
The challenges of screen time in children with typical development and children with developmental disorders during COVID-19 pandemic
Highlight box
Key findings
• Children spent more time on screens during the COVID-19 pandemic. The screen time of children with autism spectrum disorder (ASD) and those with attention deficit hyperactivity disorder (ADHD) was longer than that of children with typical development before the emergence of COVID-19. Risk factors for screen time included age, pre-COVID-19 screen time, screen time used for learning, screen time of siblings, use of screens as “babysitters”, and lack of parental restriction.
What is known and what is new?
• Children’s lifestyles have changed dramatically during the COVID-19 epidemic, including those with developmental disabilities. Electronic screen exposure has adverse effects on children’s development.
• This study analyzed the changes in children’s screen time and lifestyles in China, and identified the risk factors of screen time in children with and without developmental disabilities.
What is the implication, and what should change now?
• Much effort should be directed at managing children’s screen time and promoting healthier lifestyles, including children with developmental disorders.
Introduction
The COVID-19 (coronavirus disease 2019) pandemic was a universal public health issue (1,2). By May 13, 2022 (Beijing time, GMT+8), the World Health Organization (WHO) had reported 517,648,631 confirmed cases and 6,261,708 deaths worldwide. China adopted a series of methods and public health policies to effectively control the spread of COVID-19 (3). However, due to the pandemic of the Omicron variant, confirmed cases in China continued to surge. Epidemic prevention strategies, including online teaching, limited outdoor activities, isolation, and social distancing, can bring about significant changes in lifestyles (4) which may increase children’s sedentary behaviors (5). As an important aspect of sedentary behavior, there is much concern regarding changes in screen exposure among children and adolescents during the COVID-19 pandemic, and this may progress from a temporary short-term issue to a long-term permanent problem, thus affecting the development of children.
Increased electronic screen time may have many adverse effects, which may affect children more than adults (6). Especially for children before the age of 3, it may affect the overall cognitive development of children (7). The American Academy of Pediatrics (8) advises that children under 18–24 months should avoid digital media (except video chat); and children 2–5 years old should limit screen time to 1 hour per day of high-quality program, accompanied by parents. In the early days of the COVID-19 epidemic, preliminary researches (9-11) suggested that the COVID-19 pandemic would lead to changes in children’s sedentary behavior, screen time, and the physical activity time, not only in China but also other countries. Furthermore, the effect of screen exposure in children with neurodevelopmental disabilities is more concerning to pediatricians than in children with typical development. Researches show (12-14) that children with autism spectrum disorder (ASD) appear to be more attracted to electronic screens, are exposed to screens longer, at a younger age , and are more prone to addiction-like symptoms than children with normally development. The anti-social aspects of screen interaction may exacerbate the symptoms of ASD (15) and may play a role in the onset of ASD (16). For children with attention deficit hyperactivity disorder (ADHD), symptoms have been shown to be positively correlated with screen time (17-19), with a higher risk of negative effects on academic performance, attention, and cognitive skills (18). Some surveys (20,21) have demonstrated that changes in children’s mental health may be related to lifestyle changes during the COVID-19 pandemic.
Current studies have found that during the lockdown associated with the COVID-19 epidemic, the total media exposure time increased by 46% in ADHD children (22) and this may have aggravated the symptoms of ADHD (23), including externalizing behavior problems (24) and emotional problems (25,26). Increased screen time was also reported in children with ASD in different countries (27-29). However, there is a paucity of data concerning the electronic screen status of children with ASD/ADHD during the COVID-19 pandemic. Most of the available evidence is data from the early stages of the COVID-19 pandemic, and there is currently no relevant study focusing on the changes in children’s electronic screen time after such a long lockdown of COVID-19 due to the Omicron variant. Therefore, we conducted this survey to understand the changes in children’s screen time and lifestyles in the background of China’s strong and long term prevention and control measures for more than two years, as well as the different characteristics of screen time changes in children with developmental disabilities and typically developing children during the epidemic. The purpose is to draw attention to the potential adverse effects of lifestyle changes on children’s development during the normalized management of COVID-19, and to help teachers, parents, education departments, and health departments to gradually improve the policies and management for children and adolescents in epidemic control. We present this article in accordance with the SURGE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-162/rc).
Methods
Participants
For this cross-sectional survey, children undergoing physical examination and children with developmental disorders attending parent training programs in the Developmental and Behavioral Department of the First Hospital of Jilin University, Changchun City, China, were enrolled. Questionnaires were distributed in the WeChat group sponsored by pediatrician of the parent training program in our department. The following inclusion criteria were applied: patients under 18 years old, who had been admitted to our department and been clearly diagnosed with developmental disorders or confirmed to have typical development by a professional pediatrician in our department; and all children with developmental disabilities participated in the parent training program and/or children rehabilitation program in our department. Participants who had not been explicitly diagnosed by our professional pediatrician or did not agree to complete the questionnaire were excluded from this study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the First Hospital of Jilin University (No. 21K096-001).
