Instrumentation for minimally invasive surgery in pediatric urology
Introduction
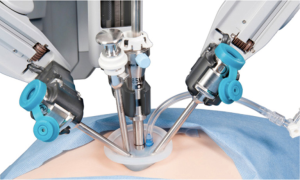
Minimally invasive surgery (MIS) is redefining the field of surgery. The term is used to describe a number of surgeries as well as diagnostic innovative procedures; all done with specially designed thin instruments through tiny incisions. MIS includes laparoscopy (surgery through small holes), endoscopy (diagnostic and therapeutic procedures performed through the body’s organs and vessels) and robotic surgery. In traditional surgery, a surgeon needs to make a large incision in order to operate. With MIS, the surgeon makes a few small holes—usually less than 1/2 an inch, called “ports”: a port is a hollow tube or cannula with a cap that contains a valve to prevent gas leak but allows instruments to pass through. The surgeon then inserts specially designed, thin instruments and sophisticated video equipment (Figure 1) to perform the operation through these small openings. The goal of MIS is to minimize patient morbidity while maintaining successful outcomes. Typical benefits of MIS include less pain and complications, quicker return to normal activities, and less tissue damage (scarring) (1). Of note, the first reported use of laparoscopy in paediatric urology was for patients with non-palpable undescended testes in the 1960s, and diagnostic laparoscopy in this setting has gained widespread acceptance among paediatric urologists. The first paediatric laparoscopic pyeloplasty is dated on 1995. Initially the utility of endourology and laparoscopy was hampered by bulky equipment and limited tools. Since 1995 several companies (Karl Storz Endoscopy, Richard Wolf, Jarit instruments) have been willing to work with paediatric surgeons to develop instruments that were appropriate in size and function. Today technological advances have provided excellent optics and fine dissecting instruments, sets of instruments appropriate for infants, toddlers, older children and teenagers. For paediatric urology cases, the limitation of conventional laparoscopic equipment (telescopes which provide limited 2-dimensional (2D) image, limited instrument mobility or decreased ergonomics) and the steep learning curve associated with its use in reconstructive procedures, have led to a modest adoption for this type of procedures. The da Vinci surgical system has introduced the benefits of an intuitive interface, highly magnified 3-dimensional (3D) (stereoscopic) visualization that improves hand-eye coordination, and greater degrees of instrument articulation and control for robotic assisted laparoscopic procedures. The increased precision of and facility with instruments offered by robotic assistance is readily seen in paediatric procedures, specifically those that are reconstructive in nature, and thus require intensive dissection and suturing.

Endourologic surgery and instrumentation
Endourologic surgery involves specialized instruments that can enter the urinary tract via the urethra eliminating the need for incisions (2,3). Several companies manufacture paediatric endoscopic equipment (Storz/Olympus, Wolf). Given to the delicate nature of this equipment it is crucial to have several scopes available in case of malfunction or other needs. Paediatric endourologic procedures include:
- Deflux injection for vesicoureteral reflux (VUR);
- Bladder outlet injection for urinary incontinence;
- Removal of stones from the kidney, ureter or bladder;
- Treatment of posterior urethral valves, a congenital urinary tract blockage, in infants;
- Endoscope management of ureterocele;
- Ureteroscopy;
- Endopyelotomy for obstructed kidneys.
In a term male paediatric patient, the urethra typically can accept a 7.5 or 8 Fr calibre cystouretroscope. Rigid (operative) paediatric cystoscopes range from 5 Fr to adult sizes (Figure 2A). Flexible cystoscopes are used when the purpose is merely to look inside the low urinary tract. The “all in one” cystoscope is one-piece instrument with united telescope and sheath, and with 2.5–3–5 Fr working channel (rather limiting). The other scopes consist of two pieces: the interchangeable telescope (0°, 30° and 70°) and the sheath.
A range of reusable and disposable equipment exist (such as graspers, biopsy forceps, bugbee electrode, wires, catheters, stents, balloons, baskets, laser fibres, and STING needles), whose use may be impossible with working channels calibre less than 5 Fr. Paediatric cystoscopes with an offset lens allow straight entry into the working channel for the use of the STING needle (in case of VUR and bladder incontinence). STING needles can be found in sizes 3 to 5 Fr and made from plastic body with metal end or metal body depending on the manufacturer, with a black line marking 5 mm from the needle tip. Rigid and flexible cystoscopes are necessary for bladder stone management. To achieve stone fragmentation, electrohydraulic, ultrasonic, combined ultrasonic and pneumatic, or holmium laser lithotripsy can be used. Rigid (3 or 5 Fr) and flexible probes (0.2–1 mm) are available. Paediatric resectoscopes, ranging from 7.5 Fr to adult sizes, require loops, balls, blades, hook, unique to the Fr size of the resectoscope. Instrumentation that should be available for valve resection includes:
- Paediatric cystoscope 6–7.5 Fr: to perform an initial diagnostic cystoscopy;
- Paediatric resectoscope 11 F: if the neonatal urethra is too small to accommodate the resectoscope, the membrane can be ablated using a 7.5 Fr cystoscope and a 3 Fr ureteric catheter;
- Cold knife bugbee and diathermy electrodes.
