
The risk factors for negative emotions in parents of children with bacterian vulvovaginitis and its impact on prognosis: a retrospective cohort study
Highlight box
Key findings
• Parental negative emotions have a significant impact on the prognosis of children with vulvovaginitis. We should pay attention to the psychological guidance to the parents, so that they can actively cooperate with the treatment and accelerate the recovery of the children.
What is known and what is new?
• Parental negative emotions (such as anxiety and depression) have lots of independent risk factors.
• Negative emotions of parents have a significant impact on the prognosis of children with vulvovaginitis.
What is the implication, and what should change now?
• In clinical treatment, we should not only pay attention to the physical and mental health of the patients, but also focus on psychological guidance to the parents of the children, so that they can actively cooperate with the treatment and accelerate the recovery of the children.
Introduction
Vulvovaginitis is an inflammatory disease of the vulva and vaginal tissues caused by pathogenic infections such as bacteria, fungi, and viruses, and it is a common condition that damage women’s physical and psychological health (1). Clinical symptoms usually include pruritus, pain, dysuria, ulcerations, increased vaginal secretions, and odor (2). If left untreated, it can cause upstream infection of bacteria in the vagina, resulting in gynecological diseases such as cervicitis, and some inflammatory diseases can also be linked to other organs, resulting in diseases of the reproductive organs such as pelvic inflammatory disease and adnexitis. Severe cases of vaginitis can lead to infertility in women, with serious consequences. Due to the lack of effective treatment for this disease, experts emphasize the prevention of infection through regular hand washing, attention to perineal hygiene, and the maintenance of healthy habits (3-5). There is the evidence that the incidence of recurrence is higher if the hygiene recommendations are not followed (6).
In recent years, the incidence of vulvovaginitis in children has increased year by year with the increased occurrence of precocious puberty, becoming the most common gynecologic disease in prepubertal girls (7), and the evidence suggests that 4 out of 10 young girls exhibit symptoms of vulvovaginitis (8). Chinese and international studies have shown that the percentage of children with vulvovaginitis in pediatric gynecology clinics can exceed 60% (9). The reasons why prepubertal girls exhibit vulnerability to vulvovaginitis are determined by their anatomy and physiological characteristics, for example, the proximity of the vagina to the anus and the lack of hygiene in young children may lead to the entry of fecal flora into the vagina. In addition, the lack of estrogen leads to a thinner epithelium and a low number of lactobacilli, which creates a more neutral pH compared to the post-pubertal vagina (10), which leads to an easy survival of other harmful flora. Further, the underdevelopment of the labia in children and the lack of protection provided by the pubic hair and lipid pads leads to a greater vulnerability to trauma in affected children (11), which leads to the development of infections. Vulvovaginitis includes both infectious and non-infectious etiologies. Approximately 75% of vaginitis cases before puberty are non-specific vaginitis (12). In cases of nonspecific vaginitis, decreased mucosal integrity and physicochemical changes caused by local irritants or endogenous vaginal flora are the main causes (13). Many scientists believe that tight clothing and cleaning products may be associated with the progression of nonspecific vaginitis (14-16). Therefore, the development of vulvovaginitis in children may be the result of the interaction of various factors.
Studies (17,18) have found that vulvovaginitis can have a similar impact on children and parents as other chronic diseases. Vulvovaginitis in children is often considered an embarrassing and taboo subject by parents or families, who often consider the disease to be private and shameful, and the recurrence of the condition is often a source of great concern for parents, so this frequently leads to the development of negative emotions such as anxiety and depression in the families of children with vulvovaginitis. However, there is a paucity of research on the risk factors for negative parental emotions and it is not known whether negative emotions have an impact on the prognosis of the child. Therefore, this study aimed to analyze the clinical characteristics of children with vulvovaginitis and the risk factors of negative parental emotions on the prognosis, in order to improve the prognosis of patients, reduce negative parental emotions, and develop the quality of family life. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-183/rc).