Procedure
Questionnaires were distributed online and informed consent was obtained from the children’s parents. A study-specific questionnaire on “children/adolescents’ screen use during the COVID-19 pandemic” had been pre-tested on a small scale, with parents reporting that the questionnaire was easy to understand and takes an average of 5–6 minutes to complete. Parents and/or children were required to complete the questionnaire, which included the following: child’s gender, date of birth, grade level, place of residence, the average household income, the main caregiver, any siblings, marriage and education level of the parents, average outdoor activity time (on weekdays and weekends, per day), and average screen exposure time of children during and before the COVID-19 (on weekdays and weekends, per day). An evaluator calculated the average daily outdoor activity time/screen time of the children using the following formula: Average daily outdoor activity time/screen time (hours) = [outdoor activity time/screen time per day on weekdays (hours) ×5+ outdoor activity time/screen time per day on weekends (hours) ×2]/7. The following questions are filled in for the last 2 months during COVID-19: types of children’s outdoor activities and screen time activity, types of electronic devices, screen time for education/learning (per day on average), restrictions on screen time, the reasons for screen time restriction, parental accompaniment during screen time, screen time of caregivers and siblings (per day on average), age at first screen exposure, use of electronic screens as a tool to occupy children, use of screen time as a reward or punishment, ownership of electronic equipment, screen time before going to bed, and sleep duration. Restrictions on screen time was divide into no restriction, partial restriction (sometimes parents can consult with children) and restriction (strict restrictions without any consultation).
We analyzed the basic demographic characteristics of the 496 participates and described the demographic characteristics of ASD/ADHD children and typically development (TD) children. We also described and compared the screen time and related factors for the total cohort and for TD children, ASD children, and ADHD children during the re-emergence of COVID-19. The risk factors that influenced children’ screen time during COVID-19 re-emergence were identified.
Statistical analysis
The Statistical Product and Service Solutions (SPSS) software, version 23.0 (SPSS for Windows, SPSS Inc., Chicago, IL, USA) was used to analyze all data. Continuous variables with normal distributions are represented as mean ± standard deviation (SD) and categorical variables are represented as frequencies (percentages). Screen time and outdoor activity time before and during COVID-19 re-emergence was compared using the paired t-test. The chi-square test was used to compare the rates between groups of categorical variables. Covariance analysis (covariant was “age”) was used to compare groups of continuous variables. Pearson correlation was used to test the correlation between continuous variables. Comparisons of children’s screen time between multiple subgroups were performed using analysis of variance (ANOVA). The significant factors in the univariate analysis (Pearson correlation and ANOVA) were included in the multiple linear regression model to analyze the risk factors of children’s screen time. A P value <0.05 was considered statistically significant.
Results
Basic characteristics of the participants
The basic characteristics of all participants are shown in Table 1. A total of 499 children were surveyed by online questionnaire, and 496 cases were available with complete data. Among them, 184 children had typical development (TD), 128 children presented with ASD and 134 children presented with ADHD. A total of 50 children presented with other developmental disorders, including global development delay, epilepsy, intellectual disabilities, or other emotional disorders such as depression or anxiety, and these were not included in the subgroup analysis due to the small numbers in each group. For all participants, there was a significant increase in screen time (t=−14.069, P<0.001) and a statistically significant decrease in outdoor activity time (t=14.774, P<0.001) during the re-emergence of COVID-19 compared to before. All other information is detailed in Table 2.
Table 1
| Variables | Total (N=496) | TD (N=184) | ASD (N=128) | ADHD (N=134) |
|---|---|---|---|---|
| Gender (N) | ||||
| Boy | 362 | 110 | 101 | 112 |
| Girl | 134 | 74 | 27 | 22 |
| Age (years), M (SD) | 6.64 (3.23) | 6.83 (3.37) | 4.34 (2.12) | 8.51 (2.46) |
| Grade level, n (%) | ||||
| Before kindergarten | 95 (19.2) | 15 (8.2) | 71 (55.5) | 0 |
| Kindergarten | 175 (35.3) | 87 (47.3) | 45 (35.2) | 27 (20.1) |
| Primary | 206 (41.5) | 72 (39.1) | 12 (9.4) | 99 (73.9) |
| Middle school | 20 (4.0) | 10 (5.4) | 0 | 8 (5.9) |
| Residence, n (%) | ||||
| City | 448 (90.3) | 172 (93.5) | 115 (89.8) | 115 (85.8) |
| Town/rural | 48 (9.7) | 12 (6.5) | 13 (10.2) | 19 (14.2) |
| Income/month (yuan), n (%) | ||||
| <5,000 | 125 (25.2) | 31 (16.8) | 42 (32.8) | 44 (32.8) |
| 5,000–10,000 | 203 (40.9) | 76 (41.3) | 51 (39.8) | 52 (38.8) |
| 10,000–30,000 | 138 (27.8) | 62 (33.7) | 33 (25.8) | 29 (21.6) |
| >30,000 | 30 (6.0) | 15 (8.2) | 2 (1.6) | 9 (6.7) |
| Caregiver, n (%) | ||||
| Parents | 326 (65.7) | 118 (64.1) | 77 (60.2) | 102 (76.1) |
| Parents and grandparents | 142 (28.6) | 57 (31.0) | 42 (32.8) | 25 (18.7) |
| Parents and nanny | 4 (0.8) | 1 (0.5) | 1 (0.8) | 1 (0.7) |
| Single parent | 19 (3.8) | 5 (2.7) | 7 (5.5) | 6 (4.5) |
| Grandparents | 5 (1.0) | 3 (1.6) | 1 (0.8) | 0 |
| Siblings, n (%) | ||||
| None | 353 (71.2) | 133 (72.3) | 93 (72.7) | 90 (67.2) |
| Older | 69 (13.9) | 18 (9.8) | 28 (21.9) | 15 (11.2) |
| Younger | 74 (14.9) | 33 (17.9) | 7 (5.5) | 29 (21.6) |
| Parents’ marital status, n (%) | ||||
| Married | 473 (95.4) | 177 (96.2) | 125 (97.7) | 126 (94) |
| Single parent | 23 (4.6) | 7 (3.8) | 3 (2.3) | 8 (6.0) |
| Maternal education, n (%) | ||||
| Primary | 74 (14.9) | 12 (6.5) | 21 (16.4) | 34 (25.4) |
| Middle | 82 (16.5) | 25 (13.6) | 26 (20.3) | 25 (18.7) |
| College | 248 (50.0) | 81 (44.0) | 70 (54.7) | 65 (48.5) |
| Graduate | 92 (18.5) | 66 (35.9) | 11 (8.6) | 10 (7.5) |
| Paternal education, n (%) | ||||
| Primary | 90 (18.1) | 17 (9.2) | 27 (21.1) | 39 (29.1) |
| Middle | 77 (15.5) | 23 (12.5) | 18 (14.1) | 28 (20.9) |
| College | 258 (52.0) | 96 (52.2) | 72 (56.3) | 61 (45.5) |
| Graduate | 71 (14.3) | 48 (26.1) | 11 (8.6) | 6 (4.5) |
Data are expressed as n (%) or M (SD). TD, typically developed; ASD, autism spectrum disorder; ADHD, attention deficit hyperactivity disorder; M, mean; SD, standard deviation.