In case of ureterocele a variety of scopes should be available. A 9.5 Fr offset cystoscope with a 5 Fr working channel is a good option. There is a variety of probes that may be used to puncture or incise the ureterocele depending on the surgeon’s preference. These probes involve electrocautery current.
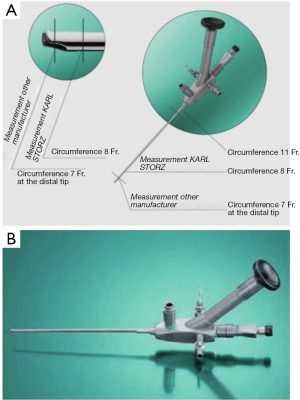
Rigid paediatric cysto-urethroscopes
Today the marketplace provides the smallest possible instrumentation (Figure 2B, Figure 3) and a complete array of integral cystoscopes, where the sheath and the bridge are built in to the endoscopes. Integral cystoscopies allow for quick, easy, diagnostic and therapeutic examinations. The large variety in sheath sizes allows the smallest sheath possible for children to help reducing potential strictures.
See “Accessories for 8 and 9.5 cystoscopes” (Figures 4-8).
9.5 Fr offset operating urethro/cystoscope: also known as the “stinger” it was designed for sub-trigone injections. Its offset eyepiece is ideal for video applications as it removes the camera from the operative field and serves as an excellent handgrip for both the endoscope and the camera. The 5 Fr insert capacity allows the use of flexible or rigid forceps coupled with excellent flow capabilities.
Rigid neonatal cystourethroscope
The new ultrathin paediatric systems for endoscopy in neonates and children propose a 1.2 mm telescope and smaller calibre endoscopes (antireflux endoscope, urethrotome, resectoscope) with a wide working channel (that allows 4 or 5 Fr rigid instruments) (Figure 9). Consequently, the examination of the lower urinary tract in neonates today is easy, the urethrotome can be used for the incision of scarred tissue in urethral stricture, and in case of urethral valves they can be incised with a small hook knife or the resectoscope (the new working element of the resectoscope is designed to permit the urethrotome to cut from 6 to 12 o’clock) (Figure 10). In case of VUR, with the proximal working channel in the reflux sheath, the rigid needles can be gently inserted into the working channel without becoming blunt. The working channel guides the reflux needle with excellent precision.

Pediatric cysto-uretero-fiberscopes
Diagnostic and therapeutic applications
- Lithotripsy and stone extraction in ureteral and renal tract;
- Access to entire renal tract, including lower renal calyces;
- Detection of pathology in anatomically difficult areas;
- Diagnostic indications:
- Identyfing causes of hematuria;
- Differential diagnosis in filling defects;
- Diagnosis of ureteral tumors;
- Therapy:
- Removing calculi/foreign objects;
- Treating ureteral tumors;
- Coagulatin hemorrhage;
- Disintegrating ureteral calculi.
The ceramic tip at the distal end of the working channel prevents thermal damage to the fiberscope during laser treatment. The tip enables laser to be used at a shorter distance to the fiberscope tip. Passive deflection components enhance manoeuvrability and provide easier access to the renal calyces. A larger angle upward from 270° and downward from 270° allows the orientation and visualization of the entire renal tract, including the collecting system. The angulation system allows greater laser fibres to be used without compromise the angulation properties—50% magnification of image. Working channel allows using wide choice of instruments (accessories: coagulating electrode, guide wire, grasping forceps, biopsy forceps; CALCULASE laser system for endoscopic treatment of bladder, ureter and kidney stones) (Figure 11).

