Evaluation and management of lower back pain in young athletes
Introduction
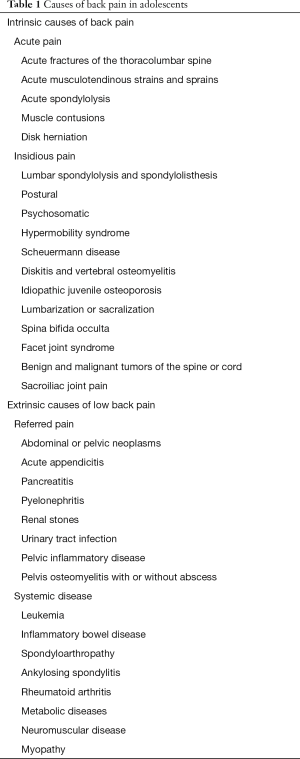
A recent increase in the intensity and volume of physical conditioning exercises or sports participation is the most common predisposing factor for low back pain. A number of causes should be considered in the differential diagnosis of lower back pain in young athletes (Table 1) (1-7). Sports with a relatively higher incidence of low back pain are listed in Table 2 (8-12). It is useful to understand the normal biomechanics of spine movements (2,5,11). During flexion of the thoracolumbar spine there is increased pressure on the intervertebral disks. This increases the tension on the nerve root and the dural sac, and the relative size of the intervertebral canal and foramen. On the other hand, during extension of the thoracolumbar spine, the effects are opposite; there is a decreased tension on the nerve root and dural sac, and the relative size of the intervertebral canal and foramen. Different sports impart different types of biomechanical stresses to the spine. For example, there is compression of the spine in vertical plane in American football and weight lifting; rotational (torque) or shear force in horizontal plane in throwing sports, golf and baseball; and tensile stress from repetitive motion in gymnastics, ballet and cheerleading. Hyperextension of the lumbar spine in American football and gymnastics has been associated with spondylolysis. Incidence is higher with higher levels of competition and floor exercises, the balance beam, uneven parallel bars, flips, and vaulting dismounts are associated with spondylolysis in gymnasts. In throwing sports, such as pitching in baseball, musculotendinous avulsions may occur from sudden and forceful muscle contractions.
Full table

Full table
Lifting with spine in flexion, and moving from flexion to extension causes significant stress to the spine. Improper lifting techniques may cause injuries in ballet and figure skating. Twisting motions in tennis can cause musculotendinous strains and avulsions. Chronic poor posture may result in chronic ligamentous strain.
Clinical presentation
History should include the mechanism of injury and detailed history characterizing the pain. Pain should be characterized by onset, location, duration, progression, exacerbating factors and relieving factors. Is there night pain? Is there radiation of pain in legs? Ascertain past history of back pain or injury. Has the athlete sought any previous medical care?
Athlete will present with a history of back pain following acute trauma or activity related chronic or recurrent pain. Back pain in a young child must be thoroughly investigated for specific etiology that may include infection, tumors or developmental anomalies of the spine.
Localization of pain may indicate possible etiology. Scheuermann disease is the most common identifiable cause of thoracic back pain (13). Spondylolysis most commonly affects the lower lumbar spine (11). Constitutional symptoms such a fever, rash, other joint pain, loss of appetite and weight loss suggest systemic disease. Family history and psychosocial history are essential in all adolescents to assess psychosomatic pain syndrome which is common in this age group. Although neurological injuries are rare, it is important to recognize symptoms and signs that indicate neurological injury that should prompt appropriate imaging and referral for definitive diagnosis and treatment.
General physical examination should focus on detecting signs that indicate systemic etiology. Sexual maturity rating or Tanner stage should be assessed and both lower extremities should be carefully examined. A systematic examination of the back and thoracolumbar spine as well as neurological exam should be conducted in all athletes with back injuries and pain.
AP, lateral and oblique X-rays of the spine are the initial study of choice to assess back thoracolumbar spine injuries and pain (5,9,11). Other imaging studies such as bone scan; computed tomography (CT) scan or magnetic resonance imaging (MRI) scan may be indicated in the evaluation of specific conditions. The most useful screening laboratory studies are a complete blood count and erythrocyte sedimentation rate.