Methods
Research participants
A total of 350 children with vulvovaginitis treated at the Affiliated Hospital of Jiangnan University from April 2017 to April 2022 were retrospectively admitted to this study.
The inclusion criteria were as follows: (I) patients aged <12 years and female; (II) meeting the diagnostic criteria for bacterial vulvovaginitis; (III) good medication compliance (Figure 1).
The exclusion criteria were as follows: (I) patients aged ≥12 years or male; (II) involvement of recurrent infections, vaginal foreign bodies, or sexual abuse; (III) other causes of vulvovaginitis; (IV) parents with pre-existing mental illness; (V) having congenital vulvovaginal malformation (Figure 1).
The purpose of this cross-sectional study was to investigate the relationship between parents’ anxiety and depression and the prognosis of children. According to our previous research and related literature reports, the incidence rates of anxiety and depression in parents of children with bacterial vaginitis are about 40% and 30%, respectively. The allowable error is 2.5%, the confidence level is 1-α=0.95, and N2/N1 is about 0.9. The sample size to be investigated was calculated using PASS 15 software, N1=117 cases and N2=105 cases. Assuming that the non-response rate of the subjects is 10%, the sample size is required N=247 (222/0.9) cases. Assuming that the qualified rate of the questionnaire is 90%, the total sample size is N=274 (247/0.9) cases. The general rule of logistic linear regression requires that the ratio of the number of items to the sample size be 1:5 to 1:10. Therefore, the initial sample size of the research cohort in this study was 350 patients, of which, 47 patients were excluded. Finally, 303 pediatric patients with vulvovaginitis were enrolled in this study according to the inclusion and exclusion criteria.
All patients and their parents were given a face-to-face questionnaire 2 weeks after receiving treatment.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Affiliated Hospital of Jiangnan University board (No. KYLC2017031) and informed consent was taken from all the patients’ guardians.
General information questionnaire
The general information questionnaire included demographic data (such as parental age, marital status, monthly household income, address, parental occupation, education level, whether the child was the only child or premature, whether the child had congenital diseases, and the child’s age) and clinical data (such as vulvar pruritus, increased secretions, vulvar ulcerations, dysuria, frequent urination, painful urination, labia minora adhesion, and the presence of odor).
Diagnosis
Bacterial vaginitis is characterized by itching, pain and purulent discharge from the vulva, along with a peculiar odor. Physical examination reveals symptoms such as congestion and oedema of the vulva, or the formation of ulcers, flaky eczema, erosions, and congestion of the vestibular or vaginal mucosa. Asepsis is ensured throughout and the specimen sent for examination shows a bacterial infection.
Treatment
(I) Health education: Educate the child and the child’s family about the causes of vaginitis, risk factors, precautions, prevention and daily care. (II) Drug treatment: Depending on the condition, the child should be given amoxicillin clavulanic acid potassium tablets for oral use or cefotaxime sodium for injection by intravenous infusion, or erythromycin dry suspension or azithromycin dry suspension for β-lactam allergy. The child’s medication regimen will be adjusted based on the results of bacterial cultures and drug sensitivity tests.
Negative emotion assessment
Negative emotions of parents of children with bacterial vaginitis in this study were assessed by self-rating anxiety scale (SAS) and self-rating depression scale (SDS). The total score of SAS was 100 points: <50 points indicated no anxiety or depression, 50–70 points indicated mild anxiety or depression, 71–90 points indicated moderate anxiety or depression, and >90 points indicated severe anxiety or depression. An SDS score >52 was used as the evaluation criterion. An SDS ≥53 was classified as depression, 53–62 as mild depression, 63–72 as moderate depression, and >72 as severe depression. A higher score indicated more severe anxiety or depression. If either the SAS score of the patient was greater than 50 points or SDS score was greater than 52 points during the treatment, the patient was defined as having negative emotions. And the Cronbach’s α coefficients are above 0.75.
Prognostic evaluation
Patients were evaluated prognostically based on the relief time of clinical symptoms (such as pain, vulvar pruritus, purulent discharge, ulceration, odor) and the rate of recovery within 2 weeks, as well as the clearance rate of urinalysis.