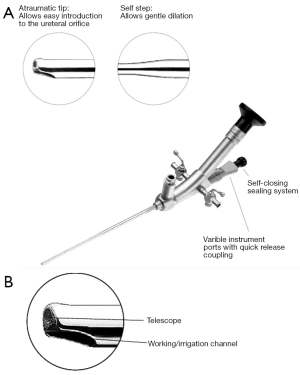
Paediatric uretero-renoscopes
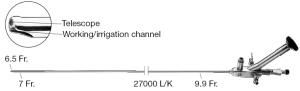
Pediatric ureteroscopic procedures are similar to their adult counterparts. The ureteroscope (rigid or flexible) is used for endoscopic evaluation and management of diverse conditions involving the upper urinary tract (ureteral and renal calculi) even in the smallest children. Endoscopic treatment can be effective in highly selected children with intraluminal ureteral obstruction. These conditions include renal hemangiomas or arteriovenous malformations, ureteropelvic junction obstruction, ureteral strictures, ureteral polyps, ureteral and renal calculi. Endoscopic treatment of pediatric urolithiasis is the treatment of choice. Holmium:YAG laser lithotripsy is the intracorporeal lithotriptor of choice thanks to its safety and efficacy. Storz offers a variety of uretero-renoscopes tailored to the needs of users and patients with a sheath circumference of 7 to 9.5 Fr and working channels of 4.8 to 6 Fr. Both rigid and flexible uretero-renoscopes are supplemented by various forceps and lithotripsy systems (Calculase II, Calcuson, Calcusplit) to offer outstanding options for stone treatment. The Laser system for endoscopic stone therapy offers precise cutting effect in case of stenosis, extremely fast lithotripsy, least tissue damage, high success rate, and lithotripsy under endoscopic control. The ultrathin uretero-renoscope (Figure 12) with a distal tip of 6.5 Fr and a sheath of 7 Fr is particularly indicated in children. The atraumatic sheath end offers easy insertion into the ureter. An excellent view is ensured by the irrigation guaranteed by a large working channel.
Flexible uretero-fiberscopes
Used to access the entire internal collecting system (Storx Flex-X2) (Figure 13). The system helps to safeguard the scope’s working channel from both mechanical (puncture of the instrument channel) and thermal damage. The FLEX-GUARD sheath (9.5 Fr) is designed to help protecting against this type of damage during insertions and is suitable for children. Deflection of distal tip (270° up/270° down), working channel inner diameter 3.6 Fr, sheath size 7.5 Fr, working length 45–67 cm.
Laparoscopic urologic surgery
The use of laparoscopy in urology has grown significantly over the past 30 years. Children’s special anatomic and pathological characteristics require instruments that are appropriately adapted to them in every respect. A special product range for this patient group exists, with products perfectly tailored to the needs of the youngest patients. Smaller diameters mean less scar formation and less postoperative pain. For surgeons, shorter instruments and greater stability ensure safety and ergonomics (2,4,5). Laparoscopic urologic procedures for children include:
- Orchidopexy to bring down undescended testicles from the abdomen;
- Pyeloplasty for obstructed kidneys—the vascular ‘hitch’ procedure;
- Diagnosis and treatment of disorders of sexual development;
- Nephrectomy—partial nephrectomy;
- Varicocelectomy;
- Transvesicoscopic Cohen ureteric reimplantation;
- Adrenalectomy;
- Intersexual states.
Instruments set for urology laparoscopic paediatric surgery
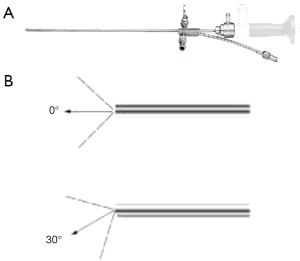
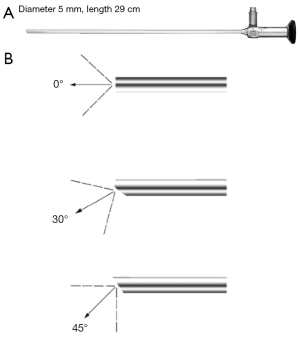
Telescope (Figure 14) and trocars (Figure 15)

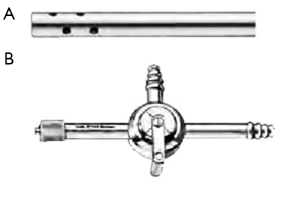
The new trocar generation (Figure 16) for laparoscopic paediatric surgery combines single use with reusable components. The ergonomic shape of the trocar ensures safe and reliable handling during placement. The new plastic trocar housing ensures reduced weight and the new valve seal is intended for single use (available in package of 10). These trocars are available in diameters 2.5, 3.5 and 6 mm with working length of 6 mm.
Self-retaining trocars (Figure 17) have been developed especially for neonates and infants. The distal tip of the cannula enables fixation under the abdominal wall preventing the cannula from slipping away. The sheath is short, so that the tip of the cannula doesn’t hinder the opening of the jaws. Diameters of 3.5 and 6 mm.