Management
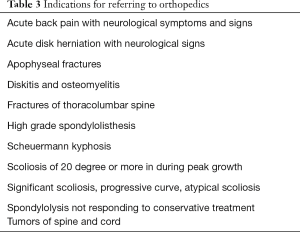
Management of the athlete with thoracolumbar back injury and pain depends upon the specific condition. Conservative modalities include rest, pain management, therapeutic exercises, bracing, orthotics, improving biomechanics, improving sport techniques, and appropriate conditioning and training. Most athletes will respond to conservative treatment depending up on the nature of the specific condition causing the back pain; a few will need further orthopedic consultation (Table 3). Some signs and symptoms are of particular concern and include the following: back pain in a child younger than 10 years of age, pain that wakes up the patient from sleep, pain that lasts more than 2 months, rapidly progressive pain, continuous pain, pain at rest, pain associated with focal neurological findings, and pain associated with systemic symptoms and signs (3,6,7,11).
Full table
Acute soft tissue sprains, strains, and muscle contusions
Acute soft tissue trauma is the most common back injury and cause of back pain in adolescent athletes. The athlete with acute back strain or sprain, who is otherwise in good health, should expect full recovery within few days. Absolute bed rest is not recommended. The athlete should be allowed to carry on daily activities as tolerated. Analgesics and muscle relaxants may help relieve pain during the acute phase. As the pain and general mobility improve, a back rehabilitation exercise program is started in consultation with a sports physical therapist. The goals of rehabilitation for acute back strains and sprains are to regain normal pain-free range of motion, improve core strength and stability, correct abnormal posture, improve biomechanics, and improve sport techniques.
Thoracic Scheuermann disease (Juvenile disk disease)
Scheuermann disease, seen in adolescents, is characterized by fixed kyphotic deformity of the spine. The normal range of thoracic spine curve in sagittal plane is between 20 and 40 degrees and a kyphotic deformity exceeding 45 degrees is considered abnormal (13-15). Males are affected more often than females and most cases are seen between ages 10 and 15 years (13). Most have a positive family history of kyphosis. The reported incidence ranges between 0.4% and 10% during adolescence (13-15). No studies have reported specific incidence or prevalence in athletes. Scheuermann disease is the most common identified cause of thoracic back pain in adolescents. The exact etiology is not known. Postulated contributing factors include genetic predisposition, hormonal abnormalities, collagen defects, juvenile osteoporosis, vitamin deficiencies and repetitive microtrauma from sport participation or other physical stress to the spine (13-15).
Clinical presentation
Many adolescents initially remain asymptomatic and may first present with poor posture and kyphotic deformity. However most present with dull aching thoracic back pain located between scapulae that is aggravated by physical activity, prolonged sitting, standing and forward flexion (13). Pain tends to diminish as the adolescent approaches skeletal maturity. The severity of pain and progressive worsening of the kyphosis have poor correlation.
Many adolescents in the early stage may only have back pain for several weeks to months before progressive kyphosis develops; therefore, Scheuermann disease should be considered in any adolescent who presents with chronic or recurrent thoracic back pain. Occasionally the pain is of sudden onset. The kyphosis should be differentiated from adolescent postural round back that disappears when the athlete hyperextends the back while prone. Patients also have decreased flexibility of hamstrings and exacerbated lumbar lordosis.
Diagnostic imaging
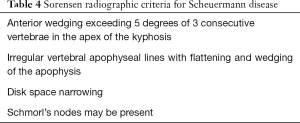
X-ray findings include vertebral end plate irregularities, narrowing of the intervertebral disk space, anterior wedging and decreased height of the vertebrae, and Schmorl nodes (protrusion of nucleus pulposus into the vertebral body anteriorly) (13). Sorenson’s radiographic criteria are listed in Table 4. The diagnostic wedging is not seen before 10 years of age (14). In the classic presentation the apex of the kyphotic deformity is at T7–T8 level (13).