The follow-up was conducted by telephone, e-mail, and outpatient review. Depending on the age of the patient, follow-up methods can be provided by the patient himself or the patient’s guardian to improve the accuracy of follow-up results. The last follow-up occurred in April 2022.
All treatments were based on the guidelines for diagnosis and treatment of bacterial vaginosis.
Statistical analysis
The results of each scale were subjected to score conversion and statistical analysis using the software SPSS 26.0 (IBM Corp., Armonk, NY, USA), with measured data expressed as mean and standard deviation, and count data expressed as frequencies and percentages. Statistical analysis between groups was performed using t-test and chi-squared test, and logistic regression analysis was used for factors influencing parental anxiety and depression and the prognosis of patients. A 2-sided P value <0.05 was considered statistically significant.
Results
Baseline data
The baseline characteristics of patients are shown in Table 1. A total of 303 children with vaginitis were included in this study, with an average age of 6.18±2.39 years. A total of 109 patients were <6 years old and 194 patients were ≥6 years old. Among them, 218 patients were the only child and 85 patients were not the only child. A total of 69 patients were preterm infants and 234 patients were non-preterm infants. A total of 87 patients had congenital diseases and 216 patients had no congenital diseases. The mean age of the parents was 28.40±3.88 years, including 203 parents <30 years old, 100 parents ≥30 years old, 106 parents whose occupation was related to medicine, and 197 parents whose occupation was not related to medicine.
Table 1
| Item | N (%) | SDS | SAS | |||||
|---|---|---|---|---|---|---|---|---|
| Scores, mean ± SD |
t/F | P value | Scores, mean ± SD |
t/F | P value | |||
| Age (year) | 1.243 | 0.215 | 1.732 | 0.084 | ||||
| <30 | 203 (67.00) | 51.00±8.41 | 49.79±9.82 | |||||
| ≥30 | 100 (33.00) | 49.72±8.57 | 47.76±9.09 | |||||
| Spouse or not | 4.471 | 0.000 | 2.453 | 0.015 | ||||
| Have spouse | 264 (87.13) | 49.67±7.94 | 48.60±9.52 | |||||
| No spouse | 39 (12.87) | 56.77±9.44 | 52.62±9.70 | |||||
| Monthly household income (yuan) | 2.280 | 0.023 | 2.330 | 0.020 | ||||
| <5,000 | 176 (58.09) | 51.52±8.33 | 50.20±9.57 | |||||
| ≥5,000 | 127 (41.91) | 49.28±8.52 | 47.61±9.52 | |||||
| Occupation | 2.194 | 0.029 | 2.047 | 0.041 | ||||
| Medical related | 106 (34.98) | 49.19±7.72 | 47.58±9.59 | |||||
| Non-medical related | 197 (65.02) | 51.33±8.78 | 49.94±9.55 | |||||
| Level of education | 0.660 | 0.510 | 0.430 | 0.667 | ||||
| Below bachelor degree | 129 (42.57) | 50.96±9.06 | 49.40±9.90 | |||||
| Bachelor degree or above | 174 (57.43) | 50.30±8.02 | 48.91±9.42 | |||||
| Address | 2.028 | 0.043 | 2.124 | 0.034 | ||||
| City | 136 (44.88) | 51.67±8.19 | 50.41±9.83 | |||||
| Rural | 167 (55.12) | 49.69±8.62 | 48.07±9.34 | |||||
| The only child or not | 0.790 | 0.430 | 0.756 | 0.450 | ||||
| Yes | 218 (71.49) | 50.82±8.45 | 48.86±9.93 | |||||
| No | 85 (38.51) | 49.96±8.54 | 49.79±8.78 | |||||
| Premature infant or not | 0.419 | 0.676 | 1.315 | 0.190 | ||||
| Yes | 69 (22.77) | 50.96±7.94 | 47.78±10.10 | |||||
| No | 234 (77.23) | 50.47±8.64 | 49.51±9.46 | |||||
| Congenital disease | 2.210 | 0.029 | 2.228 | 0.027 | ||||
| Yes | 87 (28.71) | 52.34±9.08 | 51.05±9.72 | |||||
| No | 216 (71.29) | 49.87±8.13 | 48.34±9.49 | |||||
| Child’s age (year) | 0.551 | 0.582 | 2.294 | 0.022 | ||||
| <6 | 109 (35.97) | 50.95±9.27 | 50.80±9.26 | |||||
| ≥6 | 194 (64.03) | 50.37±8.01 | 48.18±9.71 | |||||
SDS, Self-rating Depression Scale; SAS, Self-rating Anxiety Scale; SD, standard deviation.