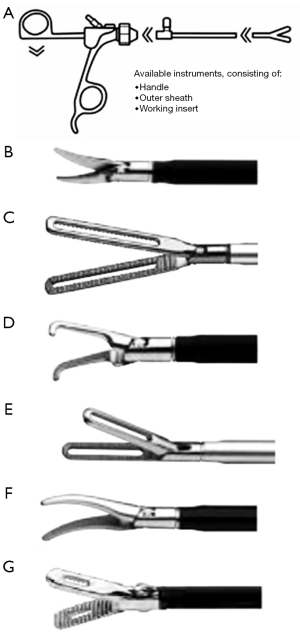
Graspers, dissectors and scissors (2–3–5 mm)
This instrument (Click-LIne series—available size 2–10 mm) (Figure 18) features great efficiency thanks to its modular construction (three-part dismantling instruments and alternatively 3 mm instruments with two-part dismantling) that offers great variability and flexibility with the combination of a wide range of jaws with various outer sheaths and click line handles. Its diameter is 3.5 mm, working length 20 cm. The same instruments are available in the rotating and bipolar adaptation, with a diameter of 3.5 mm, working length 20 cm. They are designed with a force limiter integrated in the handle to prevent the jaws from overloading while ensuring secure grasping. The insulated outer sheath is 360° rotating.
Electrodes (Figure 19)
Insulated sheath with connector pin for unipolar coagulation (monopoly diathermy). Alternative coagulation systems: harmonic scalpel (vessel sealing) and LigaSure (provides a combination of pressure and energy to create vessel fusion up to 7 mm diameters).
Other instruments
Other instruments are suction and irrigation tubes (Figure 20), knot tiers (Figure 21), endobag (Figure 22), endoloop (Figure 23), endoclip (Figure 24), needle holders 2 and 3 mm (Figure 25).


Pediatric urology procedures
The open or Hasson technique is preferable in children access the abdomen. In this technique a 5–12 mm open minilaparotomy is created. If a Hasson trocar (Figures 26,27) is used, sutures are placed into the fascia and secured to the side arms of the trocar to hold it in place. The same sutures can be used for fascial closure at the end of the case. Alternatively, a blunt tip balloon trocar can be used. This device has a retention balloon, which lies under the fascia and is filled with 5–10 cc of room air. A moveable foam pad slides down to the skin and is secured in place with an incorporated clasp to prevent leakage of air.
Orchidopexy
The principles of laparoscopic surgery for the undescended impalpable testis are similar to those of open approach: mobilization of the spermatic vessels and the vas, hernia repair and redirecting the testis to the scrotum via a straight route. The advantage of laparoscopy is to mobilize the proximal vessels.
Key instruments:
- 5 mm camera: umbilical port;
- Two working ports (2 or 3 mm trocars) anterior axillary line: dissection and coagulation;
- 2 mm grasper and 5–10 mm trocar (dilator) to create the neo-inguinal canal through the Prentiss manoeuvre.
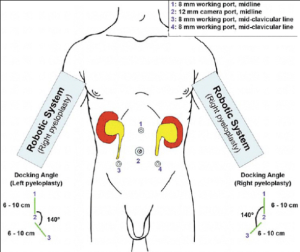
Pyeloplasty
The most significant challenge in laparoscopic pyeloplasty is the difficulty of precise intracorporeal suturing, which requires a significant learning curve. For this reason this procedure has not gain widespread acceptance for treating pelvi-ureteric junction obstruction.
Key instruments:
- 5 mm telescope 30°;
- 6 mm Hasson umbilical port;
- Transperitoneal or retroperitoneal approach: 3 ports (3 or 5 mm) one under the costal margin the other in the ipsilateral iliac fossa;
- Cystoscopy: to place a guidewire in the ureter;
- Dissector (Kelly forceps);
- Bowel grasper;
- Scissors 3 mm, to spatulate the ureter laterally;
- Diathermy hook;
- 3 mm needle holder;
- Small curved needle for anastomosis passed through a 3–5 mm port;
- Suction/irrigation device;
- Double pig tail stent (JJ 5.2 Fr 8–20 cm multilength silicone) placed retrograde over the guide wire or alternatively nephrostomy tube.
Nephrectomy (removal of benign lesions and non-functional kidneys)
Key instruments:
- Transperitoneal or retroperitoneal (lateral or prone) approach: 3 ports + 1 for retraction;
- Dissector: dissect from lower pole upwards the ureter before the hilum.
Vessel size is the clue to decide between:
- Clips forceps: 5 mm;
- Electocautery or harmonic scalpel or LigaSure (for small and atretic vessels);
- Clips + intracorporeal tie if clips too small alone;
- Vascular endoscopic stapling device for difficult hilum:
- Extraction bag;
- Morcellator;
- Ureteral catheter (Methylene blue text for urine leakage).
Partial nephrectomy (non-functional segment of a duplex system)
The demarcation line, which separates the affected unit from the normal one, is generally clear (the first is hydronephrotic and cystic). The critical moment is protection of the vasculature of the remnant segment. For this procedure the laparoscopic learning curve is prolonged, and robotic-assisted partial nephrectomy is gaining popularity.
