
Comparing the impact of comprehensive care with conventional care in children with congenital heart disease: a systematic review and meta-analysis
Highlight box
Key findings
• Through meta-analysis, this study revealed that comprehensive nursing intervention can reduce the occurrence of complications after interventional treatment of congenital heart disease in children, reduce the time of puncture, time of operation, X-ray exposure time, length of hospitalization, and reduce the pain of the children.
What is known and what is new?
• Congenital heart disease in children poses a serious threat to the life and safety of children. Due to the young age, immature physiology, and psychology of the child, it is common to experience a sense of fear, anxiety, and other adverse emotions during interventional treatment, which may negatively impact treatment outcomes.
• In this study, a meta-analysis was performed to examine the effects of comprehensive care on interventional treatment in children with congenital heart disease.
What is the implication and what should change now?
• Comprehensive care has high application value and is worthy of promotion in clinical treatment.
Introduction
Congenital heart disease is a common congenital malformation in children, accounting for about one-third of all congenital malformations (1). Its occurrence is related to abnormal development of the great blood vessels and the heart during the fetal period. According to reports, the global incidence of congenital heart disease is 8.22 cases/1,000 live births, and the incidence of moderate to severe congenital heart disease is 1.5 cases/1,000 live births (2). In China, the situation is not optimistic, with the incidence of congenital heart disease being 8.98 cases/1,000 live births (3). Congenital heart disease in infants poses a serious threat to the life and safety of children. In recent years, interventional therapy has become one of the main treatment methods for children with congenital heart disease (4). It has the advantages of high diagnostic accuracy, less trauma, and radical cure (5). However, due to their young age and immature physiology and psychology, children are often prone to fear, restlessness, anxiety, and other negative emotions during the interventional treatment process, which may adversely affect the therapeutic effect. Following interventional treatment of congenital heart disease in children, various complications may occur, including thrombosis, high fever, infection, and bleeding (6). One study showed that compared with routine nursing, good nursing intervention (including whole-process information provision, preoperative stroking, music guidance, strict postoperative monitoring of signs and treatment of complications) is conducive to improving the safety of children’s surgery and reducing complications during interventional therapy and shorten the hospitalization time of children (7). However, the current sample size of individual study is small and there is a lack of reliable evidence to guide clinical practice. In this study, we conducted a meta-analysis on the impact of integrated care versus routine care during interventional therapy for children with congenital heart disease. We present the following article in accordance with the PRISMA reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-96/rc).
Methods
Search strategy and inclusion and exclusion criteria
The Wanfang Data Knowledge Service Platform, China National Knowledge Infrastructure (CNKI), PubMed, Web of Science databases and Embase databases were searched for related literatures published from the establishment of the databases to November 27, 2022. The Chinese and English search terms included “congenital heart disease”, “children”, “prevention”, and “interventional therapy”. The research language was limited to Chinese and English.
The following inclusion criteria were applied: (I) type of study design: randomized controlled trial (RCT); (II) study subjects: pediatric patients who met the clinical diagnostic criteria for congenital heart disease and underwent interventional treatment; (III) interventions and comparison groups: the control group was given conventional care and the experimental group was given comprehensive care on the basis of conventional care. Routine care included hospitalization knowledge, preoperative routine preparation, postoperative detection of vital signs, rest and postural care, symptomatic treatment and medication guidance. Comprehensive care also included psychological care, educational preaching, detailed assessment, dietary care, drainage tube care, enhanced monitoring, pain care, etc.; (IV) outcome: the outcome indicators were one or more of postoperative complications (number of cases), puncture time (minutes), pain score (points), surgical operation time (minutes), X-ray exposure time (minutes) and length of hospital stay (days).
The following exclusion criteria were applied: (I) publications that did not satisfy the research topic; (II) case analyses; (III) reviews, books, or conference papers; (IV) repeatedly or previously published research or data; (V) publications that did not include the full text article; (VI) papers that did not provide outcome indicators that satisfy the meta-analysis; and (VII) non-RCT studies.
Literature screening and data extraction
The retrieved documents are imported into the document management software Endnote X9 for duplication. Two researchers independently read the titles and abstracts for preliminary screening, deleted the literatures that did not satisfy the research topic, and then download the full text for further screening. Any disagreements were resolved by discussion and consultation with a third person. The extracted literature data mainly included the following: the first author and the year of publication, sample size, age of the research subjects, number of postoperative complications, puncture time, pain score, operation time, X-ray exposure time and hospitalization days.