Negative emotions in parents of children with vulvovaginitis
There were significant differences in SAS scores and SDS scores among children with congenital diseases, single parent families, parents’ occupation, family monthly income, and address. There were significant differences in the SAS scores among children of different ages (P<0.05; Table 1, Figure 2).

Analysis between clinical manifestations of children and parents’ negative emotions
The binary logistics regression analysis showed that vulva itching, secretion increase, and the production of unpleasant odor were the common independent factors causing anxiety and depression in the parents. The furuncle of vulvar ulcer and the adhesion of labia minora were independent factors causing anxiety of parents (P<0.05; Table 2, Figure 3A); Dysuria, frequency and pain of urination in children were independent factors causing parental depression (P<0.05; Table 3, Figure 3B).
Table 2
| Related factors | B | SE | Wald | P value | OR | 95% CI |
|---|---|---|---|---|---|---|
| Vulvar pruritus | 0.509 | 0.257 | 3.919 | 0.048 | 1.664 | 2.755–1.005 |
| Increased secretion | 0.828 | 0.261 | 10.099 | 0.001 | 2.289 | 3.816–1.374 |
| Dysuria | 0.475 | 0.266 | 3.202 | 0.074 | 1.609 | 2.707–0.956 |
| Frequent urination | 0.373 | 0.262 | 2.024 | 0.155 | 1.452 | 2.428–0.869 |
| Painful urination | 0.479 | 0.267 | 3.226 | 0.072 | 1.615 | 2.724–0.957 |
| Hyperemia and edema of the vulva | 0.484 | 0.260 | 3.481 | 0.062 | 1.623 | 2.699–0.976 |
| Furuncle and swelling of vulvar ulcer | 0.605 | 0.268 | 5.074 | 0.024 | 1.831 | 3.099–1.082 |
| Attached labia minora | 1.130 | 0.321 | 12.415 | 0.000 | 3.096 | 5.806–1.651 |
| Malodor | 0.540 | 0.269 | 4.030 | 0.045 | 1.716 | 2.909–1.013 |
SAS, Self-rating Anxiety Scale; CI, confidence interval; OR, odds ratio; SE, standard error; B, beta.
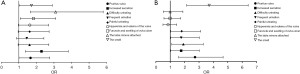
Table 3
| Related factors | B | SE | Wald | P value | OR | 95% CI (higher to lower) |
|---|---|---|---|---|---|---|
| Vulvar pruritus | 1.001 | 0.276 | 13.185 | 0.000 | 2.722 | 4.673–1.585 |
| Increased secretion | 0.564 | 0.276 | 4.185 | 0.041 | 1.758 | 3.019–1.024 |
| Dysuria | 0.648 | 0.278 | 5.433 | 0.020 | 1.911 | 3.294–1.109 |
| Frequent urination | 0.566 | 0.276 | 4.208 | 0.040 | 1.761 | 3.024–1.026 |
| Painful urinating | 0.586 | 0.279 | 4.407 | 0.036 | 1.797 | 3.105–1.040 |
| Hyperemia and edema of the vulva | −0.167 | 0.273 | 0.373 | 0.541 | 0.846 | 1.446–0.495 |
| Furuncle and swelling of vulvar ulcer | −0.015 | 0.285 | 0.003 | 0.958 | 0.985 | 1.721–0.564 |
| Attached labia minora | −0.010 | 0.328 | 0.001 | 0.976 | 0.990 | 1.882–0.521 |
| Malodor | 1.310 | 0.280 | 21.896 | 0.000 | 3.705 | 6.416–2.141 |
SDS, Self-rating Depression Scale; SE, standard error; B, beta; OR, odds ratio; CI, confidence interval.
