Cardiac screening to prevent sudden death in young athletes
Introduction
Cardiovascular (CV) screening in young athletes remains a challenging issue and a topic of considerable debate. There is no question that sudden deaths in this population are rare and heartbreaking events that continue to have an impact on communities worldwide. While media coverage of sudden cardiac arrests in young athletes helps raise awareness of the importance of CV screening in young athletes, it has also led the general population to believe that these events occur more frequent than they actually do. The incidence of sudden cardiac death (SCD) on the playing field is 0.61 in 100,000 (1). Although these events are rare, it is still appropriate to ask the question: can these sudden deaths be prevented? To answer this question, it is first important to recognize the causes of SCD in young athletes. In 2016, a study analyzed the demographics and epidemiology of sudden deaths in young athletes using the United States National Registry between 1980 and 2011 (2). Using autopsy reports, 842 athletes were found to have cardiovascular etiologies. Among the 842 athletes, males represented the majority in a 6.5:1 male to female ratio. Of the specific cardiovascular diagnoses, hypertrophic cardiomyopathy (HCM) was the most common cause of SCD, occurring in 302 of 842 athletes (36%) (2). Some of the other leading causes of SCD were identified as congenital coronary artery anomalies, arrhythmogenic right ventricular cardiomyopathy, and clinically diagnosed long QT syndrome. African Americans and other minorities were the most represented (5 times greater than whites) with HCM remaining as the leading cause of SCD in that population (2). Conditions affecting the heart that increase young athletes’ risk for SCD are listed in Table 1.
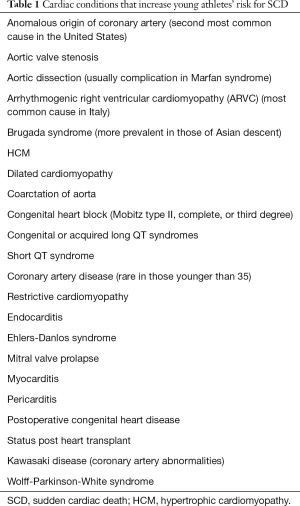
Full table
Considering the common causes of SCD in young athletes, the American Heart Association (AHA) developed a screening tool to help detect and subsequently prevent SCD in young athletes that suffer from congenital or genetic heart disease. Currently, the guidelines do not recommend the use of routine screening electrocardiography (ECG) in the physical evaluation of young athletes, but this remains an issue for debate. In this article we will review normal physiologic adaptations of the athlete’s heart, current recommendations and limitations for screening young athletes for cardiac disease, and discuss whether all young athletes should be screened with routine ECGs.
The athlete’s heart
The cardiovascular system of athletes and the general population is functionally and structurally different due to conditioning based on exercise type. Endurance training includes sports such as long-distance running and swimming, while examples of strength training include wrestling, weightlifting, or throwing heavy objects (3). However, most sports to some extent are a combination of both.
The acute phase response to endurance training includes an increase in oxygen consumption, cardiac output, stroke volume, and systolic blood pressure, associated with decreased peripheral vascular resistance (PVR) (3). The acute response to resistance training, such as lifting weights, includes only marginally increased oxygen consumption and cardiac output but large increases in blood pressure, PVR, and heart rate. Thus long term, endurance exercise primarily produces volume overload induced left ventricular (LV) dilatation, while resistance training produces a pressure overload induced left ventricular hypertrophy (LVH).
Each athlete’s heart responds to cardiovascular conditioning differently. Exercise will induce some sort of evidence of cardiac remodeling in around 50% of all athletes (3). Changes include increased cavity size of both ventricles and the left atrium (3). Endurance athletes may have marked enlargement of the LV chamber and this may be accompanied by a mild increase in absolute LV wall thickness that exceed what is considered normal. Additionally, left atrial remodeling can also be frequently seen in highly trained athletes. Twenty percent of athletes have been found to have increased left atrial dimensions that may be considered benign and often seen with training in endurance sports (3).