Quality evaluation
Risk of bias was assessed using Cochrane Rob2 software (8). Cochrane Rob2 software is commonly used for quality assessment of RCT studies (9). The assessment consists of five main domains: bias in the randomization process, bias in deviations from established interventions, bias in missing outcome data, bias in outcome measures and bias in the selection of reported outcomes. Under each domain are a number of different signaling questions that researchers need to make judgements and answer objectively when evaluating the risk of bias. There are five options for the signal questions: yes, most likely yes, most likely no, no, and no information. Based on the answers to these signal questions, the risk of bias for each domain can be categorized as low risk, high risk and unclear risk, and then the overall risk of bias can be evaluated based on the risk of bias for each domain. Based on the aggregated risk of bias assessment, Rob2 is used to create a risk assessment chart (including a point chart of risk of bias and a bar chart of risk of bias).
Statistical analysis
The Stata 14.0 software was used to process the data included in this study. The count data, that is, the dichotomous data (complications), respectively extracted the number of events and the total number of people in the test group and the control group, and combined the risk ratio (RR) of each study. The measurement data, that is, continuous data (puncture time, pain score, operation time, X-ray exposure time, and hospitalization time), respectively extracted the number of events and the total number of people in the test group and the control group, as well as the mean and standard deviation, and combined the results of each study into a standardized mean difference (SMD). According to the P value and I2 value of the forest plots drawn in the Stata software, the degree of heterogeneity of the literature included in the meta-study was assessed. When the included studies showed no heterogeneity (P>0.1, I2<50%), the fixed effects model was used. When there was heterogeneity among the included studies (P<0.1, I2≥50%), the random effects model was used. Sensitivity analyses were conducted using a one-by-one exclusion of all literature included for each outcome indicator, examining the effect of individual study on the overall combined effect size outcome as well as heterogeneity. Tests of publication bias were performed using Egger’s test. P<0.05 for statistical analysis suggested statistical significance, except for the test of heterogeneity.
Results
Literature screening process and results
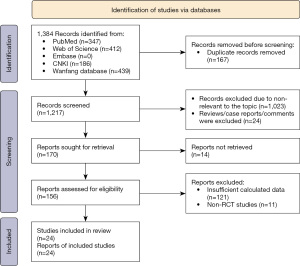
A total of 1,384 literatures were identified, including 439 from Wanfang Data Knowledge Service Platform, 186 from CNKI, 347 from PubMed, and 412 from the Web of Science database and no relevant literature was retrieved from the Embase database. After exclusion of 167 duplicate literatures, 1,023 literatures that did not meet the research theme, 17 reviews, books and conference papers, 7 case analyses, 14 papers that did not include the full text, 121 papers that did not satisfy the research indicators, and 11 non-RCT research papers, a total of 24 papers remained (5-7,10-30). The literature screening process and results are shown in Figure 1.
The basic characteristics of the included studies and the results of the risk of bias assessment
The basic characteristics of the included studies are listed in Table 1. In the 24 papers included in the study, there was a total of 2,028 subjects, including 1,025 patients in the experimental group and 1,003 patients in the control group. The 24 studies all provided information on the number of postoperative complications. A total of 7 studies provided puncture time, 7 studies provided pain scores, 11 studies provided operation times, 4 studies provided X-ray exposure times, and 13 studies provided length of hospital stay.
