatr Hematol Oncol 2005;27:15-22. [PubMed]
- Phillips-Salimi CR, Andrykowski MA. Physical and mental health status of female adolescent/young adult survivors of breast and gynecological cancer: a national, population-based, case-control study. Support Care Cancer 2013;21:1597-604. [PubMed]
- Allen R, Newman SP, Souhami RL. Anxiety and depression in adolescent cancer: Findings in patients and parents at the time of diagnosis. Eur J Cancer 1997;33:1250-5. [PubMed]
- Dyson GJ, Thompson K, Palmer S, et al. The relationship between unmet needs and distress amongst young people with cancer. Support Care Cancer 2012;20:75-85. [PubMed]
- Mattsson E, El-Khouri B, Ljungman G, et al. Empirically derived psychosocial states among adolescents diagnosed with cancer during the acute and extended phase of survival. Ann Oncol 2009;20:1722-7. [PubMed]
- Smith AW, Bellizzi KM, Keegan TH, et al. Health-related quality of life of adolescent and young adult patients with cancer in the United States: the Adolescent and Young Adult Health Outcomes and Patient Experience study. J Clin Oncol 2013;31:2136-45. [PubMed]
- Zabora J, Brintzenhofeszoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psychooncology 2001;10:19-28. [PubMed]
- Arpawong TE, Oland A, Milam JE, et al. Post-traumatic growth among an ethnically diverse sample of adolescent and young adult cancer survivors. Psychooncology 2013. [Epub ahead of print]. [PubMed]
- Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. J Pediatr Psychol 2006;31:413-9. [PubMed]
- Hobbie WL, Stuber M, Meeske K, et al. Symptoms of posttraumatic stress in young adult survivors of childhood cancer. J Clin Oncol 2000;18:4060-6. [PubMed]
- Lebel S, Beattie S, Arès I, et al. Young and worried: age and fear of recurrence in breast cancer survivors. Health Psychol 2013;32:695-705. [PubMed]
- Schwartz L, Drotar D. Posttraumatic stress and related impairment in survivors of childhood cancer in early adulthood compared to healthy peers. J Pediatr Psychol 2006;31:356-66. [PubMed]
- Servitzoglou M, Papadatou D, Tsiantis I, et al. Psychosocial functioning of young adolescent and adult survivors of childhood cancer. Support Care Cancer 2008;16:29-36. [PubMed]
- Yanez B, Garcia SF, Victorson D, et al. Distress among young adult cancer survivors: a cohort study. Support Care Cancer 2013;21:2403-8. [PubMed]
- Alderfer MA, Navsaria N, Kazak AE. Family functioning and posttraumatic stress disorder in adolescent survivors of childhood cancer. J Fam Psychol 2009;23:717-25. [PubMed]
- Chan CW, Choi KC, Chien WT, et al. Health-related quality-of-life and psychological distress of young adult survivors of childhood cancer in Hong Kong. Psychooncology 2013. [Epub ahead of print]. [PubMed]
- Erickson SJ, Steiner H. Trauma and personality correlates in long-term pediatric cancer survivors. Child Psychiatry Hum Dev 2001;31:195-213. [PubMed]
- Gerhardt CA, Yopp JM, Leininger L, et al. Brief report: post-traumatic stress during emerging adulthood in survivors of pediatric cancer. J Pediatr Psychol 2007;32:1018-23. [PubMed]
- Gianinazzi ME, Rueegg CS, Wengenroth L, et al. Adolescent survivors of childhood cancer: are they vulnerable for psychological distress? Psychooncology 2013;22:2051-8. [PubMed]
- Gianinazzi ME, Rueegg CS, von der Weid NX, et al. Mental health-care utilization in survivors of childhood cancer and siblings: the Swiss childhood cancer survivor study. Support Care Cancer 2013. [Epub ahead of print]. [PubMed]
- Kamibeppu K, Sato I, Honda M, et al. Mental health among young adult survivors of childhood cancer and their siblings including posttraumatic growth. J Cancer Surviv 2010;4:303-12. [PubMed]
- Kazak AE, Meadows AT. Families of young adolescents who have survived cancer: social-emotional adjustment, adaptability, and social support. J Pediatr Psychol 1989;14:175-91. [PubMed]
- Kazak AE, Barakat LP, Alderfer M, et al. Posttraumatic stress in survivors of childhood cancer and mothers: development and validation of the Impact of Traumatic Stressors Interview Schedule (ITSIS). J Clin Psychol Med Settings 2001;8:307-23.
