Endoscopic craniosynostosis repair
Introduction
Humans are relatively unique among mammals with regard to our cranial growth and development. Because of the relatively large size of the human brain, and the fact that we are bipedal and therefore have a narrow pelvic outlet, human babies are born much earlier in the developmental cycle of the brain than all other mammals. Therefore, whereas a newborn calf can walk away from a mother cow within moments after birth, infants take about a year before they attain the skills of ambulation and speech. Not surprisingly, this corresponds to when the human brain has reached nearly 80% of its adult size.
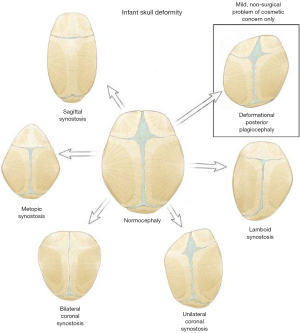
The very rapid growth of the human brain in the first postnatal year of life is only feasible because the human brain is encased in an open skull. On a continual basis the brain is growing and pushing apart skull bones, while at the same time the sutures, which are the growth plates between the major cranial bones, are depositing new bone. Unfortunately, this system fails when any of these growth plates prematurely fuse, a condition known as craniosynostosis (Figure 1).
Craniosynostosis occurs when two or more of the bone plates are fused together prematurely. In the normal course of events, fusion of the cranial sutures does not occur until all of the growth plates of the skeletal system fuse, which is generally at the end of puberty. The common misconception is that the sutures fuse at 1 to 2 years of age, which is ‘functionally’ true, but not anatomically accurate, with the exception to this being the metopic suture, which can fuse normally in infancy. Although the sutures are not anatomically fused, since brain growth is substantially completed by 2 years of age, the role of the sutures is very limited after that point in time. However, a very small percentage of babies can develop craniosynostosis after one year of age, which results in a normal cranial shape but increased intracranial pressure.
Evidence of craniosynostosis has been apparent in skulls since early history, but viable treatment options have only been developed over the past century. Initial attempts at treatment involved open operations with large incisions, followed by surgical removal of the fused cranial suture, an operation known as strip craniectomy. Unfortunately, in many patients the operated suture re-fused too quickly, and did not achieve adequate correction. This led to the development of much larger operations, heralded by Dr. Tessier, in which large segments of cranial bone were removed and replaced in a more anatomic position. However, these operations were not without their own set of complications, including the issues associated with a very large surgical procedure in an infant, and concerns about impaired growth patterns over time leading to some degree of regression. In addition, re-fusion of skull bones remained a problem (1-3).
In the 1990s Drs. Jimenez and Barone described their experience with an innovative technique combining the technology of minimally invasive endoscopic surgery with post operative orthotic therapy (4,5). The endoscope is used to perform the traditional strip craniectomy using very small incisions with minimal blood loss. In addition, this allowed for minimal tissue disruption, and the bone generating dura and periosteum were largely untouched. Postoperatively the orthosis then insures that skull growth progresses in the desired direction. The directed growth of the brain and skull prevents the rapid re-fusion of the suture that had been seen historically. Their work has ushered in the new era of endoscopic surgery for craniosynostosis (1,3,6-10).
Endoscopic strip craniectomy-evolution, not revolution
One of the more intriguing aspects of this new technology is how slowly it has been adopted. At this point in time there are dozens of peer-reviewed articles in the literature regarding the use of these endoscopic techniques for craniosynostosis, yet many people still consider it new, “experimental”, unproven, and even dangerous. In fact, there are now more published articles on this technique then essentially any other technique used for the correction of craniosynostosis. It is fair to say that its safety and efficacy have been well established, and many centers with proficiency in both open and endoscopic techniques consider minimally invasive surgery the standard of care for young infants with craniosynostosis.
Perhaps this slow adoption is now surprising in a historic context. Interestingly, many new surgical procedures are often met with resistance by those in the medical community with expertise in performing the traditional procedures. It is fair to say that laparoscopic cholecystectomy is now the procedure of choice for removal of a gallbladder. However, when the technique was first developed, it was met with equal skepticism and concern (11,12). Some of the early literature on the use of the laparoscope for cholecystectomy can almost be looked upon comically 25 years later, with titles such as “Laparoscopic cholecystectomy-let us control the virus”. Within a short period of time, though, it became apparent this was a safe and effective technique, evidenced by the article “Laparoscopic cholecystectomy—evolution, not revolution”. Certainly laparoscopic cholecystectomy is not completely analogous to the use of the endoscope for the treatment of craniosynostosis, as ultimately the goal of laparoscopic cholecystectomy is removal of the gallbladder, which is the same goal that is achieved with open cholecystectomy. For craniosynostosis surgery, the goal of surgery is philosophically different. Although it employs the endoscope, it is not a reconstruction of the skull as performed with open techniques, but an attempt to restore normal skull anatomy such that subsequent brain growth can lead to a slow correction of cranial morphology over time. An important lesson learned from the laparoscopic cholecystectomy era is that expertise in this minimally invasive field was only achieved by a thorough understanding of the anatomy and the disease process by surgeons experienced in the open techniques (11). In addition, minimally invasive techniques for craniosynostosis surgery should only be performed by those who thoroughly understand craniosynostosis, and also have expertise in open techniques.