Table 1
| No. | First author | Year | Age of patients (range) | Total number of research subjects | Total number of test groups | Total number of control groups | Complications (number of cases) | Puncture time (minutes) mean ± SD | Pain score (score) mean ± SD |
Operation time (minutes) mean ± SD | X-ray exposure time (minutes) mean ± SD | Hospitalization time (days) mean ± SD | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Test group | Control group | Test group | Control group | Test group | Control group | Test group | Control group | Test group | Control group | Test group | Control group | ||||||||||||
| 1 | Chen (5) | 2012 | 1–14 years | 50 | 30 | 20 | 0 | 4 | 4.9±1.4 | 7.1±1.5 | 1.5±0.4 | 2.3±0.6 | 48.5±12.8 | 61.4±14.4 | 9.2±4.1 | 12.5±4.9 | 3.0±1.5 | 4.5±1.9 | |||||
| 2 | Qi (10) | 2013 | – | 80 | 45 | 35 | 5 | 10 | 4.2±0.4 | 7.1±0.9 | 1.7±0.1 | 3.1±0.4 | 44.7±3.6 | 59.8±3.9 | – | – | 3.3±0.6 | 5.2±0.2 | |||||
| 3 | He (11) | 2014 | 3 months–14 years | 158 | 79 | 79 | 13 | 30 | – | – | – | – | – | – | – | – | – | – | |||||
| 4 | Du (12) | 2015 | 2 months–15 years | 62 | 31 | 31 | 5 | 11 | – | – | – | – | – | – | – | – | – | – | |||||
| 5 | Liu (13) | 2015 | 1–14 years | 68 | 34 | 34 | 1 | 5 | – | – | 1.6±0.5 | 2.4±0.7 | 48.6±12.9 | 61.5±14.5 | – | – | 3.1±1.6 | 4.6±1.8 | |||||
| 6 | Tang (14) | 2015 | 2–13 years | 140 | 70 | 70 | 3 | 11 | 4.8±1.4 | 7.3±1.6 | – | – | 48.2±11.3 | 62.7±12.6 | 9.1±3.9 | 13.8±4.8 | 3.1±1.4 | 4.7±1.8 | |||||
| 7 | Feng (15) | 2016 | 1–13 years | 60 | 30 | 30 | 0 | 3 | – | – | – | – | 46.4±2.3 | 62.2±3.3 | – | – | 3.0±1.1 | 4.8±1.2 | |||||
| 8 | Li (16) | 2016 | 1–14 years | 40 | 20 | 20 | 0 | 16 | – | – | – | – | 46.5±2.1 | 67.5±2.4 | – | – | 3.0±1.2 | 4.7±1.5 | |||||
| 9 | Lv (17) | 2016 | 2.1–8.5 years | 68 | 34 | 34 | 4 | 15 | – | – | – | – | – | – | – | – | 5.0±2.7 | 8.0±6.2 | |||||
| 10 | Wu (18) | 2016 | 3–8 years | 48 | 24 | 24 | 4 | 21 | – | – | – | – | – | – | – | – | – | – | |||||
| 11 | Zhao (19) | 2016 | 3 days–6 years | 220 | 110 | 110 | 5 | 29 | – | – | – | – | – | – | – | – | – | – | |||||
| 12 | Gao (20) | 2017 | 0.9–6.2 years | 100 | 50 | 50 | 2 | 8 | – | – | – | – | – | – | – | – | – | – | |||||
| 13 | Liang (21) | 2017 | 1–14 years | 84 | 42 | 42 | 1 | 10 | – | – | – | – | – | – | – | – | – | – | |||||
| 14 | You (22) | 2017 | 1–13 years | 100 | 50 | 50 | 0 | 5 | – | – | – | – | – | – | – | – | – | – | |||||
| 15 | Zhao (23) | 2017 | 1.2–6.5 years | 88 | 44 | 44 | 1 | 4 | – | – | – | – | – | – | – | – | – | – | |||||
| 16 | Mayila (24) | 2018 | 5 months–9 years | 80 | 40 | 40 | 6 | 15 | – | – | – | – | – | – | – | – | – | – | |||||
| 17 | Shen (25) | 2018 | 1–12 years | 60 | 30 | 30 | 0 | 5 | 4.76±1.46 | 7.53±1.41 | – | – | 48.21±3.15 | 63.24±3.58 | 8.12±1.39 | 13.19±1.72 | 3.5±0.5 | 5.5±0.5 | |||||
| 18 | Yang (26) | 2018 | 2–10 years | 100 | 50 | 50 | 3 | 12 | – | – | – | – | – | – | – | – | – | – | |||||
| 19 | Zhang (27) | 2018 | 3 months–14 years | 80 | 40 | 40 | 7 | 16 | – | – | – | – | – | – | – | – | – | – | |||||
| 20 | Huang (28) | 2019 | 1–6 years | 50 | 25 | 25 | 1 | 6 | 5.89±0.67 | 9.21±1.22 | 1.76±0.66 | 3.3±0.76 | 53.37±8.48 | 59.93±8.72 | – | – | 4.13±0.87 | 5.21±1.39 | |||||
| 21 | Liu (29) | 2019 | 8 months–12 years | 32 | 16 | 16 | 0 | 4 | 4.73±1.12 | 6.91±1.24 | 1.97±0.23 | 3.11±0.52 | – | – | 8.76±1.65 | 10.83±1.88 | 4.67±1.13 | 5.97±1.34 | |||||