Table 2
| Factors | Total | TD | ASD | TD vs. ASD | ADHD | TD vs. ADHD | ||
|---|---|---|---|---|---|---|---|---|
| F/χ2/Z | P | F/χ2/Z | P | |||||
| Screen time before epidemic (hours/d) | 0.94 (1.12) | 0.79 (0.76) | 1.00 (1.48) | 7.00 | 0.009 | 1.01 (1.13) | 4.762 | 0.030 |
| Screen time during epidemic (hours/d) | 2.01 (1.89) | 2.00 (1.97) | 1.45 (1.65) | 1.945 | 0.164 | 2.58 (1.82) | 0.150 | 0.699 |
| t | −14.069 | −9.248 | −4.485 | −9.465 | ||||
| P | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Outdoor activity time before epidemic (hours/d) | 0.78 (0.57) | 0.84 (0.58) | 0.81 (0.59) | 0.353 | 0.553 | 0.73 (0.53) | Z=−1.518 | 0.129 |
| Outdoor activity time during epidemic (hours/d) | 0.38 (0.35) | 0.36 (0.31) | 0.40 (0.43) | 1.099 | 0.295 | 0.39 (0.32) | Z=−1.104 | 0.270 |
| t | 14.774 | 10.773 | 7.139 | 7.381 | ||||
| P | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Screen time for education/learning (hours/d) | 1.08 (1.33) | 1.06 (1.32) | 0.40 (0.71) | 0.060 | 0.807 | 1.70 (1.45) | 1.465 | 0.227 |
| Screen time restriction, n (%) | ||||||||
| No restriction | 9 (1.8) | 4 (2.2) | 3 (2.3) | 4.959 | 0.084 | 1 (0.7) | 1.026 | 0.599 |
| Partial restriction | 286 (57.7) | 113 (61.4) | 63 (49.2) | 83 (61.9) | ||||
| Restriction | 201 (40.5) | 67 (36.4) | 62 (48.4) | 50 (37.3) | ||||
| The companionship during screen time, n (%) | ||||||||
| Accompanying with communication | 203 (40.9) | 80 (43.5) | 62 (48.4) | 2.941 | 0.230 | 44 (32.8) | 3.700 | 0.157 |
| Accompanying without communication | 87 (17.5) | 33 (17.9) | 14 (10.9) | 28 (20.9) | ||||
| No accompanying adult | 206 (41.5) | 71 (38.6) | 52 (40.6) | 62 (46.3) | ||||
| Screen time of parents (hours/d) | 2.86 (2.08) | 3.01 (2.16) | 2.41 (1.97) | 0.796 | 0.373 | 3.10 (2.02) | 0.051 | 0.821 |
| Screen time of siblings (hours/d) | 1.76 (2.14) | 1.52 (1.89) | 2.52 (2.59) | Z=−1.55 | 0.120 | 1.56 (2.09) | Z=−0.240 | 0.810 |
| Age of first screen exposure, n (%) | ||||||||
| 0–0.5 years | 20 (4.0) | 9 (4.9) | 9 (7.0) | 31.840 | <0.001 | 2 (1.5) | 8.046 | 0.090 |
| 0.5–1 year | 87 (17.5) | 25 (13.6) | 42 (32.8) | 12 (9.0) | ||||
| 1–2 years | 150 (30.2) | 55 (29.9) | 47 (36.7) | 32 (23.9) | ||||
| 2–3 years | 107 (21.5) | 37 (20.1) | 17 (13.3) | 38 (28.4) | ||||
| Over 3 years | 132 (26.6) | 58 (31.5) | 13 (10.2) | 50 (37.3) | ||||
| Frequency of screen exposure before bedtime, n (%) | ||||||||
| No exposure | 297 (59.9) | 120 (65.2) | 76 (59.4) | 1.428 | 0.699 | 70 (52.2) | 7.198 | 0.066 |
| 1–3 d/week | 92 (18.5) | 30 (16.3) | 26 (20.3) | 23 (17.2) | ||||
| 3–5 d/week | 35 (7.1) | 11 (6.0) | 7 (5.5) | 15 (11.2) | ||||
| 5–7 d/week | 72 (14.5) | 23 (12.5) | 19 (14.8) | 26 (19.4) | ||||
| Screen time before sleep (hours/d) | 0.29 (0.76) | 0.28 (0.76) | 0.19 (0.42) | 0.010 | 0.922 | 0.39 (0.88) | 0.421 | 0.517 |
| Sleep duration (hours) | 8.93 (1.13) | 8.94 (1.03) | 9.10 (1.36) | 0.001 | 0.995 | 8.81 (1.01) | <0.001 | 0.999 |
| Electronic nanny, n (%) | ||||||||
| Almost never | 193 (38.9) | 69 (37.5) | 42 (32.8) | 5.102 | 0.078 | 59 (44.0) | 2.874 | 0.238 |
| Sometimes | 265 (53.4) | 106 (57.6) | 71 (55.5) | 65 (48.5) | ||||
| Always | 38 (7.7) | 9 (4.9) | 15 (11.7) | 10 (7.5) | ||||
| As a reward or punishment, n (%) | ||||||||
| Almost never | 209 (42.1) | 77 (41.8) | 64 (50.0) | 2.070 | 0.355 | 42 (31.3) | 6.616 | 0.037 |
| Sometimes | 254 (51.2) | 98 (53.3) | 58 (45.3) | 77 (57.5) | ||||
| Always | 33 (6.7) | 9 (4.9) | 6 (4.7) | 15 (11.2) | ||||
| Ownership of independent electronic equipment, n (%) | ||||||||