- Kazak AE, Alderfer M, Rourke MT, et al. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol 2004;29:211-9. [PubMed]
- Kazak AE, DeRosa BW, Schwartz LA, et al. Psychological outcomes and health beliefs in adolescent and young adult survivors of childhood cancer and controls. J Clin Oncol 2010;28:2002-7. [PubMed]
- Langeveld NE, Grootenhuis MA, Voûte PA, et al. Posttraumatic stress symptoms in adult survivors of childhood cancer. Pediatr Blood Cancer 2004;42:604-10. [PubMed]
- Lee YL, Santacroce SJ. Posttraumatic stress in long-term young adult survivors of childhood cancer: a questionnaire survey. Int J Nurs Stud 2007;44:1406-17. [PubMed]
- Maunsell E, Pogany L, Barrera M, et al. Quality of life among long-term adolescent and adult survivors of childhood cancer. J Clin Oncol 2006;24:2527-35. [PubMed]
- Meeske KA, Ruccione K, Globe DR, et al. Posttraumatic stress, quality of life, and psychological distress in young adult survivors of childhood cancer. Oncol Nurs Forum 2001;28:481-9. [PubMed]
- Recklitis CJ, Parsons SK, Shih MC, et al. Factor structure of the brief symptom inventory-18 in adult survivors of childhood cancer: results from the childhood cancer survivor study. Psychol Assess 2006;18:22-32. [PubMed]
- Rourke MT, Hobbie WL, Schwartz L, et al. Posttraumatic stress disorder (PTSD) in young adult survivors of childhood cancer. Pediatr Blood Cancer 2007;49:177-82. [PubMed]
- Seitz DC, Besier T, Debatin KM, et al. Posttraumatic stress, depression and anxiety among adult long-term survivors of cancer in adolescence. Eur J Cancer 2010;46:1596-606. [PubMed]
- Stuber ML, Meeske KA, Krull KR, et al. Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics 2010;125:e1124-34. [PubMed]
- Stuber ML, Meeske KA, Leisenring W, et al. Defining medical posttraumatic stress among young adult survivors in the Childhood Cancer Survivor Study. Gen Hosp Psychiatry 2011;33:347-53. [PubMed]
- Teall T, Barrera M, Barr R, et al. Psychological resilience in adolescent and young adult survivors of lower extremity bone tumors. Pediatr Blood Cancer 2013;60:1223-30. [PubMed]
- Wenninger K, Helmes A, Bengel J, et al. Coping in long-term survivors of childhood cancer: relations to psychological distress. Psychooncology 2013;22:854-61. [PubMed]
- Zebrack BJ, Zeltzer LK, Whitton J, et al. Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin’s disease, and non-Hodgkin’s lymphoma: a report from the Childhood Cancer Survivor Study. Pediatrics 2002;110:42-52. [PubMed]
- Zebrack BJ, Gurney JG, Oeffinger K, et al. Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivor study. J Clin Oncol 2004;22:999-1006. [PubMed]
- Zebrack BJ, Landier W. The perceived impact of cancer on quality of life for post-treatment survivors of childhood cancer. Qual Life Res 2011;20:1595-608. [PubMed]
- Decker CL, Haase JE, Bell CJ. Uncertainty in adolescents and young adults with cancer. Oncol Nurs Forum 2007;34:681-8. [PubMed]
- Jörngården A, Mattsson E, von Essen L. Health-related quality of life, anxiety and depression among adolescents and young adults with cancer: a prospective longitudinal study. Eur J Cancer 2007;43:1952-8. [PubMed]
- Kim MA, Yi J. Psychological distress in adolescent and young adult survivors of childhood cancer in Korea. J Pediatr Oncol Nurs 2013;30:99-108. [PubMed]
- Kwak M, Zebrack BJ, Meeske KA, et al. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psychooncology 2013;22:1798-806. [PubMed]
- Kwak M, Zebrack BJ, Meeske KA, et al. Trajectories of psychological distress in adolescent and young adult patients with cancer: a 1-year longitudinal study. J Clin Oncol 2013;31:2160-6. [PubMed]
- Larsson G, Mattsson E, von Essen L. Aspects of quality of life, anxiety, and depression among persons diagnosed with cancer during adolescence: a long-term follow-up study. Eur J Cancer 2010;46:1062-8. [PubMed]
- Tebbi CK, Bromberg C, Mallon JC. Self-reported depression in adolescent cancer patients. Am J Pediatr Hematol Oncol 1988;10:185-90. [PubMed]
- von Essen L, Enskär K, Kreuger A, et al. Self-esteem, depression and anxiety among Swedish children and adolescents on and off cancer treatment. Acta Pædiatr 2000;89:229-36. [PubMed]
- Walker AJ, Gedaly-Duff V, Miaskowski C, et al. Differences in symptom occurrence, frequency, intensity, and distress in adolescents prior to and one week after the administration of chemotherapy. J Pediatr Oncol Nurs 2010;27:259-65. [PubMed]
- Allen R, Newman SP, Souhami RL. Anxiety and depression in adolescent cancer: findings in patients and parents at the time of diagnosis. Eur J Cancer 1997;33:1250-5. [PubMed]
- Derogatis LR. Brief Symptom Inventory (BSI)-18: administration, scoring, and procedures manual. Minneapolis, MN: NCS Pearson, 2000.