Key instruments:
- Primary camera port: 6 or 10 mm Hasson;
- Two secondary 5 mm ports;
- 5 mm telescope 30°;
- Dissection (Kelly forceps);
- Harmonic scalpel or 5 mm endoclips for vessels <3 mm diameter (3 clips, 2 remaining on the proximal stump);
- Endoloop to encircle the moiety;
- Hook scissor to transect the parenchyma;
- Endopouch for specimen retrieval.
Antireflux procedure (ureteric reimplantation)
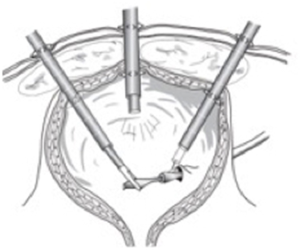
Limited data are available to assess the efficacy and safety of this procedure. The most commonly used is the Lich-Gregoire technique, with an efficacy similar to that of open surgery. The transvesical pneumovesicoscopic approach (Figure 28) mimics the Cohen procedure.
Key instruments:
- Extravesical implantation:
- Cystoscope: inspection and insertion of 3 Fr ureteral catheter;
- 5 mm telescope: infraumbilical port;
- 3 mm trocars midclavicular lines and infraumbilical (hook, grasper, dissector, needle holder);
- Babcock retractor or umbilical tape to isolate the ureter.
- Intravesical implantation:
- Operative cystoscope: insertion of two ureteral stents and direct vision of trocars insertion;
- Alternatively: resectoscope to insert a knife to dissect out the ureter (intra and partially extravesical);
- Two 5 mm balloon tip ports (locking trocars): the external cuff is pressed down to seal the port within the bladder;
- Continuous suction (urethral catheter): to maintain decompressed the bladder.
Retroperitoneal approach
The patient is in prone or flank position (Figure 29). Key instruments:

- The space can be created with a telescope inserted in the port or using a balloon device (several balloons are available for creation of the retroperitoneal space) or the middle finger of a 8.5 glove tied to a 12 Nelaton catheter;
- 6 mm Hasson cannula secured to the skin;
- Insufflation of the retroperitoneum 10 to 12 mmHg at a flow rate of 1 L/min;
- 5 mm working port below the tip of the 11th rib;
- 5 mm working port through the paravertebral muscles.
Varicocelectomy: laparoscopic single channel varicocele dissection (LEVD)
This is a new surgical procedure in paediatric surgery. In this case the surgeon only uses one port through which the telescope and instrument set can be inserted (6,7). A compact operation set was created for this method. The laparoscopic one hand single-channel technique consists of an individual trocar technique (5.5 mm laparoscope with 3.5 mm working channel) (Figure 30). It reduces surgical trauma and provides a scar less method. Special bipolar forceps (Figure 31) are required for vascular dissection (with bipolar generator which avoids compromising the adjacent structures). A suction and irrigation function maintains visibility. The option to continue using additional 3.5 mm working trocars exists. The 5 mm longitudinal incision in the umbilicus leaves no visible scar. Gas insufflation up to 8 mmHg is carried out via the 5.5 mm trocar. With a 3.5 mm scissors the parietal peritoneum is dissected, 2 cm above the inner inguinal ring. A dissector is used to expose the vessels. Bipolar grasping forceps are used to facilitate coagulation. The coagulation section should be at least of 5 mm. Scissors can be used to resect the entire vessel. If the following inspection reveals other vessels, the procedure is repeated.
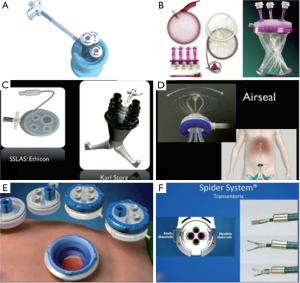
Laparoscopic single-site surgery (LESS)
Urologic paediatric LESS was reported for the first time in 2008 (7-9). Although the subsequent literature (case reports and initial small case series) describes the use of LESS for most surgeries (nephroureterectomy, orchidopexy, varicocelectomy, ureterolithotomy, utricle excision), the preferred option in paediatric urology population for reconstructive procedures remains laparoscopic and robotic surgery. In 2008, Kaouk and Palmer reported for the first time the use of single multifunctional port for varicocelectomy in three patients (10). In 2009 Park described the first LESS nephrectomy. LESS requires an experienced laparoscopic skill set for the safe and effective completion of surgery (11). Currently, commercially available instruments designed for adults cannot be used for children younger than 3 years. Most authors used a 5 mm 0° or 30° telescope whereas others have favoured the advantages provided by a reticulating telescope or longer length laparoscope to decrease the degree of collision between the surgeon and the laparoscope operator.
Olympus endo-eye
5 mm, flexible tip telescope that delivers 100-degree angulations and a 85° field of view (Figure 32).