| No | 309 (62.3) | 113 (61.4) | 101 (78.9) | 10.722 | 0.001 | 67 (50.0) | 4.112 | 0.043 |
| Yes | 187 (37.7) | 71 (38.6) | 27 (21.1) | 67 (50.0) | ||||
Data are expressed as n (%) or M (SD). TD, typically developed; ASD, autism spectrum disorder; ADHD, attention deficit hyperactivity disorder; M, mean; SD, standard deviation.
Risk factors for electronic screen time in children during the COVID-19 epidemic
The correlation analysis of screen time and related factors is shown in Table 3. The children were divided into multiple subgroups according to grade levels, parental education, ownership of independent electronic devices, degree of screen restriction, frequency of parental guidance during screen use, frequency of screen use as a form of babysitting, and frequency of screen use as a punishment or reward. The screen use of each subgroup is shown in Figure 1. The significant factors of univariate analysis were incorporated into the multiple linear regression model, and the rank data were transformed into dummy variables (the assignment of dummy variables is presented in Table 4). Regression analysis suggested that risk factors for children’s screen time during COVID-19 are age, degree of restriction, screen time before COVID-19, screen time for learning/education, screen time of siblings, and frequent use of electronic devices as a form of babysitting (see details in Table 4).
Table 3
| Factors | Age | Screen time before COVID-19 | Outdoor activity time | Screen time for learning/education | Screen time of parents | Screen time of siblings | Age of first exposure to screen |
|---|---|---|---|---|---|---|---|
| R | 0.519 | 0.224 | −0.033 | 0.587 | 0.416 | 0.313 | 0.192 |
| P | <0.001 | <0.001 | 0.467 | <0.001 | <0.001 | <0.001 | <0.001 |
COVID-19, coronavirus disease 2019.
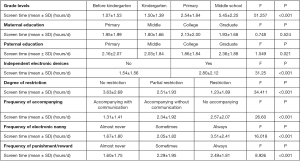
Table 4
| Factors | β | t | P | 95% CI |
|---|---|---|---|---|
| Age | 0.248 | 2.110 | 0.037 | 0.009, 0.285 |
| Screen time before COVID-19 | 0.191 | 2.889 | 0.005 | 0.084, 0.451 |
| Independent electronic devices (no =0, yes =1) | 0.067 | 1.098 | 0.274 | −0.211, 0.738 |
| Screen time for learning/education | 0.462 | 5.665 | <0.001 | 0.420, 0.871 |
| Screen time of parents | 0.081 | 1.179 | 0.240 | -0.049, 0.195 |
| Screen time of siblings | 0.181 | 2.728 | 0.007 | 0.045, 0.283 |
| Age of first exposure to screen | −0.061 | −0.938 | 0.350 | −0.361, 0.129 |
| Grade levels (before kindergarten =0) | ||||
| Kindergarten =1 (dummy variable) | 0.020 | 0.221 | 0.826 | −0.659, 0.824 |
| Primary school =1 (dummy variable) | −0.153 | −1.165 | 0.246 | −1.613, 0.417 |
| Middle school =1 (dummy variable) | 0.001 | 0.006 | 0.995 | −1.181, 1.822 |
| Degree of restriction (no restriction =0) | ||||
| Partial restriction =1 (dummy variable) | −0.600 | −2.429 | 0.017 | −4.488, −0.459 |
| Restriction =1 (dummy variable) | −0.688 | −2.675 | 0.008 | −4.989, −0.747 |
| Frequency of accompanying (no =0) | ||||
| Without communication =1 (dummy variable) | −0.059 | −0.924 | 0.357 | −0.845, 0.307 |
| With communication =1 (dummy variable) | 0.022 | 0.339 | 0.735 | −0.449, 0.634 |
| Frequency of electronic nanny (almost never =0) | ||||
| Sometimes =1 (dummy variable) | 0.131 | 1.833 | 0.069 | −0.041, 1.077 |
| Always =1 (dummy variable) | 0.200 | 2.859 | 0.005 | 0.389, 2.137 |
| Frequency of punishment/ reward (almost never =0) | ||||
| Sometimes =1 (dummy variable) | −0.033 | −0.477 | 0.634 | −0.650, 0.397 |
| Always =1 (dummy variable) | −0.036 | −0.561 | 0.576 | −1.206, 0.673 |
COVID-19, coronavirus disease 2019; CI, confidence interval.