| 22 | Bi (30) | 2021 | 1–11 years | 80 | 40 | 40 | 2 | 7 | – | – | – | – | 55.32±13.09 | 79.36±12.17 | – | – | 5.69±1.24 | 7.88±1.95 | |||||
| 23 | Chen (7) | 2022 | 1–7 years | 98 | 50 | 48 | 9 | 19 | – | – | 1.82±0.44 | 3.77±0.96 | 53.12±8.44 | 60.13±8.67 | – | – | 4.26±0.77 | 5.45±1.38 | |||||
| 24 | Liu (6) | 2022 | 1 month–8 years | 82 | 41 | 41 | 2 | 7 | 4.5±1.3 | 8.9±1.6 | 3.1±0.8 | 4.2±0.5 | 50.5±11.3 | 60.3±11.5 | – | – | 3.6±0.7 | 5.5±0.9 | |||||
SD, standard deviation.
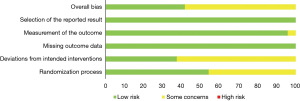
The Cochrane risk of bias assessment tool was used to evaluate the quality of the 24 included literatures. Figure 2 shows the summary map of the risk of bias obtained from the comprehensive evaluation of seven items including random allocation method and allocation concealment for the 24 studies included in this article. Figure 3 shows the statistics for each individual study as a percentage of each entry. The results show bias mainly from bias in the randomization process and bias from deviation from the established interventions. The results showed that most of the literatures belonged to low-risk or some concern level, and none of the studies were high-risk, suggesting that the quality evaluation of the included studies met the requirements.
Meta-analysis research results
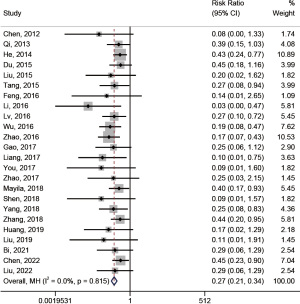
Complications
Among the included studies, all 24 articles provided complications as outcome indicators. A total of 2,028 subjects were included, with 1,025 patients in the experimental group and 1,003 patients in the control group. The heterogeneity test showed that there was no statistical heterogeneity among the literatures included in this outcome index (I2=0.0%, P=0.815), and the fixed effects model was used for meta-analysis. The results of meta-analysis showed that compared with the control group, comprehensive care in the experimental group had a protective effect on the occurrence of complications, and the difference was statistically significant [RR =0.27, 95% confidence interval (CI): 0.21 to 0.34, P<0.05; Figure 4].
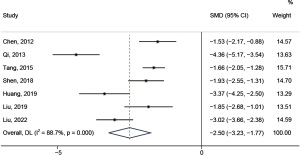
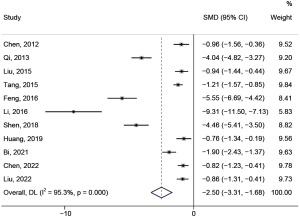
Puncture time
Seven articles provided puncture times as an outcome measure. A total of 494 subjects were included, with 257 in the experimental group and 237 in the control group. The heterogeneity test indicated that there was statistical heterogeneity among the literatures included in this outcome index (I2=88.7%>50%, P=0.000<0.1), and the random effects model was used. Meta-analysis revealed that compared with the control group, the puncture time of the comprehensive care group was significantly shorter (SMD =−2.50, 95% CI: −3.23 to −1.77, P<0.05; Figure 5).
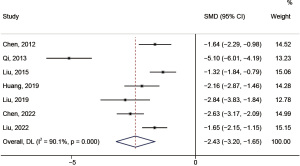
Pain score
Seven papers provided pain scores as outcome measures, including a total of 460 subjects, with 241 in the experimental group and 219 in the control group. The heterogeneity test indicated that there was statistical heterogeneity among the literatures included in this outcome index (I2=90.1%, P=0.000), and the random effects model was used. Meta-analysis demonstrated that compared with the control group, the pain score of the experimental group using comprehensive care was significantly lower (SMD =−2.43, 95% CI: −3.20 to −1.65, P<0.05; Figure 6).