- Zevon MA, Neubauer NA, Green DM. Adjustment and vocational satisfaction of patients treated during childhood or adolescence for acute lymphoblastic leukemia. Am J Pediatr Hematol Oncol 1990;12:454-61. [PubMed]
- Trask PC, Paterson AG, Trask CL, et al. Parent and adolescent adjustment to pediatric cancer: associations with coping, social support, and family function. J Pediatr Oncol Nurs 2003;20:36-47. [PubMed]
- Langeveld NE, Grootenhuis MA, Voute PA, et al. Quality of life, self-esteem and worries in young adult survivors of childhood cancer. Psychooncology 2004;13:867-81. [PubMed]
- Wu E, Robison LL, Jenney ME, et al. Assessment of health-related quality of life of adolescent cancer patients using the Minneapolis-Manchester Quality of Life Adolescent Questionnaire. Pediatr Blood Cancer 2007;48:678-86. [PubMed]
- Hall AE, Boyes AW, Bowman J, et al. Young adult cancer survivors’ psychosocial well-being: a cross-sectional study assessing quality of life, unmet needs, and health behaviors. Support Care Cancer 2012;20:1333-41. [PubMed]
- Stam H, Grootenhuis MA, Caron HN, et al. Quality of life and current coping in young adult survivors of childhood cancer: positive expectations about the further course of the disease were correlated with better quality of life. Psychooncology 2006;15:31-43. [PubMed]
- Tedeschi RG, Calhoun LG. Beyond the concept of recovery: growth and the experience of loss. Death Stud 2008;32:27-39. [PubMed]
- Sumalla EC, Ochoa C, Blanco I. Posttraumatic growth in cancer: reality or illusion? Clin Psychol Rev 2009;29:24-33. [PubMed]
- Berger R, Weiss T. The post-traumatic growth model: an expansion to the family system. Traumatology 2009;15:63-74.
- Cantrell MA, Conte TM. Between being cured and being healed: the paradox of childhood cancer survivorship. Qual Health Res 2009;19:312-22. [PubMed]
- Wakefield CE, McLoone J, Goodenough B, et al. The psychosocial impact of completing childhood cancer treatment: a systematic review of the literature. J Pediatr Psychol 2010;35:262-74. [PubMed]
- Wakefield CE, McLoone JK, Fleming CAK, et al. Adolescent cancer and health-related decision-making: an Australian multi-perspective family analysis of appointment attendance and involvement in medical and lifestyle choices. J Adolesc Young Adult Oncol 2011/2012;1:173-80.
- Zebrack BJ, Chesler MA. Quality of life in childhood cancer survivors. Psychooncology 2002;11:132-41. [PubMed]
- Love C, Sabiston CM. Exploring the links between physical activity and posttraumatic growth in young adult cancer survivors. Psychooncology 2011;20:278-86. [PubMed]
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593-602. [PubMed]
- Kessler RC, McGonagle KA, Swartz M, et al. Sex and depression in the National Comorbidity Survey. I: lifetime prevalence, chronicity and recurrence. J Affect Disord 1993;29:85-96. [PubMed]
- Mitby PA, Robison LL, Whitton JA, et al. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer 2003;97:1115-26. [PubMed]
- Nagarajan R, Neglia JP, Clohisy DR, et al. Education, employment, insurance, and marital status among 694 survivors of pediatric lower extremity bone tumors: a report from the childhood cancer survivor study. Cancer 2003;97:2554-64. [PubMed]
- Barakat LP, Marmer PL, Schwartz LA. Quality of life of adolescents with cancer: family risks and resources. Health Qual Life Outcomes 2010;8:63. [PubMed]
- Rosenberg SM, Tamimi RM, Gelber S, et al. Body image in recently diagnosed young women with early breast cancer. Psychooncology 2013;22:1849-55. [PubMed]
- Evan EE, Zeltzer LK. Psychosocial dimensions of cancer in adolescents and young adults. Cancer 2006;107:1663-71. [PubMed]
- Patterson P, Millar B, Desille N. The needs of young people who have, or have had, cancer: Report on the CanTeen National Member Survey for Patient Members 2008. Sydney, Australia: CanTeen Australia.