Full table
Treatment
Therapeutic exercises to improve flexibility (especially of hamstrings and lumbodorsal muscles and fascia) and core strength are recommended for all patients (15). Pain can be managed as needed by use of analgesics. More definitive treatment is guided by the severity of the deformity and the remaining growth potential of the patient based on skeletal maturity. Patients with kyphosis less than 50 degrees can be managed conservatively with rehabilitation exercises and regular clinical and radiographic monitoring until they reach skeletal maturity (13-15). Orthopedic consultation should be obtained in all cases of Scheuermann disease. Adolescents who are skeletally immature and have kyphosis that exceeds 50 degrees, bracing is considered (13-15). Curves that exceed 70 degrees, severe persistent pain, and progression of the curve are indications for considering surgical treatment (13-15).
Athletes with curves less than 50 degrees who have undergone rehabilitation and are asymptomatic may return to sports without restrictions (13-15). Athletes being treated with bracing may be allowed to participate in sports, with brace removed for the duration of game or practice, once they have started the rehabilitation and are pain free. Recurrent, activity related back pain and restriction of some back extension are long term problems seen in some patients; however, overall functional outcome has been reported to be very good.
Thoracolumbar (atypical) Scheurmann disease
Thoracolumbar Scheuermann disease is seen in adolescents who participate in sports that require repeated flexion and extension movements such as gymnastics (15). It has also been reported in adolescents who participate in wrestling, football, weight lifting, rowing, tennis, and bicycle racing. It is seen most commonly in male athletes with a peak incidence between 15 and 17 years of age (13).
Because of wedging of the vertebrae at the thoracolumbar spine there is a loss of lumbar lordosis and the back appears straight or mildly kyphotic. Other clinical features are similar to the thoracic type. Thoracolumbar Scheuermann disease generally is nonprogressive and treated with exercise and conditioning program and restriction of sport until the athlete is pain free. Most athletes are able to return to sports after a period of about 6 months of conservative treatment. Bracing for a period anywhere from 3 to 12 months has also been used allowing athletes to return to sports within 2–3 months once pain free (13).
Adolescent idiopathic scoliosis
Scoliosis is defined as a lateral curvature of the spine greater than 10 degrees as measured by using the Cobb method on a standing posteroanterior radiograph of the spine (16). Vertebral rotation is associated with the lateral curvature. In Cobb method, a line is drawn through the superior surface of the uppermost vertebra of the curve. Another is drawn through the inferior surface of the lowermost vertebra of the curve. The angle at the intersection of lines drawn perpendicular to the above two lines is the Cobb angle or the curvature of the scoliosis. The reported prevalence of adolescent scoliosis is between 0.5% and 3% (16-21).
The exact mechanism or etiology of adolescent scoliosis is not known but believed to be multifactorial with strong genetic predisposition (21-24). During adolescent years, curve progression occurs in about 10% of cases of adolescent idiopathic scoliosis (25). Curve progression is a function of gender, remaining skeletal maturity at the time of diagnosis, and the magnitude of the curve at the time of diagnosis (25,26).
Clinical presentation
Adolescent idiopathic scoliosis can be asymptomatic. Pain and deformity may become apparent with larger curves and with progression of the curve (16). Spine should be examined at all preventive visits during adolescent years, typically once a year. Measure leg length (from anterior superior iliac spine to medial malleolus) to rule out leg length inequality. Have the standing patient bend forward as far as he or she can, with both upper extremities extended and palms held together hanging down. Observe from the front of the patient for a thoracic hump on one side indicating scoliosis. This is called Adam’s test (Figure 1). Also observe the spine from side to note any kyphosis. Determine the sexual maturity rating of the patient. Some studies have shown that overweight and obese children and adolescents are more likely to initially present with more severe curve and at a higher degree of skeletal maturity at the time of the presentation (16).

Diagnostic imaging
A scoliosis series is indicated to assess the degree of scoliosis as measured by Cobb angle. Periodic radiographic evaluation is indicated based on the initial degree and risk of progression of the scoliosis.
Treatment
Adolescents with idiopathic scoliosis at sexual maturity rating of 2 with curves more than 20 degrees should be referred to pediatric orthopedic or spine specialist (21). Those whose curves are less than 20 degrees, and are less likely to progress as determined by gender and remaining skeletal maturity can be followed every 6 months with clinical and radiologic evaluation to assess the curve (24,25). Exercise programs are not effective in altering the progression of the curve.