Operating time
Eleven papers provided operation time as an outcome indicator, with total of 808 subjects, including 415 in the experimental group and 393 in the control group. The heterogeneity test indicated that there was statistical heterogeneity among the literatures included in this outcome index (I2=95.3%, P=0.000), and the random effects model was used. Meta-analysis showed that compared with the control group, the operation time of the experimental group using comprehensive care was significantly shorter (SMD =−2.50, 95% CI: −3.31 to −1.68, P<0.05; Figure 7).
X-ray exposure time
Four literatures provided X-ray exposure time as the outcome index, with a total of 282 subjects, including 146 in the experimental group and 136 in the control group. The heterogeneity test indicated that there was statistical heterogeneity among the literatures included in this outcome index (I2=94.4%, P=0.000), and the random effects model was used for meta-analysis. The results showed that compared with the control group, the X-ray exposure time of the comprehensive care group was significantly shorter (SMD =−1.29, 95% CI: −2.51 to −0.07, P<0.05; Figure 8).

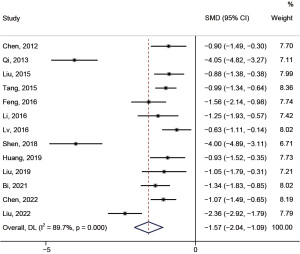
Length of hospital stay
Thirteen papers provided length of hospital stay as an outcome measure, with a total of 908 subjects, including 465 in the experimental group and 443 in the control group. The heterogeneity test indicated that there was statistical heterogeneity among the literatures included in this outcome index (I2=89.7%, P=0.000), and the random effects model was used. Meta-analysis revealed that compared with the control group, the hospitalization time of the experimental group using comprehensive care was significantly shorter (SMD =−1.57, 95% CI: −2.04 to −1.09, P<0.05; Figure 9).
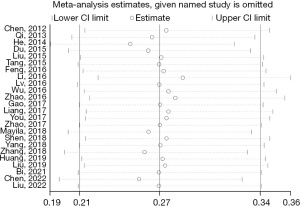
Sensitivity analysis
To ensure the accuracy and stability of the research results, sensitivity analysis was performed on the 24 literatures included in this analysis. As shown in the sensitivity map in Figure 10, the point estimates of each study in the figure are concentrated within the 95% CI, and no document was found scattered outside the interval, suggesting that the stability of the research results is relatively good.
Publication bias test
The bias of the included literature was examined using the Egger’s test. The results demonstrated that there was no publication bias in the included studies (P=0.061> 0.05, Egger’s bias test).
Discussion
Interventional surgery conforms to the minimally invasive concept advocated by modern clinical treatment and has been widely used in the management of children with congenital heart disease, as it is conducive to the early recovery of children. However, due to their young age and immature physical and psychological development, children have poorer tolerance to interventional surgery, and various complications may occur, which makes the quality of postoperative prognosis of children unsatisfactory. Therefore, scientific and good nursing intervention methods have been used as an effective way to improve the effect of interventional therapy in children. We herein conducted a meta-analysis of 24 literatures and found that compared with routine nursing intervention, comprehensive care can reduce the incidence of complications after interventional therapy for children with congenital heart disease, and reduce the puncture time, operation time, and X-ray exposure time of children. Furthermore, the length of hospital stay is decreased and children experience less pain. Comprehensive care is therefore worthy of application and promotion in the clinical setting.