Screen time in children with TD, ASD, and ADHD
We separately described the above content for TD children, ASD children, and ADHD children among all participants, and compared ASD children and ADHD children with TD children, respectively. The differences in the average daily screen use before and during COVID-19 re-emergence were statistically significant in TD children, ASD children, and ADHD children (Table 2). Before COVID-19, ASD children (F=7.00, P=0.009) and ADHD children (F=4.762, P=0.030) had longer screen time use compared to TD children, after controlling for age with statistical methods. However, no statistically significant differences were found during COVID-19 between the groups. The average duration of daily outdoor activity before and during COVID-19 were significantly different for TD children, ASD children, and ADHD children (Table 2). Compared with TD children, however, there was no statistically significant difference in outdoor activity time between TD children and ASD/ADHD children before COVID-19 nor during the COVID-19 pandemic.
Compared with TD children, children with ASD had a younger age of first screen exposure (χ2=31.84, P<0.001), and parents of ADHD children were more likely to use screens as a reward or punishment (χ2=6.616, P=0.037). During the COVID-19 pandemic, there was no statistical difference between TD children and ASD/ADHD children in terms of screen time for education/learning, screen time restriction, the companionship during screen time, screen time of parents, screen time of siblings, screen time before sleep, sleep duration, nor the frequency that screens were used as babysitters (Table 2).
Discussion
During the COVID-19 pandemic, time spent outdoors decreased and screen time increased
This study demonstrated that children spent less time outdoors and more time on electronic screens during the COVID-19 pandemic. The changes were seen in all children, whether in TD children, or ASD/ADHD children. Although the outbreak has been recurring for more than 2 years and China has experienced a very long period of regular prevention and control measure, our results are consistent with the earlier studies on COVID-19 and are not specific to China. A meta-analysis (30) showed that sedentary behavior in children was most affected by the COVID-19 pandemic (compared to adults and the elderly), with an increase in sedentary time of 159.5±142.6 min/day. A study of children aged 3–16 years in Spain (31) showed that preschoolers (ages 3 to 4) increased their screen exposure by 2.2 hours per day. An online survey at the beginning of COVID-19 in the United States reported that 211 parents of children aged 5–13 years perceived that children’s physical activity time had decreased, whereas children’s sedentary behavior had increased (32). Of all the sedentary behavior, children spent the most time watching television, videos, and movies. A total of 94% of parents interviewed reported that during the COVID-19 pandemic, children’s physical activity had decreased and 81% parents reported that children’s screen time had increased (33). Only about 3% of children met the recommended guidelines of 60 minutes of moderate-intensity physical activity per day during the COVID-19 pandemic (34). The situation is not exactly the same in different countries. In Sweden (35), physical activity, outdoor time, and screen time increased significantly among preschoolers, and this is attributed to the fact that Sweden did not close outdoor venues during this period. The change in outdoor hours may relate to national policy.
Governments, schools, health workers, sport professionals, and parents need to be aware of the grim situation and implement more effective interventions immediately to minimize the negative impact of the COVID-19 pandemic on the health of children and adolescents (36). It is recommended that governments develop policies to promote healthy lifestyles and screen use (33,37).
Risk factors of children/adolescents’ screen time use during the COVID-19 pandemic
Our study suggested that during the COVID-19 pandemic, prolonged screen time use by children/adolescents was associated with older age, longer pre-COVID-19 screen time, longer screen time used for learning/education, longer screen time of siblings, decreased parental restrictions on screen time, and the frequency with which parents used screen devices as babysitters.
Early in the pandemic, a study was conducted in Turkey (38) on the relationship between parenting practices and screen time in children during the COVID-19 pandemic. Results showed that age, household income, mother’s employment status, family’s rules about screen time, and inconsistent parenting practices were defined as significant predictors in children’s screen time. This is partly consistent with our results, which also found that age and family rules (the restrictions imposed by parents, and the frequency of using screen devices as babysitters) were associated with children’s screen time. Many studies have also confirmed that the establishment of family screen rules can limit children’s screen time (39,40), but the existence of rules not sufficient if there is inconsistent application of the rules (38), or if parents use electronic screens to occupy the children (41).