- Decker CL. Social support and adolescent cancer survivors: a review of the literature. Psychooncology 2007;16:1-11. [PubMed]
- Sansom-Daly UM, Peate M, Wakefield CE, et al. A systematic review of psychological interventions for adolescents and young adults living with chronic illness. Health Psychol 2012;31:380-93. [PubMed]
- Rait DS, Ostroff JS, Smith K, et al. Lives in a balance: perceived family functioning and the psychosocial adjustment of adolescent cancer survivors. Fam Process 1992;31:383-97. [PubMed]
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 2000;55:469-80. [PubMed]
- D’Agostino NM, Penney A, Zebrack B. Providing developmentally appropriate psychosocial care to adolescent and young adult cancer survivors. Cancer 2011;117:2329-34. [PubMed]
- Millar B, Patterson P, Desille N. Emerging adulthood and cancer: how unmet needs vary with time-since-treatment. Palliat Support Care 2010;8:151-8. [PubMed]
- Zeltzer LK, Recklitis C, Buchbinder D, et al. Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Clin Oncol 2009;27:2396-404. [PubMed]
- Patterson JM. Families experiencing stress: I. The family adjustment and adaptation response model: II. Applying the FAAR model to health-related issues for intervention and research. Fam Syst Med 1988;6:202-37.
- Patterson JM. Understanding family resilience. J Clin Psychol 2002;58:233-46. [PubMed]
- Patterson JM, Holm KE, Gurney JG. The impact of childhood cancer on the family: a qualitative analysis of strains, resources, and coping behaviors. Psychooncology 2004;13:390-407. [PubMed]
- Haase JE. The adolescent resilience model as a guide to interventions. J Pediatr Oncol Nurs 2004;21:289-99; discussion 300-4. [PubMed]
- Robinson KE, Gerhardt CA, Vannatta K, et al. Survivors of childhood cancer and comparison peers: the influence of early family factors on distress in emerging adulthood. J Fam Psychol 2009;23:23-31. [PubMed]
- Corey AL, Haase JE, Azzouz F, et al. Social support and symptom distress in adolescents/young adults with cancer. J Pediatr Oncol Nurs 2008;25:275-84. [PubMed]
- Cantrell MA, Lupinacci P. Investigating the determinants of health-related quality of life among childhood cancer survivors. J Adv Nurs 2008;64:73-83. [PubMed]
- Trevino KM, Fasciano K, Block S, et al. Correlates of social support in young adults with advanced cancer. Support Care Cancer 2013;21:421-9. [PubMed]
- Chesler M, Barbarin O. Childhood cancer and the family: meeting the challenge of stress and support. New York: Brunner/Routledge, 1987.
- Deimling GT, Kahana B, Bowman KF, et al. Cancer survivorship and psychological distress in later life. Psychooncology 2002;11:479-94. [PubMed]
- Scott DW, Oberst MT, Dropkin MJ. A stress-coping model. ANS Adv Nurs Sci 1980;3:9-23. [PubMed]
- Zabora JR, Loscalzo MJ, Weber J. Managing complications in cancer: identifying and responding to the patient’s perspective. Semin Oncol Nurs 2003;19:1-9. [PubMed]
- Miedema B, Hamilton R, Easley J. From “invincibility” to “normalcy”: coping strategies of young adults during the cancer journey. Palliat Support Care 2007;5:41-9. [PubMed]
- Decker CL. Coping in adolescents with cancer: a review of the literature. J Psychosoc Oncol 2006;24:123-40. [PubMed]
- Lazarus RS, Folkman S. eds. Stress, appraisal and coping. New York: Springer Publishing Company, 1984.