Commonly used comprehensive nursing intervention includes psychological intervention, behavioral intervention, cognitive intervention, and clinical nursing technology intervention (31-34). Related studies have found that comprehensive nursing intervention can improve the prognosis of many diseases. Yu et al. found that 163 patients with alcohol dependence and depression showed significantly improved depression status following comprehensive nursing intervention (35). Cai et al. examined 320 diabetic patients and found that comprehensive nursing intervention effectively improved the quality of bowel preparation in diabetic patients and increased the detection rate of polyps and adenomas (36). In the interventional treatment of children with congenital heart disease, comprehensive nursing intervention often includes preoperative, intraoperative, and postoperative intervention. Preoperative intervention includes understanding the condition of the child before the operation; providing health education to the parents of the child; and relieving pain by touching, playing music, playing games, etc. Intraoperative intervention occurs while the child is in the operating room, and involves helping the child take a comfortable position, and evaluating the blood vessels of the child so that the puncture can be successful. Postoperative intervention includes the use of storytelling, look at pictures, and other ways to distract the child’s attention to relieve pain; good nasal cleaning and nursing; preventing the occurrence of complications such as thrombosis; helping children formulate scientific and nutritious recipes; and strengthening postoperative rehabilitation exercises for children (29). Although studies have evaluated the impact of comprehensive nursing interventions on the efficacy of interventional therapy for children with congenital heart disease, there is paucity of meta-analyses to systematically review this field.
Among the 24 studies included in this meta-analysis, 21 were published after 2015, accounting for 87.5% of the total literature, indicating that the included literature is up-to-date. This study found that comprehensive care after interventional treatment in children with congenital heart disease can significantly reduce the incidence of complications; reduce the time of puncture, operation time, X-ray exposure time, and hospitalization time; and reduce the pain of children. In this study, the Cochrane risk assessment tool was used for standardized scoring in the quality evaluation, aiming to ensure the objectivity and authenticity of the data, and to avoid information extractor bias or research quality scoring bias due to incomplete information extraction or unreasonable quality scoring. The Cochrane risk assessment tool found that the 24 documents included in the studies were all low-risk or somewhat concerned, and there was no high-risk level, suggesting that the quality of the included studies was high.
This meta-analysis systematically evaluated the impact of comprehensive care on interventional therapy for children with congenital heart disease from the aspects of complications, puncture time, operation time, X-ray exposure time, hospitalization time, and pain score, and the Cochrane risk of bias assessment was used for quality evaluation to ensure that the results more detailed and reliable. However, there are some limitations. First, we cannot confirm whether there are any unpublished relevant data, and there may be some bias in the selection of literature and data extraction. Second, due to the limited study characteristics, subgroup analysis was not performed in this evaluation.
Conclusions
In conclusion, this meta-analysis revealed that comprehensive nursing intervention after interventional therapy for children with congenital heart disease can reduce the incidence of complications; reduce the puncture time, operation time, X-ray exposure time, and hospitalization time; and reduce pain in children, and thus has high clinical application value.
Acknowledgments
Funding: The project was supported by the Hainan Province Clinical Medical Center.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-96/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-96/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-96/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang T, Li Q, Chen L, et al. Maternal Viral Infection in Early Pregnancy and Risk of Congenital Heart Disease in Offspring: A Prospective Cohort Study in Central China. Clin Epidemiol 2022;14:71-82. [Crossref] [PubMed]
- van der Bom T, Zomer AC, Zwinderman AH, et al. The changing epidemiology of congenital heart disease. Nat Rev Cardiol 2011;8:50-60. [Crossref] [PubMed]
- Zhang S, Liu X, Wang T, et al. Association and interaction effect of UCP2 gene polymorphisms and dietary factors with congenital heart diseases in Chinese Han population. Sci Rep 2021;11:8699. [Crossref] [PubMed]
- Zhang Y, Zhang ZW, Xie YM, et al. Toxicity of nickel ions and comprehensive analysis of nickel ion-associated gene expression profiles in THP-1 cells. Mol Med Rep 2015;12:3273-8. [Crossref] [PubMed]
- Chen YY. Effect of Nursing Intervention on Interventional Therapy for Children with Congenital Heart Disease. Nursing Practice and Research 2012;9:27-8.
- Liu Y, Zhang XY, Li S. The effect of nursing intervention on interventional therapy for children with congenital heart disease. Healthful Friend 2022;246-7.
- Chen HY. Effect of early nursing intervention on the effect and complications of interventional therapy for children with congenital heart disease. The Journal of Medical Theory and Practice 2022;35:1407-8.
- Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [Crossref] [PubMed]
- Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Qi HY. Effect of Nursing Intervention on Interventional Therapy for Children with Congenital Heart Disease. Health Horizon 2013;21:10.
- He LY, He Q. Effects of Postoperative Nursing in Pediatric Congenital Heart Disease Treated with Interventional Therapy. Clinical Medical & Engineering 2014;21:1473-4.
- Du EY. Nursing experience in 62 cases of children with congenital heart disease. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2015;7-8.