Several studies have shown effectiveness of bracing if done appropriately and when the patient is adherent to the treatment protocol (17-20). Surgery is considered in rapidly progressive curves, and curves more than 45 degrees (22).
Asymptomatic athletes are allowed unrestricted sport participation. Participation decision should be individualized in consultation with orthopedic or spine surgeon for those with painful high degree curves, those being treated with bracing, and those who had surgical correction.
Lumbar spondylolysis
Spondylolysis refers to stress fracture of the pars interarticularis (isthmic type), most lesions are bilateral (80%) and affect L5 (95%) (27-29). It is one of the most common and significant conditions that causes back pain in adolescent athletes, reported in almost 50% of cases of sport related low back pain in adolescents (30,31). The incidence of spondylolysis is 6% in the general population compared with 50% in gymnasts, 40% in Alaskans and 13% in Eskimos (30-33). A higher incidence is seen in ballet, gymnastics, competitive cheerleaders, American football linemen, weight lifting, wrestling, diving, volleyball, and fast bowlers in cricket (32,33). The mean age at diagnosis in athletes is around 15–16 years, but can occur at earlier age. Repetitive axial loading and rotation, especially in an extended lumbar spine, is the most important contributing mechanism leading to fatigue fracture of the pars interarticularis (33-35).
Clinical presentation
Many athletes with spondylolysis are asymptomatic and may or may not progress to symptomatic lesions. Athletes with symptomatic spondylolysis generally present with insidious onset, recurrent, activity associated, low back pain (31). Athlete may also present with a history of sudden onset of pain with acute spondylolysis as reported in competitive cheerleading and gymnastics. The pain is localized to low back, non-radiating, and dull aching to sharp. Pain is also reported in buttocks and back of the thigh. Patients do not have any neurological symptoms or signs.
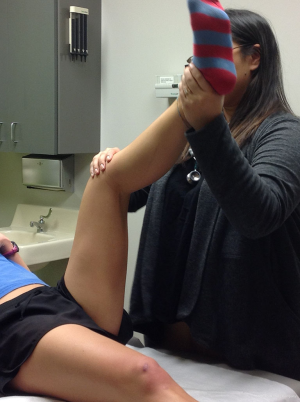
Decreased flexibility of the hamstrings (Figure 2) and lumbodorsal muscles and fascia is seen in almost all symptomatic athletes and may be the only and/or initial presenting sign. Increased lumbar lordosis and a relative weakness of abdominal muscles are also common findings. Lower back pain can be reproduced or exacerbated by one-leg hyperextension movement of the lumbo-sacral spine (Figure 3).

Diagnostic imaging
There is no universally accepted consensus for imaging protocol, and the decision to proceed with any particular imaging study and its timing should be determined on an individual basis based on the findings on clinical evaluation and particular circumstances of the athlete.
Plain films are initial study of choice and should include anteroposterior, lateral, and oblique views of the lumbosacral spine. In a typical lesion the characteristic pars defect is most evident on the oblique view, and described as the scotty dog with a collar appearance (32). Like other stress fractures, X-rays may not be positive until after 1–2 weeks. Plain films are useful to detect any associated anomalies such as spina bifida occulta and other congenital vertebral anomalies, as well as spondylolisthesis.
The need for and appropriateness of additional imaging studies should be ideally considered in consultation with the radiologist locally. A bone scan or a single photon emission computed tomography (SPECT) scan are highly sensitive in the diagnosis if the plain films are normal, and to determine the acuity of the fracture; and a CT scan is useful to delineate the defect. The bone scan and SPECT scan require injection of radiographic dye, and radiation exposure which is also a consideration for CT scan. Increasingly, magnetic imaging resonance scan is being used as a next step in cases where initial X-rays are negative. MRI scan is useful in detecting early or acute lesions, delineating the anatomic nature of the pars defect, and detect any spinal or soft tissue pathology (32).
Treatment
Most athletes with spondylolysis can be managed conservatively. Symptomatic athletes should refrain from sports and hyperextension activities until pain free, which may take a few days to several weeks (30-35). Athletes should work with knowledgeable sports physical therapist or athletic trainer for rehabilitation program focused on core stabilization, strengthening, and flexibility exercises. Return to sport is allowed once the athlete is pain free, has normal examination, and has undergone rehabilitation. Failure of conservative treatment and recurrent or persistent pain is an indication for orthopedic consultation.