Some studies (42,43) have found that children whose parents have more screen time also have more screen time, but our results suggested that electronic screen time of siblings is more likely to influence children’s electronic screen time. Durham (44) reported a significant relationship between the presence of a sibling and children’s screen time. This situation may be more obvious during the COVID-19 pandemic. Siblings tend to demand extra screen time to achieve what they perceive as “fairness”. This may directly expose child to additional screen time, if it is in the form of television or on a large screen. The study did not investigate age of siblings. This may be a limitation of our study. Differences in screen activity may be due to differences in sibling age, which may have different effects on participants' screen time. In addition, we did not analyze differences in screen time between children with and without siblings to see if the absence of siblings might be a protective factor for screen time. Our study also suggested that age and screen time used for learning/education are also risk factors for children’s screen time during the COVID-19 epidemic. This appears to be a unique situation during the pandemic when children needed to use electronic devices increasingly with age and grade to participate in online lessons, complete homework, complete group activities, interact with teachers, and other activities through mediums such as Zoom or Tencent Meeting (45). Although these online resources were convenient and satisfied a need during the pandemic (46), we cannot ignore the adverse effects on children and adolescents. Another interesting issue is that numerous studies have found that less time spent in physical activity is a risk factor for more screen time in children (47-49), but our study did not suggest this. Implementation of COVID-19 pandemic policies has limited outdoor activity time for all children. We hypothesize that other non-sedentary behaviors such as housework at home, strength training at home, and physical activity at home may still influence children’s screen time. However, this report did not investigate children’s indoor physical activity, which is a limitation of this study.
A comparison of screen time in children with TD, ASD, and ADHD
The results herein suggested that both ASD and ADHD children had longer screen time use than TD children before the pandemic of COVID-19, however, there was no statistical difference during the COVID-19 pandemic.
Many studies (14,50,51) have found that children with ASD had higher screen time even when there is no COVID-19 epidemic, and this is not a novel topic. Cardy’s study (28) reported that, compared to the community sample, the ASD group had a significantly higher screen time use before and during the COVID-19 pandemic school closures. Our study did not find that children with ASD had more screen time during the pandemic than children with TD, but found that TD children had more screen time on average (2 hours) than children with ASDs (1.45 hours), although this was not statistically significant. However, the average age of the ASD children in this study was over 11 years old, while the ASD children we included were younger with an average age of 4.34 years old, and more than 90% of the ASD children did not attend primary school. Another important point to note is that these parents have received systematic parent training programs (52) in our department and have a certain understanding of screen exposure and children’s development. Parent training programs focus on the education of parents, family support, family interaction and play programs, with an emphasis on the ecological environment of early childhood development in ASD children. It should be added that the statistical effect may be affected by the large age gap in the sample, because the ASD group is too young to be likely to have screen time of learning. ASD children are more likely to prefer stereotypical screen content that appeals to them, rather than learning content. And the screen time of the typical children may have been academic. These may have contributed to some extent to our results, which need to be confirmed by further research.
Longer screen time in children with ADHD has also been reported (17,53), and screen time for ADHD has increased significantly during COVID-19 (54). These are all consistent with our research. However, we found no statistical difference in screen time between ADHD children and TD children during the COVID-19 epidemic. Since ADHD children suffer from an executive function deficit (55), they are less able to control their own behavior than children of the same age. During the pandemic, children had more autonomous time, and children with less self-control were more likely to choose screen activities that appealed to children. From this point of view, our results which found no difference in screen time between children with ADHD and those with TD seemed difficult to explain. However, similar to the ASD children, the parents of the enrolled ADHD children had undergone a parent training program. This suggested a possible role of parent training programs in the management of children’s electronic screen time, which may be examined further in our future work.
Limitation
This was a cross-sectional study, and future studies are expected to establish cohorts to explore the development of children growing up with the COVID-19 virus. In the procedure of data collection, parent surveys are limited by recall bias, especially for the earlier data. Therefore, future research tends to choose more accurate methods. Children with developmental disabilities included in our study had parents who participated in our training program, and thus, there is a large sampling bias among the children participating in the survey. The majority of ASD children in this cohort were preschoolers, while the majority of ADHD children were school-age children. This may have significantly impacted some of the comparisons, especially since screen time seems to be associated with age. Further research should be conducted using comparable ages and a larger sample size to verify these results.
Conclusions
This is the first study to compare the screen time of children with TD and children with developmental disabilities during and before COVID-19 pandemic. There are great challenges surrounding the use of screens by children during the COVID-19 pandemic. Children’s screen time increased and outdoor activities decreased significantly. Age, pre-COVID-19 screen time, screen time used for learning/education, screen time of siblings, and parental use of screen devices as babysitters were identified as risk factors for screen time during COVID-19, while parental restrictions on screen use was a protective factor. The screen time of ASD and ADHD children was significantly longer than TD children before COVID-19 pandemic. It is imperative that we focus on managing children’s screen time and promoting healthier lifestyles, including children with typical development and those with developmental disorders.
Acknowledgments
The authors wish to thank all the families who contributed their time to this study.
Funding: This work was supported by The Health Science and Technology Capacity Improvement Project of Jilin Province (No. 2022LC104), and the Talent Reserve Plan of the First Hospital of Jilin University (No. 04027900001).