Due to the normal physiologic changes of the heart, abnormal ECG patterns can occur in 40% of trained athletes (3). Repolarization patterns, increased QRS voltages, diffuse T-wave inversion, and deep Q waves are most commonly reported (3). In addition, trained athletes are known to commonly manifest innocent arrhythmias and conduction alterations. These include sinus bradyarrhythmia, junctional rhythm, and first-degree or Wenckebach AV block (Mobitz type I) due to increased vagal tone (3). These abnormal but common ECG findings in athletes confuse the clinical picture when screening young athletes for cardiac disease. To date, there has been no evidence to show that the cardiac remodeling in an athlete has a disabling, permanent, or detrimental course.
Current recommendations
In 2014 the AHA released the new 14-element cardiovascular screening checklist for congenital and genetic heart disease in young athletes (Table 2) (4). This checklist is recommended to be performed during all preparticipation physical examinations (PPE). The goal in performing a PPE is to promote the health and safety of the athlete in training and competition. It provides the medical background on which physical activity decisions will be made by the individual athlete’s physician. At the discretion of the examiner, a positive response or finding in any 1 or more of the 14 items may be judged sufficient to trigger a comprehensive cardiovascular evaluation in which ECG, echocardiography or stress testing may be performed.
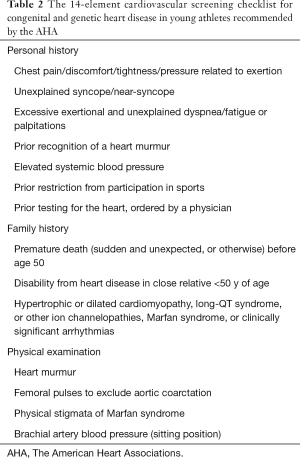
Full table
It is important to stress that routine screening ECG in young athletes is not currently recommended by the AHA. The use of ECGs to detect underlying congenital and genetic heart disease in this group prior to employing this checklist has not been shown to be effective in detecting cardiac conditions that increase the risk for SCD. Although routine ECG is not recommended, it remains a controversial issue due its potential of increasing the number of healthy athletes who screen positive.
The Seattle, Stanford and European Society of Cardiology criteria
Even if a young athlete screens positive with the current AHA 14-element screening criteria, how sensitive and specific are ECGs at diagnosing conditions that warrant further evaluation? An ECG increases the ability to detect underlying cardiac conditions that may increase the risk of SCD but in most countries physicians lack the knowledge in interpreting an athlete’s ECG. It is important for clinicians to distinguish normal physiologic adaptations of the heart in athletes from abnormal findings suggestive of pathology (5). Studies have shown that many physicians cannot accurately interpret and athlete’s ECG. As a result, this leads to an overwhelming rate of false positive interpretations and needless secondary evaluations (5). The creation of the criteria listed above [i.e., European Society of Cardiology (ESC), Stanford, and Seattle] was primarily aimed at decreasing the false positive rate of ECGs read as abnormal in an athlete with a physiologic normal heart.
The ESC was the first group to create such criteria. In 2005, the ESC developed a screening protocol for prevention of SCD in young athletes. It included a history and physical exam along with performing an ECG (6). While the 2005 guidelines listed ECG abnormalities relevant to pre-participation screening, it did not provide guidelines for ECG abnormalities that are commonly seen in an athlete’s heart. In 2010, the ESC modified its guidelines to include normal ECG findings commonly found in an athlete’s heart (6). In the 2010 ESC guidelines an athlete’s ECG findings were classified into two groups, “common and training-related” and “uncommon and training-unrelated.” The aim of the 2010 ESC criteria was to increase the specificity of the preparticipation screening ECG, while maintaining its sensitivity. Using a study population of 508 university athletes, the 2010 ESC criteria was compared to the 2005 criteria by Weiner et al. (7). Echocardiography was performed in all athletes to assess the diagnostic accuracy of the ECG criteria. The study found that the 2010 ESC criteria improved specificity and decreased false positives from 16.3% to 9.6%, while preserving sensitivity compared to the 2005 criteria (7).