Analysis between children’s prognosis and parents’ negative emotions
Parents’ negative emotions can significantly affect the prognosis of children. The t-test showed that parents’ anxiety could significantly prolong the relief time of pain, vulvar pruritus, purulent secretions, and odor, whereas parents’ depression could significantly prolong the relief time of pain, vulvar pruritus, and vulvar ulcers (P<0.05; Table 4). Binary logistics regression analysis showed that clinical symptoms such as pain, vulvar pruritus, increased purulent secretions, and malodor were also independent influencing factors for parental anxiety (P<0.05; Table 5, Figure 4A); the symptoms of pain and vulvar ulcer in children were independent factors of depression in parents (P<0.05; Table 6, Figure 4B). Chi-squared test analysis showed that parents with anxiety and depression had significant differences in the 2-week recovery rate and urine negative rate of children (P<0.05; Table 7). These results indicate that anxiety or depression in parents can significantly affect the prognosis of children.
Table 4
| Items | Pain | Vulvar pruritis | Purulent secretions | Furuncle and swelling of vulvar ulcer | Malodor |
|---|---|---|---|---|---|
| Depression | |||||
| Yes, mean ± SD | 10.91±4.465 | 9.31±3.645 | 10.23±4.358 | 8.92±3.408 | 11.44±4.791 |
| No, mean ± SD | 9.64±3.853 | 8.39±3.840 | 10.22±4.154 | 7.99±2.961 | 11.03±4.331 |
| t/F | 2.578 | 2.036 | 0.016 | 2.470 | 0.762 |
| P value | 0.010 | 0.043 | 0.987 | 0.014 | 0.446 |
| Anxiety | |||||
| Yes, mean ± SD | 10.84±4.441 | 9.91±4.029 | 11.16±4.535 | 8.64±3.465 | 12.33±4.854 |
| No, mean ± SD | 9.48±3.737 | 7.74±3.299 | 9.46±3.794 | 8.06±2.857 | 10.25±3.959 |
| t/F | 2.896 | 5.148 | 3.549 | 1.610 | 4.100 |
| P value | 0.004 | 0.000 | 0.000 | 0.108 | 0.000 |
SD, standard deviation.
Table 5
| Related factors | B | SE | Wald | P value | OR | 95% CI |
|---|---|---|---|---|---|---|
| Pain | 0.069 | 0.032 | 4.704 | 0.030 | 1.071 | 1.140–1.007 |
| Vulvar pruritus | 0.172 | 0.037 | 21.317 | 0.000 | 1.188 | 1.278–1.104 |
| Purulent secretions | 0.111 | 0.031 | 12.785 | 0.000 | 1.117 | 1.187–1.051 |
| Furuncle and swelling of vulvar ulcer | 0.070 | 0.041 | 2.932 | 0.087 | 1.072 | 1.162–0.990 |
| Malodor | 0.126 | 0.029 | 18.254 | 0.000 | 1.134 | 1.202–1.071 |
SAS, Self-rating Anxiety Scale; CI, confidence interval; OR, odds ratio; SE, standard error; B, beta.

Table 6
| Related factors | B | SE | Wald | P value | OR | 95% CI |
|---|---|---|---|---|---|---|
| Pain | 0.073 | 0.030 | 5.890 | 0.015 | 1.076 | 1.141–1.014 |
| Vulvar pruritus | 0.051 | 0.032 | 2.493 | 0.114 | 1.052 | 1.121–0.988 |
| Purulent secretions | 0.001 | 0.030 | 0.002 | 0.967 | 1.001 | 1.061–0.945 |
| Furuncle and swelling of vulvar ulcer | 0.095 | 0.039 | 5.918 | 0.015 | 1.099 | 1.186–1.019 |
| Malodor | 0.022 | 0.027 | 0.640 | 0.424 | 1.022 | 1.079–0.969 |
SDS, Self-rating Depression Scale; SE, standard error; B, beta; OR, odds ratio; CI, confidence interval.