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-162/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-162/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-162/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-162/coif). All authors report that this study was supported by the Health Science and Technology Capacity Improvement Project of Jilin Province (No. 2022LC104) and the Talent Reserve Plan of the First Hospital of Jilin University (No. 04027900001). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the First Hospital of Jilin University (No. 21K096-001) and informed consent was taken from all the children’s parents throughout the internet.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. Lancet 2020;395:470-3. [Crossref] [PubMed]
- Pan A, Liu L, Wang C, et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020;323:1915-23. [Crossref] [PubMed]
- Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020;585:410-3. [Crossref] [PubMed]
- Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 2020;27:taaa020. [Crossref] [PubMed]
- Wong ASK. Prolonged Screen Exposure During COVID-19-The Brain Development and Well-Being Concerns of Our Younger Generation. Front Public Health 2021;9:700401. [Crossref] [PubMed]
- Singh S, Roy D, Sinha K, et al. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res 2020;293:113429. [Crossref] [PubMed]
- Guellai B, Somogyi E, Esseily R, et al. Effects of screen exposure on young children's cognitive development: A review. Front Psychol 2022;13:923370. [Crossref] [PubMed]
- Media and Young Minds. Pediatrics 2016;138:e20162591. [Crossref] [PubMed]
- Wang J, Li Y, Musch DC, et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol 2021;139:293-300. [Crossref] [PubMed]
- Alonso-Martínez AM, Ramírez-Vélez R, García-Alonso Y, et al. Physical Activity, Sedentary Behavior, Sleep and Self-Regulation in Spanish Preschoolers during the COVID-19 Lockdown. Int J Environ Res Public Health 2021;18:693. [Crossref] [PubMed]
- Guo YF, Liao MQ, Cai WL, et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci Rep 2021;11:8529. [Crossref] [PubMed]
- Heffler KF, Oestreicher LM. Causation model of autism: Audiovisual brain specialization in infancy competes with social brain networks. Med Hypotheses 2016;91:114-22. [Crossref] [PubMed]
- Westby C. Screen Time and Children with Autism Spectrum Disorder. Folia Phoniatr Logop 2021;73:233-40. [Crossref] [PubMed]
- Dong HY, Wang B, Li HH, et al. Correlation Between Screen Time and Autistic Symptoms as Well as Development Quotients in Children With Autism Spectrum Disorder. Front Psychiatry 2021;12:619994. [Crossref] [PubMed]
- Krupa M, Boominathan P, Ramanan PV, et al. Relationship Between Screen Time and Mother-Child Reciprocal Interaction in Typically Developing Children and Children with Autism Spectrum Disorders. Indian J Pediatr 2019;86:394. [Crossref] [PubMed]
- Kushima M, Kojima R, Shinohara R, et al. Association Between Screen Time Exposure in Children at 1 Year of Age and Autism Spectrum Disorder at 3 Years of Age: The Japan Environment and Children's Study. JAMA Pediatr 2022;176:384-91. [Crossref] [PubMed]
- Lingineni RK, Biswas S, Ahmad N, et al. Factors associated with attention deficit/hyperactivity disorder among US children: results from a national survey. BMC Pediatr 2012;12:50. [Crossref] [PubMed]
- Ceranoglu TA. Inattention to Problematic Media Use Habits: Interaction Between Digital Media Use and Attention-Deficit/Hyperactivity Disorder. Child Adolesc Psychiatr Clin N Am 2018;27:183-91. [Crossref] [PubMed]
- Zimmerman FJ, Christakis DA. Associations between content types of early media exposure and subsequent attentional problems. Pediatrics 2007;120:986-92. [Crossref] [PubMed]
- Tang S, Xiang M, Cheung T, et al. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J Affect Disord 2021;279:353-60. [Crossref] [PubMed]
- Xie X, Xue Q, Zhou Y, et al. Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr 2020;174:898-900. [Crossref] [PubMed]
- Werling AM, Walitza S, Drechsler R. Impact of the COVID-19 lockdown on screen media use in patients referred for ADHD to child and adolescent psychiatry: an introduction to problematic use of the internet in ADHD and results of a survey. J Neural Transm (Vienna) 2021;128:1033-43. [Crossref] [PubMed]
- Mesce M, Ragona A, Cimino S, et al. The impact of media on children during the COVID-19 pandemic: A narrative review. Heliyon 2022;8:e12489. [Crossref] [PubMed]
- Eirich R, McArthur BA, Anhorn C, et al. Association of Screen Time With Internalizing and Externalizing Behavior Problems in Children 12 Years or Younger: A Systematic Review and Meta-analysis. JAMA Psychiatry 2022;79:393-405. [Crossref] [PubMed]
- Li X, Vanderloo LM, Keown-Stoneman CDG, et al. Screen Use and Mental Health Symptoms in Canadian Children and Youth During the COVID-19 Pandemic. JAMA Netw Open 2021;4:e2140875. [Crossref] [PubMed]
- Werling AM, Walitza S, Gerstenberg M, et al. Media use and emotional distress under COVID-19 lockdown in a clinical sample referred for internalizing disorders: A Swiss adolescents' perspective. J Psychiatr Res 2022;147:313-23. [Crossref] [PubMed]
- Berard M, Peries M, Loubersac J, et al. Screen time and associated risks in children and adolescents with autism spectrum disorders during a discrete COVID-19 lockdown period. Front Psychiatry 2022;13:1026191. [Crossref] [PubMed]