- Merluzzi TV, Nairn RC, Hegde K, et al. Self-efficacy for coping with cancer: revision of the Cancer Behavior Inventory (version 2.0). Psychooncology 2001;10:206-17. [PubMed]
- Ebata AT, Moos RH. Coping and adjustment in distressed and healthy adolescents. J Appl Dev Psychol 1991;12:33-54.
- Phipps S, Fairclough D, Mulhern RK. Avoidant coping in children with cancer. J Pediatr Psychol 1995;20:217-32. [PubMed]
- Rothbaum F, Weisz JR, Snyder SS. Changing the world and changing the self: a two-process model of perceived control. J Pers Soc Psychol 1982;42:5-37.
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther 2000;38:319-45. [PubMed]
- Maurice-Stam H, Oort FJ, Last BF, et al. A predictive model of health-related quality of life in young adult survivors of childhood cancer. Eur J Cancer Care (Engl) 2009;18:339-49. [PubMed]
- Daniel LC, Brumley LD, Schwartz LA. Fatigue in adolescents with cancer compared to healthy adolescents. Pediatr Blood Cancer 2013;60:1902-7. [PubMed]
- Schroevers M, Kraaij V, Garnefski N. How do cancer patients manage unattainable personal goals and regulate their emotions? Br J Health Psychol 2008;13:551-62. [PubMed]
- Schroevers MJ, Kraaij V, Garnefski N. Cancer patients’ experience of positive and negative changes due to the illness: relationships with psychological well-being, coping, and goal reengagement. Psychooncology 2011;20:165-72. [PubMed]
- Kraaij V, Garnefski N, Jan de Wilde E, et al. Negative life events and depressive symptoms in late adolescence: bonding and cognitive coping as vulnerability factors? J Youth Adolesc 2003;32:185-93.
- Coyne JC, Racioppo MW. Never the twain shall meet? Closing the gap between coping research and clinical intervention research. Am Psychol 2000;55:655-64. [PubMed]
- Mishel MH. Uncertainty in Illness. Image J Nurs Sch 1988;20:225-32. [PubMed]
- Stuber ML, Kazak AE, Meeske K, et al. Is posttraumatic stress a viable model for understanding responses to childhood cancer? Child Adolesc Psychiatr Clin N Am 1998;7:169-82. [PubMed]
- Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev 2006;26:233-56. [PubMed]
- Jim HS, Jacobsen PB. Posttraumatic stress and posttraumatic growth in cancer survivorship: a review. Cancer J 2008;14:414-9. [PubMed]
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9:455-71. [PubMed]
- Tedeschi RG, Calhoun LG. Trauma and transformation: growing in the aftermath of suffering. Thousand Aks, CA: Sage Publications, 1995.
- Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq 2004;15:1-18.
- Park CL, Edmondson D, Fenster JR, et al. Meaning making and psychological adjustment following cancer: the mediating roles of growth, life meaning, and restored just-world beliefs. J Consult Clin Psychol 2008;76:863-75. [PubMed]
- Zeltzer L, Kellerman J, Eilenberg L, et al. Psychologic effects of illness in adolescence. II. Impact of illness in adolescents-crucial issues and coping styles. J Pediatr 1980;97:132-8. [PubMed]
- Park CL, Zlateva I, Blank TO. Self-identity after cancer: “survivor”, “victim”, “patient”, and “person with cancer”. J Gen Intern Med 2009;24 Suppl 2:S430-5. [PubMed]
- Chan MW, Ho SM, Tedeschi RG, et al. The valence of attentional bias and cancer-related rumination in posttraumatic stress and posttraumatic growth among women with breast cancer. Psychooncology 2011;20:544-52. [PubMed]
- Sharpe L, Curran L. Understanding the process of adjustment to illness. Soc Sci Med 2006;62:1153-66. [PubMed]
- Zebrack BJ. Cancer survivor identity and quality of life. Cancer Pract 2000;8:238-42. [PubMed]
- Conway MA, Pleydell-Pearce CW. The construction of autobiographical memories in the self-memory system. Psychol Rev 2000;107:261-88. [PubMed]
- Williams JM, Barnhofer T, Crane C, et al. Autobiographical memory specificity and emotional disorder. Psychol Bull 2007;133:122-48. [PubMed]
- Raes F, Hermans D, Williams JM, et al. Reduced specificity of autobiographical memory: A mediator between rumination and ineffective social problem-solving in major depression? J Affect Disord 2005;87:331-5. [PubMed]
- D’Zurilla TJ, Nezu A. A study of the generation-of-alternatives process in social problem solving. Cognit Ther Res 1980;4:67-72.