Spondylolisthesis
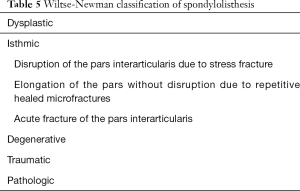
Spondylolisthesis is characterized by forward slippage of a vertebra over the one just below it, most commonly of L5 over S1 (30). Spondylolisthesis is a common complication of bilateral spondylolytic lesions. Wiltse-Newman classification of types of spondylolisthesis is described in Table 5 (30). Isthmic type is the most common type seen in adolescent athletes. The overall incidence and epidemiologic characteristics are similar to those of spondylolysis. The basic mechanism is similar to that of spondylolysis, and generally occurs as a complication of bilateral spondylolytic defects at the same vertebral level.
Full table
Clinical presentation
Athlete presents with gradual onset, aching pain in the lower back, buttocks or the posterior thigh. The pain is aggravated with physical activities, especially those involving repeated flexion, extension, and rotation. In some cases, spondylolisthesis is asymptomatic. Patient often assumes characteristic posture while standing or walking with increased hip and knee flexion or crouched posture (known as the Phalen-Dickson sign) (30). On examination there is hamstring tightness (80% of patients), and exacerbated lumbar lordosis and a step-off over the lumbar spine may be palpated (30,31). Lumbar radicular symptoms are rare, and may be present in high grade spondylolisthesis. Lower limb strength, sensation, and reflexes should be tested.
Diagnostic imaging
Lateral X-ray of the lumbosacral spine is sufficient in most cases to diagnose and assess the degree of slippage. Meyerding classification of the degree of slippage is as follows: grade 1—less than 25%; grade 2—26–50%; grade 3—51–75%; and grade 4—75–99% (30-32). MRI scan is indicated if the patient has neurological symptoms or signs to evaluate for other causes such as disk herniation in conjunction with spondylolisthesis.
Treatment
The risk for progression is higher for younger athletes and they should be followed regularly until skeletal maturity. Initial treatment of patients with low grade (grade I and II) spondylolisthesis without neurological signs is similar to that of patients with symptomatic acute spondylolysis that includes restriction of sports until asymptomatic, physical therapy, and bracing (30). All patients with high grade lesions and those with neurological signs should be referred to orthopedic surgeon for definitive further evaluation and treatment that includes different surgical options.
Disk herniation
Herniation of the intervertebral disk into the spinal canal is rare in children and adolescents with a reported incidence of between 0.8% and 3.2% (36-39). The incidence is generally equal between males and females. Most commonly affected levels are L4–L5 and L5–S1 (36). Weight lifting, gymnastics, wrestling and collision sports are high risk sports for disk herniation (36).
Disk herniation can result either from acute or repetitive trauma. In skeletally immature adolescents, compression force during forward flexion can result in disk herniation and may involve herniation of the disk vertically through the end plate. In many adolescents with disk herniation, other congenital spine anomalies are found such as spina bifida occulta, transitional vertebra or congenital spinal stenosis (36).
Clinical presentation
Athlete may present with a history of sudden onset pain related to a particular activity or insidious onset, intermittent activity related pain of several weeks or months duration. A clear history of acute trauma is elicited in only 40–50% of the patients (36,37). The most common presenting symptoms are back and leg pain and stiffness that are exacerbated with activity. The pain may or may not radiate to legs and generally neurological signs are absent in most children and adolescents (36-38). Pain is also exacerbated by coughing, sneezing or sitting. In some athletes, lumbar radicular signs may be elicited. Most have limitation of lumbosacral spine movement and mild scoliosis may be detected in some patients. Positive straight leg raise sign is the most common finding present in almost all patients. Listing toward the side of herniation may also be present. Hamstring tightness is common and early sign of disk herniation.
Diagnostic imaging
MRI is the study of choice to detect disk herniation and any neurological compromise. Positive MRI scan findings must be correlated with clinical findings because many individuals have abnormalities on MRI scan that are of no clinical significance.