In 2011, Stanford University came out with another consensus document that provided specific cut-off values for long QT interval and intra-ventricular conduction delay included in an athlete’s ECG changes (8). In addition, the Stanford criteria recognized that the configuration of anterior T-wave inversion in V1–V4 associated with ST-segment elevation in black athletes was common in an athlete’s heart (8). In 2013, the ECG criteria was further revised and detailed descriptions of ECG limits with reference values for abnormality and what warranted further evaluation were provided by the Seattle criteria (5). Table 3 lists abnormal ECG findings as defined by the Seattle criteria, while Table 4 demonstrates normal ECG findings in athletes.
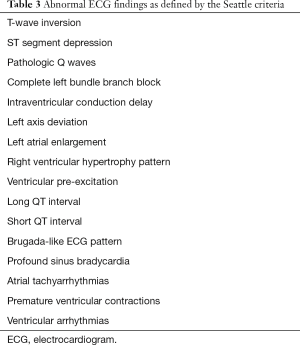
Full table
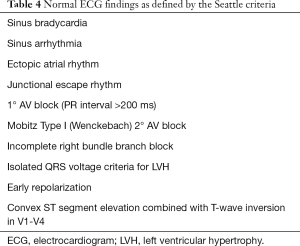
Full table
The specificity of the 2010 ESC, 2011 Stanford and 2013 Seattle criteria was compared in a population of 1417 healthy American athletes (9). This study concluded that the rate of false positive ECG abnormalities requiring further work-up and assessment significantly decreased when the Stanford (8%) and Seattle (6%) criteria were applied compared to the ESC (26%) criteria. The improved specificity of the Seattle and Stanford criteria was thought to be attributed to more definitive definitions of QT intervals and non-specific intraventricular conduction delay (9). Other studies have shown similar results in that the use of the Seattle criteria, when compared to ESC criteria, significantly decreased the number of false positive results while maintaining sensitivity (10-12).
The limitations of current AHA guidelines
Subsequent to the adoption of the AHA 14-element cardiovascular screening checklist for young athletes without the use of routine screening ECG, researchers have analyzed whether or not this is enough to prevent SCD in athletes. Since the AHA 14-element checklist is relatively new, researchers from Stanford University examined the prevalence of athletes who screened positive with the preparticipation examination guidelines from the previous AHA 12-element checklist in combination with screening ECGs (13). This study involved a total of 1,596 participants that included high school, collegiate, and professional athletes. Of the 1,596 participants, 25% of all athletes had responded “yes’ to at least one of the components of the AHA 14-element checklist (13). Of all the athletes who were screened with an ECG, 6% were found to have an abnormal ECG using the Seattle criteria, 8% percent using the Stanford criteria, and 26% using the ESC criteria (13). Only 22 athletes (1.4%) had both an abnormal ECG based on Seattle criteria and at least one positive response to an AHA checklist item, in comparison to 38 athletes (2.4%) using the Stanford criteria and 98 athletes (6.1%) based on ESC criteria (13). Only a small percentage of the population in this study were reported to have an abnormal ECG that triggered further workup including echocardiography, exercise stress test or cardiac magnetic resonance imaging (MRI). However, of the 1,596 athletes, no athlete was found to have a clinical condition excluding them from sports participation. From this study we can conclude that the 12-element screening checklist created in 2007 led to an increased number of athletes with false positive results. It is still undetermined whether the 14-element checklist, which replaced the 12-element checklist in 2014, has better sensitivity and specificity for screening. It is unlikely that the addition of two questions (having had been restricted from sports prior, and prior testing of the heart) will raise the screening tool’s ability to limit the excessive number of false positives.
Not only do the current guidelines lead to increased false positive results and unnecessary testing, lack of standardization is a major limitation to screening practices. Successful detection of athletes at risk of SCD requires a detailed personal and family history taken by a knowledgeable physician who is competent at performing a cardiovascular focused physical examination. Although the screening questions in the current AHA 14-element checklist may serve as a flag for further questioning, what is deemed a positive response may vary amongst providers. One study demonstrated a positive response in 68% of young athletes screened (14). After review by a physician over half of these responses were thought not to be relevant and were disregarded. Still, 31% of this population screened went on for further testing and none were found to have a cardiac pathology (14). To make the matter more complicated, recent findings from the US suggest that 35% of the states allow nonphysician examiners with inadequate training in cardiovascular evaluation to perform the PPE (15). There will continue to be a discrepancy in the determination of positive responses due to differences in athletic populations, manner in which the question is asked and understood, and the extent and quality of history and physical examination performed by the physician.