- Williams JM, Ellis NC, Tyers C, et al. The specificity of autobiographical memory and imageability of the future. Mem Cognit 1996;24:116-25. [PubMed]
- Watkins E, Teasdale JD. Adaptive and maladaptive self-focus in depression. J Affect Disord 2004;82:1-8. [PubMed]
- Watkins E, Teasdale JD. Rumination and overgeneral memory in depression: effects of self-focus and analytic thinking. J Abnorm Psychol 2001;110:353-7. [PubMed]
- Maccallum F, Bryant RA. Imagining the future in complicated grief. Depress Anxiety 2011;28:658-65. [PubMed]
- Maccallum F, Bryant RA. Social problem solving in complicated grief. Br J Clin Psychol 2010;49:577-90. [PubMed]
- Maccallum F, Bryant RA. Impaired autobiographical memory in complicated grief. Behav Res Ther 2010;48:328-34. [PubMed]
- Sutherland K, Bryant RA. Social problem solving and autobiographical memory in posttraumatic stress disorder. Behav Res Ther 2008;46:154-61. [PubMed]
- Sutherland K, Bryant RA. Autobiographical memory in posttraumatic stress disorder before and after treatment. Behav Res Ther 2007;45:2915-23. [PubMed]
- Raes F, Watkins ER, Williams JM, et al. Non-ruminative processing reduces overgeneral autobiographical memory retrieval in students. Behav Res Ther 2008;46:748-56. [PubMed]
- Lee-Jones C, Humphris G, Dixon R, et al. Fear of cancer recurrence--a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology 1997;6:95-105. [PubMed]
- Simard S, Savard J, Ivers H. Fear of cancer recurrence: specific profiles and nature of intrusive thoughts. J Cancer Surviv 2010;4:361-71. [PubMed]
- Platt JJ, Spivack G. Manual for the means-ends problem solving procedure (MEPS): a measure of interpersonal problem solving skill. Philadelphia: Hahnemann Medical College and Hospital, 1975.
- Ferguson E. A taxometric analysis of health anxiety. Psychol Med 2009;39:277-85. [PubMed]
- Portnoy DB. Waiting is the hardest part: anticipating medical test results affects processing and recall of important information. Soc Sci Med 2010;71:421-8. [PubMed]
- Schüz N, Schüz B, Eid M. When risk communication backfires: randomized controlled trial on self-affirmation and reactance to personalized risk feedback in high-risk individuals. Health Psychol 2013;32:561-70. [PubMed]
- Arndt J, Cook A, Goldenberg JL, et al. Cancer and the threat of death: the cognitive dynamics of death-thought suppression and its impact on behavioral health intentions. J Pers Soc Psychol 2007;92:12-29. [PubMed]
- Aubin S, Bingen K, Carpentier MY, et al. Challenges conducting qualitative psychosocial research for adolescent and young adult patients and survivors. J Adolesc Young Adult Oncol 2011;1:71-6.
- Janoff-Bulman R. Shattered assumptions: toward a new psychology of trauma. New York: Free Press, 1992.
- Naus MJ, Ishler MD, Parrott CE, et al. Cancer survivor adaptation model: conceptualizing cancer as a chronic illness. J Clin Psychol 2009;65:1350-9. [PubMed]
- Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer. A conceptual and empirical review. Clin Psychol Rev 2002;22:499-524. [PubMed]
- McLean KC. Late adolescent identity development: narrative meaning making and memory telling. Dev Psychol 2005;41:683-91. [PubMed]
- Bluck S, Alea N, Habermas T, et al. A tale of three functions: the self-reported uses of autobiographical memory. Social Cognition 2005;23:91-117.
- Habermas T, Bluck S. Getting a life: the emergence of the life story in adolescence. Psychol Bull 2000;126:748-69. [PubMed]
- Massey EK, Gebhardt WA, Garnefski N. Self-generated goals and goal process appraisals: relationships with sociodemographic factors and well-being. J Adolesc 2009;32:501-18. [PubMed]
- Kazak AE. Evidence-based interventions for survivors of childhood cancer and their families. J Pediatr Psychol 2005;30:29-39. [PubMed]
- Ferrari A, Thomas D, Franklin AR, et al. Starting an adolescent and young adult program: some success stories and some obstacles to overcome. J Clin Oncol 2010;28:4850-7. [PubMed]