Table 7
| Items | Total | Cured within 2 weeks or not, n (%) | Urine test, n (%) | |||
|---|---|---|---|---|---|---|
| Cured | Not cured | Turned negative | Did not turn negative | |||
| Anxiety | ||||||
| Yes | 135 | 83 (61.5) | 52 (38.5) | 80 (59.3) | 55 (40.7) | |
| No | 168 | 129 (76.8) | 39 (23.2) | 129 (76.8) | 39 (23.2) | |
| χ2 | 8.343 | 10.745 | ||||
| P value | 0.004 | 0.001 | ||||
| Depression | ||||||
| Yes | 106 | 66 (62.3) | 40 (37.7) | 65 (61.3) | 41 (38.7) | |
| No | 197 | 146 (74.1) | 51 (25.9) | 144 (73.1) | 53 (26.9) | |
| χ2 | 4.604 | 4.466 | ||||
| P value | 0.032 | 0.035 | ||||
Discussion
Vulvovaginitis refers to the inflammation of the vulva and vagina. It is considered a common reproductive system disease among prepubescent and adolescent girls that causes parental anxiety (19). It can be caused by infectious or non-infectious factors. Candida, trichomoniasis, and bacteria are the 3 most common causes of vulvovaginitis in adolescents and young adults (20). Non-infectious vulvovaginitis, which mostly occurs in preadolescent girls, is usually non-specific and caused by irritants, allergic reactions, or skin diseases (21), and the prevalence rate among preadolescent girls is between 25% and 75% (12,22,23). In the process of clinical diagnosis, a comprehensive assessment should be made in full combination with the patient’s medical history, physical and laboratory examination results to identify the cause, so as to carry out subsequent targeted and effective treatment (2).
Common clinical symptoms of vulvovaginitis include vaginal discharge, odor, itching, pain, dysuria, skin irritation, and burning. Gynecological physical examination shows vulva skin redness and swelling, vestibular vaginal mucosa congestion, and vaginal yellow or white purulent secretions, among others (24). For children with vulvovaginitis, the diagnosis is often delayed due to complex etiology, incomplete cognitive ability of young girls, inadequate health care by the parents, and limited gynecological examination, which leads to further progress of the disease. As a result, pelvic inflammatory disease is easily induced, and even abdominal infection in severe cases (21). Besides seriously affecting the physical and mental health of the children, it also increases the psychological burden of the parents and even causes anxiety, depression, and other negative emotions (25).
In this study, it was also found that different clinical characteristics of children with vulvovaginitis would lead to the emergence of negative parental emotions. The binary logistics regression analysis showed that vulval itching, secretion increase, and malodor are the common independent factors causing anxiety and depression in the parents of children. After comparing 45 children aged 2–12 years with vulvovaginitis, Cemek et al. (11) found that the most common symptoms were vaginal discharge (44.4%), vulvar erythema (37.8%), and vaginal itching (24.4%). This may be related to the child’s vulvar and vaginal microbes, but also to poor personal hygiene, both parents’ education level, and specific irritants.
The most common cause of increased vaginal discharge is bacterial vaginosis (BV), as shown by a cross-sectional study of 302 women aged 20–87 by de Camargo et al. (26). The prevalence rates of vulvovaginal candidiasis and trichomoniasis were 9.3% and 2.0%, respectively. When children manifest vulvar pruritus, secretion increase, and produce odor and other common clinical symptoms, their parents’ negative emotions also appear. At the same time, parents’ anxiety and depression can also significantly affect the prognosis of their children, forming a vicious cycle. Our study showed that parental anxiety or depression can significantly prolong the remission time of clinical symptoms such as pain, vulvar pruritus, purulent discharge, vulvar ulcers, and malodor in children. In addition, parents with anxiety and depression were associated with significant differences in the 2-week recovery rate and negative urine test rate of children (P<0.05).