Another significant challenge to screening with current AHA guidelines is that in up to 80% of cases, SCD is the presenting symptom in cardiovascular pathology (16). Therefore, how can these patients screen positive for symptoms with current AHA guidelines if the majority of patients remain asymptomatic until they collapse on the field? Screening for symptoms that these patients most likely do not have by history will miss the overwhelming majority of cases. The 20% of athletes who do have warning signs before SCD may have non-specific symptoms making screening by history alone challenging (17). Most recently, a systematic review and meta-analysis was done reviewing the effectiveness of the screening history and physical exam with current AHA guidelines (14). Researchers pooled all data to determine the sensitivity and specificity of history and physical exam alone. Meta-analysis determined that the history taken had a sensitivity of 20% and a specificity of 94%; while the sensitivity for the physical examination was 9% and the specificity was 97% (14). These findings suggest that history and physical exam used alone as part of the PPE is not a good screening test to detect athletes at risk of SCD.
Should advanced screening technology be included for young athletes?
The use of routine ECG screening in the pre-participation sports physicals has been a topic of contention over the last decade or so. Various studies have been carried out to determine the use of ECGs; however, the findings show mixed results. One of the main reasons for differences in findings in different studies is the fact that studies done in different countries and different populations may not be comparable in terms of cardiac disease epidemiology in young athletes and population in general. Multiple factors, including genetics, environmental, cultural and dietary, affect cardiac disease epidemiology in different parts of the world.
Currently, the American Medical Association (AMA) and AHA guidelines do not recommend screening ECGs. While the AMA/AHA guidelines do not endorse routine ECGs, many countries and organizations such as Japan, Italy, The Fédération Internationale de Football Association (FIFA) and the International Olympic Committee do recommend screening.
An often referenced study carried out in Italy concluded that a significant decrease (90%) in SCD was noted by identifying athletes with cardiomyopathy with the use of screening ECGs and history and physical examination (H&P) (18). A study done at the Children’s Hospital of Philadelphia found that an ECG screening was three-fold more likely to detect abnormalities leading to SCD when compared to history and physical examination alone, with a reported specificity of 93% and a false-positive rate of 7.8 (19). They also included the use of echocardiography in their study and it was found that echocardiography had a specificity of 100% (19).
The use of echocardiography as a screening test is controversial. Routine use of echocardiography is expensive. Echocardiography is not the best modality to detect patients with arrhythmogenic abnormalities such as ion channelopathies and Wolf-Parkinson-White syndrome that lead to SCD. On the other hand echocardiography is more useful in detecting HCM and coronary artery anomalies, which are the most common causes of SCD in the United States. The Early Screening for Cardiac Abnormalities with Pre-participation Echocardiography (ESCAPE) protocol was developed by Northeastern University (20). The study involved the use of portable echocardiography by a frontline physician (PEFP) to directly visualize specific anatomical structures of the heart that are involved in SCD in specific echo windows with specific measurements taken. Sixty-five Division 1 athletes were screened based on H&P (2007 AHA 12-element screen), an ECG (2010 ESC criteria), and limited portable echo performed by a sports medicine physician (non-cardiologist) to assess for HCM and aortic root dilatation. The study showed that PEFP was significantly faster than taking a detailed AHA 12-element H&P and ECG screening. It decreased referrals to cardiology by 33%, and there was no difference statistically from echocardiography measurements performed by a cardiologist (20). Kerkhof et al. found that compared to H&P and 12-lead ECGs, frontline physicians were able to perform more accurate screening for structural abnormalities and may provide a more cost-effective solution than a full echocardiogram read by cardiologist (20). Other studies using echocardiography as a screening modality have found it effective in detecting conditions that increase the risk for SCD (20,21). There are however limitations to consider in terms of HCM as timing of screening may also effect diagnosis, because of the progressively evolving nature of HCM.
While advanced screening is a continued topic of debate, an important aspect of screening that should be considered is its potential psychosocial implications. It has been argued that false-positive screens such as with ECG may cause unnecessary restrictions from sports leading to emotional stress for young athletes and their families.