Appropriate surgical candidates
Because endoscopic techniques are essentially restoring normal anatomy, as opposed to reconstructing the skull at the time of surgery, they rely on subsequent brain and skull growth to obtain the correction. Since the very rapid growth of the brain occurs over the first 3 to 6 months of life, endoscopic surgery needs to be performed early (4,8,13). In my personal series, the average age at surgery is 3.1 months, and after the child reaches 6 months of life, the appeal of endoscopic techniques wanes, especially when the brain is the ‘engine’ that drives growth. Techniques such as the internal fixation of springs or distractors, devices that can slowly push the bones apart, can expand the age range for these surgeries (14-19). Springs seem to be growing in popularity, and the first commercially available springs are now available. The downside of using these techniques is that a 2nd surgery is required to remove the device.
In contrast to endoscopic techniques, open craniosynostosis correction surgeries are generally performed in the 6 to 12 months age range. For this reason, many pediatricians are in the habit of referring children with suspected skull deformity to a craniofacial expert at a slightly older age, essentially observing the condition for several months to be certain it is craniosynostosis. Therefore, as a community switches to the use of these minimally invasive techniques, the referral patterns do need to change. Most surgeons practicing minimally invasive techniques for craniosynostosis encourage referral of the child as soon as there is a suspicion of the diagnosis. Early diagnosis and referral then gives the family the option to consider both the endoscopic and open techniques. This certainly can be a paradigm shift, and is something that the primary care physician should be aware of.
With the use of minimally invasive techniques, parents must also be aware that the morphological changes are going to be slow after surgery, and that they must be patient. For those in whom this may be problematic, open surgery is an excellent alternative that leads to an immediate correction. The advantages of the minimally invasive surgery are that it is physiologically generally much better tolerated by the baby, leaves very small and essentially invisible surgical scars, and is usually associated with very little blood loss.
Surgical techniques
General principles for the endoscopic treatment for craniosynostosis will be reviewed here, and then expanded upon below for the specific types of sutural fusions. It is again important to note that endoscopic treatment is philosophically different from open treatment, meaning not only is the technique different, but the way in which the skull shape corrects is different (8). With open techniques the general goal is correction of the skull shape at the time of surgery, whereas with endoscopic techniques the goal of surgery is removal of the fused portion of the bone, in an attempt to recreate normal anatomy (20,21).
For most endoscopic operations, the access to the skull requires one or two small incisions, each approximately 2 cm in length and perpendicular to the fused suture. Access to the underlying dura is accomplished by creating a burr hole using a high-speed drill. This burr hole is then locally enlarged with bone cutting instruments called kerrisons, and then the desired strip of bone is removed by working away from the incision. Drills, scissors and ultrasonic aspirators can also be used to remove the bone (22). Surgeons will differ in the surgical techniques used, whereas some perform minimal one centimeter strip craniectomies, others remove a much wider section, and create barrel stave cuts in the surrounding bone as well (23,24). In the experience of the author, with effective post-operative adjuvant therapy, a minimal 1 cm strip craniectomy along the suture is adequate to achieve the desired end result.
Because there is potential for bleeding, there should be excellent communication with the anesthesia team, and it is safest to have packed red blood cells available in the operative suite (25). Hemostasis can be achieved with cautery on the bone edges, or with the use of gelatin products which promote hemostasis. There is further discussion of the safety of the technique below.
Post operative therapy to achieve desired skull growth
As initially described, these minimally invasive endoscopic operations have generally been followed by helmet therapy to achieve the desired result. The ideal orthosis promotes growth in the direction that has previously been restricted, and limits, but does not prevent, growth in the areas that were previously overcompensated due to the fusion. In the view of the author, if there is a loss of growth in any direction, then the helmet is overly restrictive in that direction. The advantages of the helmet is that it allows for growth in a three-dimensional fashion, can be modified over time to achieve specific corrections in certain areas, and does not require any further surgeries. The limitations of the helmet include the need to wear the helmet, the need to adjust the helmet on a regular basis, generally at 2 to 4 week intervals, and the disruptions that this could place on the family. The family is generally counseled that helmet therapy might be necessary up to one year of age, although in actuality the average length of helmet treatment is approximately 6 to 7 months (26,27).