- Liu Q. Clinical care with the interventional therapy in children with congenital heart disease. Chinese Community Doctors 2015;31:143, 145.
- Tang SM, Li JY, Chen M. Analysis of the effect of comprehensive nursing on interventional therapy for children with congenital heart disease. Modern Medicine and Health 2015;3331-2:3.
- Feng CX. To Explore the Effect of Nursing Intervention in the Interventional Treatment of Children With Congenital Heart Disease. China Continuing Medical Education 2016;8:200-1.
- Li YH, Li M, Li YF. Effect evaluation of nursing intervention on interventional therapy for children with congenital heart disease. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2016;4:85, 88.
- Lv J. Observation on perioperative nursing effect of interventional surgery for children with congenital heart disease. China Practical Medical 2016;11:258-9.
- Wu L. Nursing intervention on 24 cases of pediatric cardiac intervention. Journal of Anhui Medical College 2016;15:110-1.
- Zhao WY. Exploring the application effect of comprehensive nursing intervention in interventional treatment of children with congenital heart disease. World Latest Medicine Information 2016;16:149, 152.
- Gao XQ. Effect of early nursing intervention on complications of interventional therapy for children with congenital heart disease. Journal of Bethune Military Medical College 2017;15:405-6.
- Liang JJ. Nursing analysis of interventional surgery for children with congenital heart disease. Electronic Journal of Clinical Medical Literature 2017;4:3652-3.
- You YJ. Effect of Nursing Intervention on Interventional Therapy for Children with Congenital Heart Disease. Henan Medical Research 2017;26:1134-5.
- Zhao M. Analysis of the preventive effect of comfort nursing on complications after interventional therapy for children with congenital heart disease. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2017;5:104-5.
- Mayila M. Study on perioperative nursing effect of interventional surgery for children with congenital heart disease. Diet Health 2018;5:230-1.
- Shen J. Effect of Nursing Intervention in Children with Congenital Heart Disease Intervention. Bao Jian Wen Hui 2018;101.
- Yang YD, Fu ZX. Observation and nursing analysis before, during and after interventional closure of congenital heart disease in children. Electronic Journal of Clinical Medical Literature 2018;5:124-5.
- Zhang YJ. Comprehensive nursing intervention experience of interventional therapy for children with congenital heart disease. Electronic Journal of Practical Clinical Nursing Science 2018;3:93, 96.
- Huang SS, Xu F, Chen XJ, et al. Observation on the Effect of Early Nursing Intervention on Interventional Therapy for Children with Congenital Heart Disease and Analysis on the Incidence of Complications. Electronic Journal of Practical Clinical Nursing Science 2019;4:40, 55.
- Liu LJ. Discussion on the effect of nursing intervention on interventional therapy for children with congenital heart disease. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2019;7:95-6.
- Bi JA, Gao J. The application of intraoperative nursing cooperation in interventional closure of congenital heart disease in children. Ke Xue Yang Sheng 2021;24:175.
- Lancioni GE, Singh NN, O'Reilly MF, et al. Behavioral intervention approaches for people with disorders of consciousness: a scoping review. Disabil Rehabil 2022;44:7677-92. [Crossref] [PubMed]
- Lissek VJ, Ben Abdallah H, Praetorius A, et al. go4cognition: Combined Physiological and Cognitive Intervention in Mild Cognitive Impairment. J Alzheimers Dis 2022;89:449-62. [Crossref] [PubMed]
- Yang M, Zhang Z, Nice EC, et al. Psychological intervention to treat distress: An emerging frontier in cancer prevention and therapy. Biochim Biophys Acta Rev Cancer 2022;1877:188665. [Crossref] [PubMed]
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, et al. Randomized controlled trial of cognitive-behavioural therapy for coexisting depression and alcohol problems: short-term outcome. Addiction 2010;105:87-99. [Crossref] [PubMed]
- Yu D. Study on the effect of comprehensive nursing intervention on the rehabilitation of alcohol-dependent patients with depression [Master]: Xinxiang Medical University; 2021.
- Cai L. Construction of comprehensive nursing intervention plan for intestinal preparation quality of patients with diabetes and clinical empirical research. Fuzhou: Fujian Medical University, 2021.
(English Language Editor: J. Teoh)