In the treatment of children with vulvovaginitis, drugs including antibiotics are widely used to treat vaginitis, mainly comprising oral drugs, topical drugs, and vaginal suppositories. Monotherapy or combination therapy can be selected, and a personalized treatment plan can be selected according to the types of vaginitis and patients’ conditions (21). For example, metronidazole is commonly used clinically in trichomoniasis vaginitis, which has a strong inhibitory effect on trichomoniasis and can inhibit the reproduction and growth of anaerobic bacteria; suppositories of miconazole, clotrimazole, and nystatin are commonly used for vaginal administration of simple vulvovaginal candidiasis. For bacterial vaginosis, metronidazole is often selected for systemic treatment, whereas local treatment can involve lincomycin ointment vaginal smear, and so on. In the etiology of personalized treatment to improve the clinical symptoms of children, we should also pay attention to the parents with negative emotions including anxiety, depression, and other conditions. For these parents, timely effective communication, psychological counseling, and targeted guidance to reduce the psychological burden are important to improve the quality of family life and the prognosis of children. In conclusion, some clinical symptoms of children with vulvovaginitis can lead to negative emotions in parents, which in turn can lead to a poor prognosis for the child. Therefore, it is important to pay attention not only to the physical and mental health of the children in clinical treatment, but also to provide psychological guidance to the parents so that they can actively cooperate with the treatment and accelerate the recovery of the child.
The main shortcoming of this study is that due to limited manpower and time, the follow-up time was short, and the prognosis of patients and the change of negative emotion of parents were not followed up. In future studies, it is suggested to extend the follow-up time to further explore the changes of parents’ negative emotions throughout the course of the disease.
Conclusions
Parents of children with vulvovaginitis are highly susceptible to negative emotions due to the various clinical features of the child. The negative emotions of the parents significantly prolong the recovery time of the child. In clinical practice, adequate communication should be established with the parents of patients, and detailed education should be carried out to reduce the psychological burden of patients’ parents, so as to improve the prognosis of children.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-183/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-183/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-183/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-183/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Giovanini AF, Lobas A, Reisdoerfer G. Bacterial Vaginosis and Desquamative Inflammatory Vaginitis. N Engl J Med 2019;380:1088-9. [Crossref] [PubMed]
- Itriyeva K. Evaluation of vulvovaginitis in the adolescent patient. Curr Probl Pediatr Adolesc Health Care 2020;50:100836. [Crossref] [PubMed]
- McGreal S, Wood P. Recurrent vaginal discharge in children. J Pediatr Adolesc Gynecol 2013;26:205-8. [Crossref] [PubMed]
- Oliveira AS, Rolo J, Gaspar C, et al. Allergic vulvovaginitis: a systematic literature review. Arch Gynecol Obstet 2022;306:593-622. [Crossref] [PubMed]
- Kives S. Practical Pediatric and Adolescent Gynecology. In: Adams Hillard PJ. (ed). Practical Pediatric and Adolescent Gynecology. John Wiley and Sons, Ltd., 2013.
- Tartaglia E, Giugliano B, Ucciferri C, et al. Vulvo-vaginitis in prepubertal girls: new ways of administering old drugs. J Pediatr Adolesc Gynecol 2013;26:277-80. [Crossref] [PubMed]
- Baka S, Demeridou S, Kaparos G, et al. Microbiological findings in prepubertal and pubertal girls with vulvovaginitis. Eur J Pediatr 2022;181:4149-55. [Crossref] [PubMed]
- Delago C, Finkel MA, Deblinger E. Urogenital symptoms in premenarchal girls: parents’ and girls’ perceptions and associations with irritants. J Pediatr Adolesc Gynecol 2012;25:67-73. [Crossref] [PubMed]
- Sanctis VD. Diagnosis and treatment of the commonest vulvovaginitis in adolescents. Rivista Italiana di Medicina dell’Adolescenza 2005;3:25-31.