Treatment
In the absence of neurological signs, the initial treatment is conservative with relative rest, restriction from sports and initiating physical therapy. Most adolescents respond well to conservative treatment over a period of several weeks, typically 6–12 weeks. Failure of clinical improvement with conservative treatment and presence of any neurological signs (initially or later) are indications for surgical consultation for definitive treatment. Studies show a more favorable outcome in adolescents following surgical treatment (37,38). Prognosis in young athletes is excellent for return to full sport participation following appropriate treatment.
Slipped vertebral apophysis (fracture of ring apophysis)
A fracture through the weak osteocartilaginous junction between the vertebral body and its apophysis results in displacement and protrusion into the spinal canal of the fractured segment along with the associated intervertebral disk (40). This injury is unique to adolescents, more common in males, and most commonly involves the inferior apophysis of L4 (40). Most cases are reported in wrestling and gymnastics. Apophyseal fractures and displacement can result from either acute or repetitive trauma from compressive loads applied to the spine during flexion.
Clinical presentation
In general, symptoms and signs are similar to that of acute central disk herniation. The athlete typically presents with acute lumbar pain with onset during activity usually weight lifting or other sports that require hyperflexion of lumbar spine (40). Pain may be described as burning and radiate into the leg. The pain is exacerbated by sitting, coughing and sneezing. Pain is also elicited by contralateral straight leg raise. Because of posterior central protrusion, lumbar radicular signs may be elicited on examination; however, neurological findings are uncommon in most adolescents and that may delay diagnosis (40).
Diagnostic imaging
AP and lateral X-rays of the lumbar spine may or may not show the bony avulsion. A CT scan and/ or MRI scan may be indicated to further delineate the injury.
Treatment
Athletes should be restricted from sports and referred to orthopedics for definitive treatment. Most consider surgical excision of the fractured fragment as the treatment of choice.
Fractures of the thoracolumbar spine
Acute fractures of the thoracolumbar spine are uncommon in youth sports; most are due to motor vehicle accidents, falls or abuse in the very young child and about 25% may be associated with neurological injury (1-3). Fractures of the thoracolumbar spine have been reported in adolescents participating in collision sports such as American football, ice hockey, and rugby. Most are seen in adolescents more than 16 years of age in whom the fracture characteristics are similar to those seen in adults. The most frequently injured area is from T4 to T12 (1,2,5). Spinal cord injury without a bony fracture (spinal cord injury without radiographic abnormality), most affecting the cervical spine, is a unique injury seen mostly in very young children whereas vertebral apophyseal and endplate injuries are unique to adolescents (1-7).
The key mechanisms for spine fractures include (I) sudden hyperflexion of the spine with or without vertebral body compression; (II) distraction of the spine; and (III) shearing force (1-7). Axial loading or compression of the flexed or straight spine can cause a vertebral body compression or a burst fracture seen in sports. Fracture of the apophysis of the spinous process, mostly of the thoracic spine, can result from sudden distraction force.
The athlete typically is injured in a collision sport and presents with a history of acute onset back pain with or without neurological findings. Most will present on the field or in the emergency department following the injury and should be further evaluated and treated by physicians with expertise in the management of spinal trauma.
Pediatric athletes with acute traumatic spine fractures should be referred to orthopedic surgeon for further evaluation and definitive management with long term follow up.
SI joint pain
SIJ is a diarthrodial joint with minimal movements in transverse or longitudinal planes not exceeding 2–3 degrees (41). The prevalence of low back pain directly related to SIJ in young athletes is not known. SIJ pain has been reported in most commonly in rowing and cross country skiing. Pain may be in the lower back, buttocks, back of thighs or pelvis. Tenderness may be localized over the SIJ and pain may be elicited or exacerbated with some provocative tests such as flexion-abduction-external rotation (FABER) of the hip and Gaenslen (Figure 4). The diagnosis is mainly based on history and examination findings. Imaging studies may be indicated to exclude other causes of pain. Chronic SIJ pain may be difficult to treat. In addition to relative rest, modification of activities, and use of non-steroidal anti-inflammatory drugs (NSAIDs), various other treatment modalities have been reported with variable success in individual cases (41-45). These include manual or manipulative treatment, prolotherapy, intraarticular injections of local anesthetics and corticosteroids, and radiofrequency neurotomy (41-45). Athletes with significant chronic pain should be referred to experts with experience in treating SIJ pain and dysfunction.

Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Clark P, Letts M. Trauma to the thoracic and lumbar spine in the adolescent. Can J Surg 2001;44:337-45. [PubMed]
- Ferguson RL. Thoracic and lumbar spine trauma of the immature spine. In: Herkowitz HN, Garfin SR, Eismont FJ, et al. editors. Rothman-Simeone The Spine. 5th edition. Philadelphia: Saunders, 2005: 603-12.
- Waicus KM, Smith BW. Back injuries in the pediatric athlete. Curr Sports Med Rep 2002;1:52-8. [Crossref] [PubMed]
- Curtis C, d’Hemecourt P. Diagnosis and management of back pain in adolescents. Adolesc Med State Art Rev 2007;18:140-64. x. [PubMed]
- D’Hemecourt PA, Gerbino PG 2nd, Micheli LJ. Back injuries in the young athlete. Clin Sports Med 2000;19:663-79. [Crossref] [PubMed]
- Richards BS, McCarthy RE, Akbarnia BA. Back pain in childhood and adolescence. Instr Course Lect 1999;48:525-42. [PubMed]
- Karol LA. Back pain in children and adolescents. In: Herkowitz HN, Garfin SR, Eismont FJ, et al. editors. Rothman-Simeone The Spine. 5th edition. Philadelphia: Saunders, 2005: 493-506.
- Jones GT, Macfarlane GJ. Epidemiology of low back pain in children and adolescents. Arch Dis Child 2005;90:312-6. [Crossref] [PubMed]
- Bono CM. Low-back pain in athletes. J Bone Joint Surg Am 2004;86-A:382-96. [Crossref] [PubMed]
- Trainor TJ, Wiesel SW. Epidemiology of back pain in the athlete. Clin Sports Med 2002;21:93-103. [Crossref] [PubMed]
- Herring JA. Back pain. In: Tachdjian’s Pediatric Orthopaedics. 3rd edition. Philadelphia: Saunders Elsevier, 2002: 95-108.
- Dormans JP, Moroz L. Infection and tumors of the spine in children. J Bone Joint Surg Am 2007;89 Suppl 1:79-97. [PubMed]
- Sørensen KH. Scheuermann’s juvenile kyphosis: clinical appearance, radiography, aetiology and prognosis. Copenhagen: Munksgaad, 1964.
- Bezalel T, Carmeli E, Been E, et al. Scheuermann's disease: current diagnosis and treatment approach. J Back Musculoskelet Rehabil 2014;27:383-90. [Crossref] [PubMed]
- Palazzo C, Sailhan F, Revel M. Scheuermann's disease: an update. Joint Bone Spine 2014;81:209-14. [Crossref] [PubMed]
- Goodbody CM, Sankar WN, Flynn JM. Presentation of Adolescent Idiopathic Scoliosis: The Bigger the Kid, the Bigger the Curve. J Pediatr Orthop 2017;37:41-6. [Crossref] [PubMed]
- Sanders JO, Newton PO, Browne RH, et al. Bracing for idiopathic scoliosis: how many patients require treatment to prevent one surgery? J Bone Joint Surg Am 2014;96:649-53. [Crossref] [PubMed]
- Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512-21. [Crossref] [PubMed]
- Wiemann JM, Shah SA, Price CT. Nighttime bracing versus observation for early adolescent idiopathic scoliosis. J Pediatr Orthop 2014;34:603-6. [PubMed]
- Schwieger T, Campo S, Weinstein SL, et al. Body Image and Quality-of-Life in Untreated Versus Brace-Treated Females With Adolescent Idiopathic Scoliosis. Spine (Phila Pa 1976) 2016;41:311-9. [Crossref] [PubMed]
- Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect 2005;54:529-36. [PubMed]
- Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976) 2007;32:S91-S100. [Crossref] [PubMed]
- Rowe DE, Bernstein SM, Riddick MF, et al. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am 1997;79:664-74. [Crossref] [PubMed]
- Charles YP, Daures JP, de Rosa V, et al. Progression risk of idiopathic juvenile scoliosis during pubertal growth. Spine (Phila Pa 1976) 2006;31:1933-42. [Crossref] [PubMed]