Can routine advanced screening of young athletes be cost effective?
According to Halkin et al., screening approximately 170 million high school and college athletes over 20 years would save 4,831 lives at the cost of $51–$61 billion dollars (22). In the United States, a program is typically accepted as cost-effective, if less than $50,000 to $75,000 is spent per life-year saved (4,23). Every year, it has been estimated that inclusion of ECG to screen approximately 8.5 million young athletes in the United States, it would cost the health care system ~$2.5 to $3.5 billion per year (22,24). It has been estimated that ~2.06 life years per 1,000 athletes are saved with ECG screening (i.e., $42,000 per life-year saved) (22). ECGs can detect up to 94% of most significant heart conditions, it is non-invasive, and considered cost-effective when compared to other tests such as Pap smears, mammography, and Prostate-Specific Antigen (PSA) (23,25). Overall, the routine use of screening with ECGs is expensive; however, to determine whether or not screening with ECGs should be used from an economic standpoint, more consistent data regarding false-positive rates would be needed.
A recent development in the ECG screening in athletes is that of portable ECG technology. The US Food and Drug Administration (FDA) recently approved the use of mobile heart monitoring where a smart phone is used to monitor ECGs by the patients themselves. Various alerts are sent to the patient if certain rhythms are detected based on a FDA-approved algorithm. Patients can then choose to share their alerts with their physician (26). For atrial fibrillation, the app has been found to be 99.2% specific in college athletes; whereas, the sensitivity was not determined due to vacant athlete testing positive (27). The use of this modality at present is controversial given its obvious shortcomings.
While full echocardiography screening costs would be very high, considering a limited echocardiogram screen such as used in the ESCAPE protocol using portable echo-machines performed by frontline or primary care physicians trained specifically for this may be a future consideration.
Conclusions
In summary, cardiac screening in young athletes remains a controversial topic in the US. Current AHA guidelines recommend a 14-element checklist to screen for cardiac disease in young athletes without the use of screening ECG. Recent research and evidence showed that this checklist is in fact an inadequate screening tool with a low sensitivity. The consideration of screening all young athletes with an ECG is not feasible given the financial burden it would place on our healthcare system, especially when the incidence of SCD is low. When ECGs are done, they should be evaluated using the 2013 Seattle criteria. Application of the Seattle criteria has increased the sensitivity and specificity of detecting young athletes at increased risk for SCD. While routine ECG screening is not cost effective or recommended, the use of screening portable echo is promising, although more research is needed to determine the cost effectiveness of this modality.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Maron BJ, Doerer JJ, Haas TS, et al. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation 2009;119:1085-92. [Crossref] [PubMed]
- Maron BJ, Haas TS, Ahluwalia A, et al. Demographics and Epidemiology of Sudden Deaths in Young Competitive Athletes: From the United States National Registry. Am J Med 2016;129:1170-7. [Crossref] [PubMed]
- Maron BJ, Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation 2006;114:1633-44. [Crossref] [PubMed]
- Maron BJ, Friedman RA, Kligfield P, et al. Assessment of the 12-lead electrocardiogram as a screening test for detection of cardiovascular disease in healthy general populations of young people (12-25 years of age): a scientific statement from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol 2014;64:1479-514. [Crossref] [PubMed]
- Drezner JA, Ackerman MJ, Anderson J, et al. Electrocardiographic interpretation in athletes: the ‘Seattle criteria’. Br J Sports Med 2013;47:122-4. [Crossref] [PubMed]