- Amabebe E, Anumba DOC. The Vaginal Microenvironment: The Physiologic Role of Lactobacilli. Front Med (Lausanne) 2018;5:181. [Crossref] [PubMed]
- Cemek F, Odabaş D, Şenel Ü, et al. Personal Hygiene and Vulvovaginitis in Prepubertal Children. J Pediatr Adolesc Gynecol 2016;29:223-7. [Crossref] [PubMed]
- Joishy M, Ashtekar CS, Jain A, et al. Do we need to treat vulvovaginitis in prepubertal girls? BMJ 2005;330:186-8. [Crossref] [PubMed]
- Jarienė K, Drejerienė E, Jaras A, et al. Clinical and Microbiological Findings of Vulvovaginitis in Prepubertal Girls. J Pediatr Adolesc Gynecol 2019;32:574-8. [Crossref] [PubMed]
- Juhász MLW, Korta DZ, Mesinkovska NA. Vaginal Rejuvenation: A Retrospective Review of Lasers and Radiofrequency Devices. Dermatol Surg 2021;47:489-94. [Crossref] [PubMed]
- Condado Condado H, Khaliulina Ushakova T, Acín Romero MP, et al. Vulvovaginitis due to Neisseria meningitidis in a 6-year-old girl. Enferm Infecc Microbiol Clin 2022;40:208-9. (Engl Ed). [Crossref] [PubMed]
- Rimoin LP, Kwatra SG, Yosipovitch G. Female-specific pruritus from childhood to postmenopause: clinical features, hormonal factors, and treatment considerations. Dermatol Ther 2013;26:157-67. [Crossref] [PubMed]
- Lambert V, Keogh D. Striving to live a normal life: a review of children and young people’s experience of feeling different when living with a long term condition. J Pediatr Nurs 2015;30:63-77. [Crossref] [PubMed]
- Bray L, Kirk S, Callery P. Developing biographies: the experiences of children, young people and their parents of living with a long-term condition. Sociol Health Illn 2014;36:823-39. [Crossref] [PubMed]
- Dei M, Di Maggio F, Di Paolo G, et al. Vulvovaginitis in childhood. Best Pract Res Clin Obstet Gynaecol 2010;24:129-37. [Crossref] [PubMed]
- Culhane JF, Rauh V, McCollum KF, et al. Exposure to chronic stress and ethnic differences in rates of bacterial vaginosis among pregnant women. Am J Obstet Gynecol 2002;187:1272-6. [Crossref] [PubMed]
- Zuckerman A, Romano M. Clinical Recommendation: Vulvovaginitis. J Pediatr Adolesc Gynecol 2016;29:673-9. [Crossref] [PubMed]
- Yasin J, Ayalew G, Dagnaw M, et al. Vulvovaginitis Prevalence Among Women in Gondar, Northwest Ethiopia: Special Emphasis on Aerobic Vaginitis Causing Bacterial Profile, Antimicrobial Susceptibility Pattern, and Associated Factors. Infect Drug Resist 2021;14:4567-80. [Crossref] [PubMed]
- Pérez-López FR, Phillips N, Vieira-Baptista P, et al. Management of postmenopausal vulvovaginal atrophy: recommendations of the International Society for the Study of Vulvovaginal Disease. Gynecol Endocrinol 2021;37:746-52. [Crossref] [PubMed]
- Rabinerson D, Krispin E, Werthiemer A. Pediatric and adolescent gynecology - vulvar diseases. Harefuah 2022;161:431-6. [PubMed]
- Altchek A. Pediatric vulvovaginitis. J Reprod Med 1984;29:359-75. [PubMed]
- De Camargo KC, Alves RR, Baylão L A, et al. Abnormal vaginal secretion: sensitivity, specificity and concordance between clinical and cytological diagnosis. Rev Bras Ginecol Obstet 2015;37:222-8. [PubMed]
(English Language Editor: J. Jones)