Platforms (Figures 33,34)
Multichannel single port device placed via an open technique (midline umbilical incision), not suitable for robotic assisted laparoscopy in children:
- Olympus TriPort (12–15 mm incision) (Figure 35);
- Gelpoint Mini (15 mm incision) (Figure 36);
- Covidien SILS access port (25 mm incision) (Figure 37);
- Alternatively: multiple ports (3 or 5 mm) inside the same skin incision (multiple fascial holes) and additional 2 or 3 mm ports if necessary;
- Each port accommodates different instruments (straight, articulating, prebent) (Figure 38):
- Standard straight instruments cross the point of entry resulting in right hand working in the left and vice versa;
- Flexible reticulating or curved instruments allow easier manoeuvres and intracorporeal triangulation.
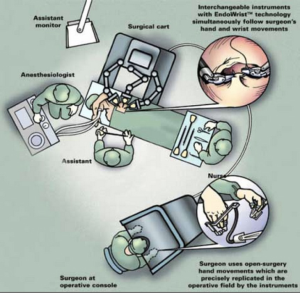
Robotic surgery
Robotics is the newest and most exciting technique in minimally invasive surgery, an important advance in laparoscopic surgery (12). The da Vinci® surgical system from intuitive surgical reproduces the dexterity of the human hand while providing a 3D view of the surgical field. Paediatric urology is the paediatric surgical specialty that most likely uses the da Vinci system, and, since there are few well-accepted indications for robotic surgery in paediatric urology, few children’s hospitals have been willing to commit their resources to this technology. The da Vinci operating room (OR) (Figure 39) must be large, because the robot and its cables take up a lot of space. Before the patient enters the room, the paediatric urologist and anaesthesia staff should plan how the patient and OR table will be positioned, where the robot will be docked, where the anaesthesia equipment will be, and were the surgical assistant will sit. The scrub-nurse should have da Vinci laparoscopic instruments. The da Vinci surgical system consists of a surgeon console, a patient-side cart with the interactive robotic arms, a vision cart (“the video tower”) and the proprietary Endowrist robotic instruments. The patient-side cart with the robotic arms consists of up to four working arms, although the fourth arm is seldom used in the paediatric population because of the smaller working spaces in paediatric patients. In addition avoiding the fourth arm can reduce the initial capital investment required for the system. The three main robotic arms consist of:
- The camera arm: two cameras in a single metallic sheath, designed to mimic ocular function of a surgeon’s eyes. The signal from each of the two cameras is delivered to the surgeon console that processes the two images to provide the surgeon with a single 3D image. This provides the surgeon with a 10-fold magnification of visualization;
- The two instrument arms (each arm attached to its respective laparoscopic port);
- The middle camera arm designed to hold the system’s camera telescope;
- The two side arms control the robotic instruments, which are inserted and removed by the bedside assistant;
- The console: a distinct unit at which the surgeon is comfortably seated while handling robotic controls (including arm position, focus, zoom, camera position, instrument movements dampening any potential hand or arm tremors);
- Endowrist articulation: allows for more precise control and multidirectional manipulation of tissue than standard laparoscopy. It mimics human wrist articulation (7 degrees of freedom, 90° of articulation, intuitive motion, finger-tip control, motion scaling and tremor reduction).
A wide range of instruments is available for robotics. Common instruments in open surgery and laparoscopy (needle drivers and Maryland dissectors) have their robotic counterparts. Most paediatric urological procedures are performed using a 12 mm camera port and 5 mm instruments—a needle driver and 5 mm grasping instruments. The robotic set consists of:
- Laparoscopic vision tower: contains a monitor, camera, light source, and insufflator;
- Telescopes: 12 and 8.5 mm, 3D 2 build-in lenses, angled (30°) and straight (0°);
- 5 mm telescope: limited to 2D visualization;
- 8.5 mm camera + 5 mm instruments (longer articulating tip): for the majority of paediatric procedures;
- 12 mm camera + 8 mm instruments: for adolescent procedures;
- Dissectors with cautery:
- 5 mm monopolar cautery with either a hook or a spatula tip: the most commonly used, also for its tip with blunt dissection utility prior to cautery;
- Monopolar curved scissor (hot shears): sharp dissection with a smaller contact focus of cautery as compared to the hook; less used as dissector for the sharp edges of the scissors distal tip as well as for sole availability in the 8 mm size;
- Harmonic curved shears (5 and 8 mm sizes). In both, the energy is transmitted between the jaws of the device;
- Energy instruments: provide coagulation, cutting and dissection of tissues:
- Monopolar and bipolar cautery instruments (electrical energy);
- Harmonic™ ACE (mechanical energy):
- da Vinci PK™ dissecting forceps (advanced bipolar);
- Laser.
- Forceps and grasping instruments:
- Maryland dissectors and the DeBakey forceps (5 mm);
- Atraumatic bowel graspers (5 mm);
- Sharp-toothed Schertel graspers (5 mm);
- Only in 8 mm size: e.g., the ProGrasp forceps;
- Bipolar Maryland forceps 8 mm size: it allows the use of bipolar cautery in the grasping instrument without the need for an instrument change.