- Cardy RE, Dupuis A, Anagnostou E, et al. Characterizing Changes in Screen Time During the COVID-19 Pandemic School Closures in Canada and Its Perceived Impact on Children With Autism Spectrum Disorder. Front Psychiatry 2021;12:702774. [Crossref] [PubMed]
- Kaku SM, Chandran S, Roopa N, et al. Coping with autism during lockdown period of the COVID-19 pandemic: A cross-sectional survey. Indian J Psychiatry 2021;63:568-74. [Crossref] [PubMed]
- Runacres A, Mackintosh KA, Knight RL, et al. Impact of the COVID-19 Pandemic on Sedentary Time and Behaviour in Children and Adults: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health 2021;18:11286. [Crossref] [PubMed]
- López-Bueno R, López-Sánchez GF, Casajús JA, et al. Health-Related Behaviors Among School-Aged Children and Adolescents During the Spanish Covid-19 Confinement. Front Pediatr 2020;8:573. [Crossref] [PubMed]
- Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020;20:1351. [Crossref] [PubMed]
- Guan H, Okely AD, Aguilar-Farias N, et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolesc Health 2020;4:416-8. [Crossref] [PubMed]
- Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act 2020;17:85. [Crossref] [PubMed]
- Delisle Nyström C, Alexandrou C, Henström M, et al. International Study of Movement Behaviors in the Early Years (SUNRISE): Results from SUNRISE Sweden's Pilot and COVID-19 Study. Int J Environ Res Public Health 2020;17:8491. [Crossref] [PubMed]
- Bates LC, Zieff G, Stanford K, et al. COVID-19 Impact on Behaviors across the 24-Hour Day in Children and Adolescents: Physical Activity, Sedentary Behavior, and Sleep. Children (Basel) 2020;7:138. [Crossref] [PubMed]
- Margaritis I, Houdart S, El Ouadrhiri Y, et al. How to deal with COVID-19 epidemic-related lockdown physical inactivity and sedentary increase in youth? Adaptation of Anses' benchmarks. Arch Public Health 2020;78:52. [Crossref] [PubMed]
- Ozturk Eyimaya A, Yalçin Irmak A. Relationship Between Parenting Practices and Children's Screen Time During the COVID-19 Pandemic in Turkey. J Pediatr Nurs 2021;56:24-9. [Crossref] [PubMed]
- Hu BY, Johnson GK, Wu H. Screen time relationship of Chinese parents and their children. Children and Youth Services Review 2018;94:659-69. [Crossref]
- Xu H, Wen LM, Rissel C. Associations of parental influences with physical activity and screen time among young children: a systematic review. J Obes 2015;2015:546925. [Crossref] [PubMed]
- Samaha M, Hawi NS. Associations between screen media parenting practices and children’s screen time in Lebanon. Telematics and Informatics 2017;34:351-8. [Crossref]
- Jago R, Sebire SJ, Edwards MJ, et al. Parental TV viewing, parental self-efficacy, media equipment and TV viewing among preschool children. Eur J Pediatr 2013;172:1543-5. [Crossref] [PubMed]
- Jiang XX, Hardy LL, Ding D, et al. Recreational screen-time among Chinese adolescents: a cross-sectional study. J Epidemiol 2014;24:397-403. [Crossref] [PubMed]
- Durham K, Wethmar D, Brandstetter S, et al. Digital Media Exposure and Predictors for Screen Time in 12-Month-Old Children: A Cross-Sectional Analysis of Data From a German Birth Cohort. Front Psychiatry 2021;12:737178. [Crossref] [PubMed]
- Camargo CP, Tempski PZ, Busnardo FF, et al. Online learning and COVID-19: a meta-synthesis analysis. Clinics (Sao Paulo) 2020;75:e2286. [Crossref] [PubMed]
- Wijesooriya NR, Mishra V, Brand PLP, et al. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev 2020;35:38-42. [Crossref] [PubMed]
- Wu XY, Tao SM, Zhang SC, et al. Analysis on risk factors of screen time among Chinese primary and middle school students in 12 provinces. Zhonghua Yu Fang Yi Xue Za Zhi 2016;50:508-13. [PubMed]
- Gingold JA, Simon AE, Schoendorf KC. Excess screen time in US children: association with family rules and alternative activities. Clin Pediatr (Phila) 2014;53:41-50. [Crossref] [PubMed]
- Carlson SA, Fulton JE, Lee SM, et al. Influence of limit-setting and participation in physical activity on youth screen time. Pediatrics 2010;126:e89-96. [Crossref] [PubMed]
- Chonchaiya W, Nuntnarumit P, Pruksananonda C. Comparison of television viewing between children with autism spectrum disorder and controls. Acta Paediatr 2011;100:1033-7. [Crossref] [PubMed]
- Healy S, Garcia JM, Haegele JA. Environmental Factors Associated with Physical Activity and Screen Time Among Children With and Without Autism Spectrum Disorder. J Autism Dev Disord 2020;50:1572-9. [Crossref] [PubMed]
- Subspecialty Group of Developmental and Behavioral Pediatrics. the Society of Pediatrics, Chinese Medical Association; Subspecialty Group of Child Health Care, the Society of Pediatrics, Chinese Medical Doctor Association. Expert consensus on family intervention for young children with autism spectrum disorder in China. Zhonghua Er Ke Za Zhi 2022;60:395-400.
- Tandon PS, Sasser T, Gonzalez ES, et al. Physical Activity, Screen Time, and Sleep in Children With ADHD. J Phys Act Health 2019;16:416-22. [Crossref] [PubMed]
- Shah R, Raju VV, Sharma A, et al. Impact of COVID-19 and Lockdown on Children with ADHD and Their Families-An Online Survey and a Continuity Care Model. J Neurosci Rural Pract 2021;12:71-9. [Crossref] [PubMed]
- Barkley RA. Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. J Clin Child Adolesc Psychol 2013;42:161-73. [Crossref] [PubMed]
(English Language Editor: J. Teoh)