- Sanders JO, Browne RH, McConnell SJ, et al. Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am 2007;89:64-73. [PubMed]
- Perdriolle R, Vidal J. Thoracic idiopathic scoliosis curve evolution and prognosis. Spine (Phila Pa 1976) 1985;10:785-91. [Crossref] [PubMed]
- Oren JH, Gallina JM. Pars Injuries in Athletes. Bull Hosp Jt Dis (2013) 2016;74:73-81. [PubMed]
- Violas P, Lucas G. L5S1 spondylolisthesis in children and adolescents. Orthop Traumatol Surg Res 2016;102:S141-7. [Crossref] [PubMed]
- Scheepers MS, Streak Gomersall J, Munn Z. The effectiveness of surgical versus conservative treatment for symptomatic unilateral spondylolysis of the lumbar spine in athletes: a systematic review. JBI Database System Rev Implement Rep 2015;13:137-73. [Crossref] [PubMed]
- Mooney JF. Spondylolysis and spondylolisthesis. In: Herkowitz HN, Garfin SR, Eismont FJ, et al. editors. Rothman-Simeone The Spine. 5th edition. Philadelphia: Saunders, 2005: 586-602.
- Cavalier R, Herman MJ, Cheung EV, et al. Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg 2006;14:417-24. [Crossref] [PubMed]
- McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Curr Sports Med Rep 2007;6:62-6. [PubMed]
- Congeni J, McCulloch J, Swanson K. Lumbar spondylolysis. A study of natural progression in athletes. Am J Sports Med 1997;25:248-53. [Crossref] [PubMed]
- Miller SF, Congeni J, Swanson K. Long-term functional and anatomical follow-up of early detected spondylolysis in young athletes. Am J Sports Med 2004;32:928-33. [Crossref] [PubMed]
- Stasinopoulos D. Treatment of spondylolysis with external electrical stimulation in young athletes: a critical literature review. Br J Sports Med 2004;38:352-4. [Crossref] [PubMed]
- Dang L, Chen Z, Liu X, et al. Lumbar Disk Herniation in Children and Adolescents: The Significance of Configurations of the Lumbar Spine. Neurosurgery 2015;77:954-9. [Crossref] [PubMed]
- Lagerbäck T, Elkan P, Möller H, et al. An observational study on the outcome after surgery for lumbar disc herniation in adolescents compared with adults based on the Swedish Spine Register. Spine J 2015;15:1241-7. [Crossref] [PubMed]
- Strömqvist F, Strömqvist B, Jönsson B, et al. Lumbar disc herniation surgery in children: outcome and gender differences. Eur Spine J 2016;25:657-63. [Crossref] [PubMed]
- Wang H, Zhang Z, Zhou Y. Irregular Alteration of Facet Orientation in Lumbar Segments: Possible Role in Pathology of Lumbar Disc Herniation in Adolescents. World Neurosurg 2016;86:321-7. [Crossref] [PubMed]
- Wu X, Ma W, Du H, et al. A review of current treatment of lumbar posterior ring apophysis fracture with lumbar disc herniation. Eur Spine J 2013;22:475-88. [Crossref] [PubMed]
- Rashbaum RF, Ohnmeiss DD, Lindley EM, et al. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg 2016;29:42-8. [PubMed]
- Brolinson PG, Kozar AJ, Cibor G. Sacroiliac joint dysfunction in athletes. Curr Sports Med Rep 2003;2:47-56. [Crossref] [PubMed]
- Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil 2006;85:997-1006. [Crossref] [PubMed]
- Hansen HC, McKenzie-Brown AM, Cohen SP, et al. Sacroiliac joint interventions: a systematic review. Pain Physician 2007;10:165-84. [PubMed]
- Rabago D, Best TM, Beamsley M, et al. A systematic review of prolotherapy for chronic musculoskeletal pain. Clin J Sport Med 2005;15:376-80. [Crossref] [PubMed]