- Scissors:
- Curved scissors (5 mm): for dissection and cutting;
- Round tip scissors (5 mm): for certain procedures i.e., spatulation of the ureter prior to anastomosis (it allows straight incisions);
- Pott scissors (8 mm only): for fine-cutting purposes, these scissors have sharp pinpoint tips.
- Other instruments: generally available only in the 8 mm size:
- Black Diamond microforceps: makes easier wrapping the suture around the narrow tips of the forceps;
- Suture cut needle driver: has a small scissors blade in the base of the instrument’s tips that can be used for cutting sutures without an instrument change or an assistant;
- Traditional laparoscopic instruments: for paediatric surgeons, may be used through a robotic port or through accessory 5-mm laparoscopic port.
This port may reduce operative times, provide assistance with retraction (bowel-liver), suture traction, placement and removal, suction, irrigation, without the need of an instrument change. Finally this accessory port can serve as a conduit in which to place ureteral wires and stents into the ureter without the need of a separate incision. As robotic technology evolves, the list of robotic instruments is expected to grow with miniaturization of the instruments.
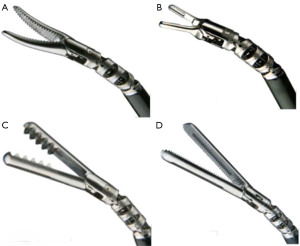
mm instruments
The snake-like movement of the 5 mm instruments requires more operating space. However, most urologic procedures are performed with Maryland grasping forceps, hook cautery, scissors, and needle holders:
- Endowrist needle driver (Figure 40);
- Endowrist scissors: round tip and curved (Figures 41,42);
- Endowrist monopolar cautery (Figures 43,44): monopolar cautery spatula and hook tip;
- Ultrasonic energy instrument (Figure 45): harmonic ACE curved shears;
- Endowrist graspers (Figure 46): Maryland dissector, DeBakey forceps, Schertel Grasper, bowel grasper.
Robotic paediatric procedures
The paediatric urology team will determine the best type of surgery for a child based on the child’s thorough exam, medical history and diagnosis. Many urological conditions are now diagnosed and treated with minimally invasive techniques. Robotic-assisted surgery can be used for complex reconstructions such as pyeloplasty, bladder augmentation or Mitrofanoff appendicovesicostomy. For Cohen procedure a 12 mm camera and two 8 mm instruments are necessary. Robotic surgery for these and other procedures have proven to give similar results as in open surgery, but with the advantage of smaller incisions and significantly shorter recovery time. As instrumentation continues to improve, more pediatric procedures will likely be performed with robotic assistance. The most commonly performed robotic procedures in the paediatric population to date are pyeloplasty and extravesical ureter reimplantation. The close approximation of robotic techniques to their open counterparts facilitates the transition to the minimally invasive option. Pyeloplasty can be performed with either transperitoneal or retroperitoneal access and offers the advantage of using smaller suture material, as fine as 7.0. Results in children older than 1 year are similar to those of laparoscopy.
Robotic-assisted pyeloplasty (Figure 47)
The robotic system helps to overcome the problem of precise intracorporeal suturing by making suturing easier thus shortening the learning curve. Similar overall operative times depend on longer robotic set-up. The recommended instruments for paediatric pyeloplasty are all 8 mm sizes:
- Dissecting forceps (Bipolar cautery PK) (Figure 48);
- Needle driver (Mega Suture Cut) (Figure 49);
- Endowrist grasper: forceps (Prograsp) (Figure 50);
- DeBakey Forceps (Figure 51);
- Round tip Scissors (Figure 52).
Monopoly cautery hook is hold in the right hand for exposure/initial dissection of the renal pelvis; Maryland dissector or DeBakey forceps in the left hand. The use of curved scissors is limited by the lack of cautery in the 5 mm version of this instrument. Curved scissors (or round tip scissors) are used for transection of the renal pelvis and the ureter, whilst round tip scissors facilitates spatulation even of a small ureter with its straight tips. Two needle drivers are generally used to perform the anastomosis or alternatively, one needle driver and one grasping instrument. While robotic surgery can be used for ureteral reimplantation, nephrectomy, heminephrectomy and orchidopexy, simple laparoscopy is usually sufficient for these procedures. Robotic surgeries may take longer than other types of minimally invasive surgeries due to time needed for positioning the instruments and other equipment.