- Zorzi A, ElMaghawry M, Corrado D. Evolving interpretation of the athlete's electrocardiogram: from European Society of Cardiology and Stanford criteria, to Seattle criteria and beyond. J Electrocardiol 2015;48:283-91. [Crossref] [PubMed]
- Weiner RB, Hutter AM, Wang F, et al. Performance of the 2010 European Society of Cardiology criteria for ECG interpretation in athletes. Heart 2011;97:1573-7. [Crossref] [PubMed]
- Uberoi A, Stein R, Perez MV, et al. Interpretation of the electrocardiogram of young athletes. Circulation 2011;124:746-57. [Crossref] [PubMed]
- Pickham D, Zarafshar S, Sani D, et al. Comparison of three ECG criteria for athlete pre-participation screening. J Electrocardiol 2014;47:769-74. [Crossref] [PubMed]
- Bessem B, de Bruijn MC, Nieuwland W. The ECG of high-level junior soccer players: comparing the ESC vs. the Seattle criteria. Br J Sports Med 2015;49:1000-6. [Crossref] [PubMed]
- Wasfy MM, DeLuca J, Wang F, et al. ECG findings in competitive rowers: normative data and the prevalence of abnormalities using contemporary screening recommendations. Br J Sports Med 2015;49:200-6. [Crossref] [PubMed]
- Brosnan M, La Gerche A, Kalman J, et al. The Seattle Criteria increase the specificity of preparticipation ECG screening among elite athletes. Br J Sports Med 2014;48:1144-50. [Crossref] [PubMed]
- Dunn TP, Pickham D, Aggarwal S, et al. Limitations of Current AHA Guidelines and Proposal of New Guidelines for the Preparticipation Examination of Athletes. Clin J Sport Med 2015;25:472-7. [PubMed]
- Harmon KG, Zigman M, Drezner JA. The effectiveness of screening history, physical exam, and ECG to detect potentially lethal cardiac disorders in athletes: a systematic review/meta-analysis. J Electrocardiol 2015;48:329-38. [Crossref] [PubMed]
- Drezner JA. Contemporary approaches to the identification of athletes at risk for sudden cardiac death. Curr Opin Cardiol 2008;23:494-501. [Crossref] [PubMed]
- Maron BJ, Shirani J, Poliac LC, et al. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA 1996;276:199-204. [Crossref] [PubMed]
- Fudge J, Harmon KG, Owens DS, et al. Cardiovascular screening in adolescents and young adults: a prospective study comparing the Pre-participation Physical Evaluation Monograph 4th Edition and ECG. Br J Sports Med 2014;48:1172-8.
- Corrado D, Basso C, Schiavon M, et al. Does sports activity enhance the risk of sudden cardiac death? J Cardiovasc Med (Hagerstown) 2006;7:228-33. [Crossref] [PubMed]
- Vetter VL, Dugan N, Guo R, et al. A pilot study of the feasibility of heart screening for sudden cardiac arrest in healthy children. Am Heart J 2011;161:1000-6.e3. [Crossref] [PubMed]
- Kerkhof DL, Gleason CN, Basilico FC, et al. Is There a Role for Limited Echocardiography During the Preparticipation Physical Examination? PM R 2016;8:S36-44. [Crossref] [PubMed]
- Grazioli G, Merino B, Montserrat S, et al. Usefulness of echocardiography in preparticipation screening of competitive athletes. Rev Esp Cardiol (Engl Ed) 2014;67:701-5. [PubMed]
- Halkin A, Steinvil A, Rosso R, et al. Preventing sudden death of athletes with electrocardiographic screening: what is the absolute benefit and how much will it cost? J Am Coll Cardiol 2012;60:2271-6. [Crossref] [PubMed]
- Woolf SH, Husten CG, Lewin LS, et al. The economic argument for disease prevention: distinguishing between value and savings. A prevention policy paper commissioned by partnership for prevention. Available online: http://www.prevent.org/data/files/initiatives/economicargumentfordiseaseprevention.pdf
- Asplund CA, O’Connor FG. The Evidence Against Cardiac Screening Using Electrocardiogram in Athletes. Curr Sports Med Rep 2016;15:81-5. [PubMed]
- Higgins JP, Cadigan JB 3rd. Electrocardiogram Screening in Athletes: A Good Return on Investment? Am J Med 2016;129:e3-5. [Crossref] [PubMed]
- Jacob JA. Interassociation Task Force Punts Decision on Universal ECG Screenings for Athletes. JAMA 2016;316:19-21. [Crossref] [PubMed]
- Haberman ZC, Jahn RT, Bose R, et al. Wireless Smartphone ECG Enables Large-Scale Screening in Diverse Populations. J Cardiovasc Electrophysiol 2015;26:520-6. [Crossref] [PubMed]