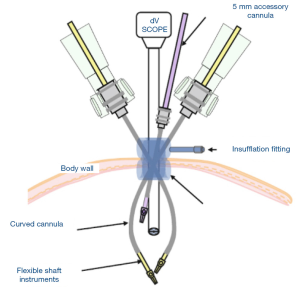
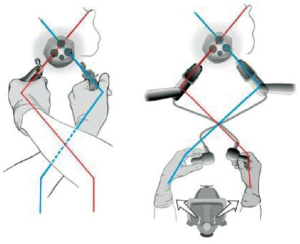
Single-site 5 mm instruments
Instruments and camera cross within the Single-site (Figures 53,54) and use remote centre technology to minimize cannula collisions, arm interference and port-site movements. da Vinci software automatically detects and re-associates the user’s hands with the instruments tip to create intuitive movement through crossed cannulae. Sigle site port: 5-lumen port, 1.5 cm incision, provides access for two single-site instruments (plus a 8.5 mm endoscope).
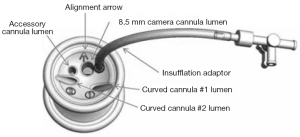
Curved 5 mm instrument cannulae:
- Designed to minimize external collision and optimize triangulation;
- Curved architecture separates the instruments arm outside the body;
- 5 mm semi-rigid instruments: used through curved cannulas;
- Bipolar cautery (Maryland forceps and fenestrated forceps);
- Monopolar cautery (hook);
- Needle drivers (wristed needle driver and curved needle driver);
- Clip applier;
- Graspers;
- Maryland dissector;
- Suction irrigation.
Conclusions
There has been a continued expansion in the application if laparoscopy in the paediatric population. Improvements in optics and instrumentation and the use of robotic assistance have brought new dimensions to the use of MIS in the paediatric population. Laparoscopy has provided a unique opportunity for paediatric urologists to work in a small space around and inside the urinary bladder. It has also allowed exploration of the complete urinary system, from kidney to bladder with just a rotation of axis of trocars, holding the laparoscope and the working instruments, thus aiding to deal with all major paediatric urologic diseases in minimally invasive fashion. Smaller scars, less pain, and quicker recovery are all potential benefits of laparoscopy, but there is also the potential of causing harm if the application of minimally invasive technique is not done properly, particularly because of lack of adequate experience in this field. Technically most complex reconstructions in children have been achieved with the use of laparoscopic technique, but their reproducibility has yet to be proved. It is therefore important to have proper clinical trials that can objectively evaluate the use of these technically demanding techniques in children.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: Karl Storz-Endoskope has authorized the publication of figures representing some of the instruments they produce for the paediatric surgical population.
References
- Kim C, Docimo SG. Use of laparoscopy in pediatric urology. Rev Urol 2005;7:215-23. [PubMed]
- Godbole P,Koyle MA, Wilcox DT. editors. Pediatric Endourology Techniques. London: Springer-Verlag London, 2014.
- Smith AD, Badlani G, Bagley D, et al. editors. Smith's Textbook of Endourology. PMPH-USA, 2007.
- Instrument set for laparoscopic and endourologic pediatric surgery-Karl Storz Endoskope Catalogue-Endoscopes, Instruments, accessories, Units and Imaging Systems. Available online: http://www.karlstorz.com/bt/en/online-catalog.htm
- Hidas G, Watts B, Khoury AE. The evolving role of laparoscopic surgery in paediatric urology. Arab J Urol 2012;10:74-80. [Crossref] [PubMed]
- Abdel-Karim AM, Zaytoun O. Laparoendoscopic single-site surgery in urology: Evaluation of complications. Arab J Urol 2012;10:89-96. [Crossref] [PubMed]
- Bansal D, Cost NG, Bean CM, et al. Pediatric urological laparoendoscopic single site surgery: single surgeon experience. J Pediatr Urol 2014;10:1170-5. [Crossref] [PubMed]
- Soto-Aviles OE, Escudero-Chu K, Perez-Brayfield MR. Laparoscopic Single-Site Surgery in Pediatric Urology: Where Do We Stand Today? Curr Urol Rep 2015;16:68. [Crossref] [PubMed]
- Abdel-Karim AM, Elmissery M, Elsalmy S, et al. Laparoendoscopic single-site surgery (LESS) for the treatment of different urologic pathologies in pediatrics: single-center single-surgeon experience. J Pediatr Urol 2015;11:33.e1-7. [Crossref] [PubMed]
- Kaouk JH, Palmer JS. Single-port laparoscopic surgery: initial experience in children for varicocelectomy. BJU Int 2008;102:97-9. [Crossref] [PubMed]
- Han WK, Park YH, Jeon HG, et al. The feasibility of laparoendoscopic single-site nephrectomy: initial experience using home-made single-port device. Urology 2010;76:862-5. [Crossref] [PubMed]
- Chandrasoma S, Koh CJ. Instrumentation during pediatric robotic anastomoses and reconstruction. In: Ost MC. editor. Robotic and Laparoscopic Reconstructive Surgery in Children and Adults. Humana Press, 2011:17-27.