Spring therapy is a newer way of treating the infant after the endoscopic removal of the suture. In this case, the spring serves as the driver of growth in the desired direction, and one substantial benefit is that this extends the age of therapy, as we are no longer relying on brain growth alone to achieve the correction. This may be an excellent hybrid model for continuing to use minimally invasive techniques but expanding the age continuum. The downside of the spring therapy is that it can only correct growth in a single direction, cannot be modified over time, and requires a 2nd operation to remove the springs, although this subsequent operation is very brief. Reported complications of spring therapy are low, and may include wound issues as well as the spring shifting and therefore not moving the bones in the desired direction. In this case, the spring can be removed and a helmet can be used to correct the shape. One additional complication is the spring etching into the bone edge as it expands, but not actually pushing the bones apart, which would lead to a less optimal correction (14-18).
Distraction osteogenesis is another technique to actively drive the bones apart after surgery. Distractors are surgically implanted devices, and require a portion of the distractor to exit through the skin. On a daily basis a screw is turned to expand the distractor and push the bones apart. As compared to the other techniques, there is a much higher concern for infection due to the device exiting through the skin. In addition, as is the case with surgical springs, the distractor requires a 2nd operation to remove it (28-32). In the age of both springs and helmets, the role of distractors which transgress the skin for minimally invasive cases is probably limited, but they have substantial roles in the treatment of children with craniofacial deformities. All children with craniosynostosis should be followed for several years to look for signs of sutural refusion, whether they were treated with open or endoscopic techniques (33-35).
Types of craniosynostosis
Any of the six major cranial sutures can close in a pathological fashion, leading to a stereotypic change in the cranial morphology. Overall, the incidence of craniosynostosis is one in every 2,000 live births. The most common suture to be affected is the sagittal suture, which results in an elongated and narrow skull. In order of decreasing frequency, the other affected sutures are a unilateral coronal suture, metopic suture, bilateral coronal sutures, and finally the lambdoid suture. Children with syndromic craniosynostosis are much more likely to have multiple and/or unusual combinations of sutures fuse. In this section the general techniques and outcomes for the different types of craniosynostosis will be reviewed.
Sagittal craniosynostosis
Sagittal craniosynostosis is, by far, the most common type of craniosynostosis. Approximately 50% of all craniosynostosis conditions affect this suture. Because it prevents normal lateral growth of the skull at the parietal bones, it leads to narrowing of the skull with elongation in both the frontal and occipital directions. Although subtleties to the presentation can exist, typical features include frontal bossing and occipital bathrocephaly, which refers to the narrowing in the occiput. In addition, there is commonly a ridge along the sagittal suture.
This condition is particularly amenable to minimally invasive techniques, and the results should be overall excellent with minimal need for any further corrective surgeries. The surgery is performed by making two incisions, one just behind the coronal sutures, and another just in front of the lambdoid sutures, each approximately 2 cm in length. Burr holes are placed at each incision, followed by removal of the fused sagittal suture. As little as a 1 cm strip should allow for adequate correction, especially if post operative adjuvant treatment such as a helmet or springs is used (24). Some authors advocate removal of up to 6 cm of bone (23), which replicates the traditional open repair for this suture that had been originally used decades ago. Is also possible to make a lateral cuts into the parietal bone and occipital bone, if further manipulations are desired.
The typical length of the surgery should be approximately 30 to 40 minutes. For children over 5 kg, the need for blood transfusion should be exceedingly small. Typically, children are admitted overnight and discharged the following morning. When helmets are used, this phase of therapy should start within 1 to 2 weeks to avoid any chance of re-fusion of the suture before the phase of correction.
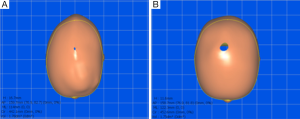
Most children with sagittal craniosynostosis will present with a cephalic index, which is the width to length ratio of the skull, that ranges from 0.6 to 0.7. The normal range is approximately 0.75-0.85. In general, surgery should result in a 0.1 improvement in the cephalic index at the completion of therapy (Figure 2). Between 1 to 2 years of age, it is common to see slight regression in the cephalic index with both endoscopic and open surgery (36). Overall, the reported results of treatment for the two modalities are quite similar (20,37-39).
Metopic craniosynostosis
The fusion of the metopic suture results in a much less stereotypic response than any other cranial suture. Although most cranial sutures will not fuse until the end of puberty, the metopic suture can be fused in normal infants by 2 to 3 months of age, and even rarely at birth. This does not necessarily result in an abnormal head shape or a need for treatment. In some babies it is simply a radiographic finding, whereas in others they may develop a ridge along the metopic suture but have a completely normal head shape. This ridge will dissipate over 2 to 3 years as the surrounding frontal bones thicken, and as long as the head shape is normal the metopic ridge never requires surgical treatment. When fusion of the metopic suture leads to a significant alteration of the forehead, a triangular shape known as trigonocephaly, surgical intervention may be warranted due to appearance and associated compression of the frontal lobes.
The endoscopic surgery for metopic craniosynostosis is performed via a single small skin incision at the hairline. This is generally curved to follow the hairline, and is 2 cm in width. A drill is used to create an opening below the incision, which is then locally expanded. A 1 cm strip craniectomy is performed going back to the anterior fontanelle. Attention is then moved inferiorly, and bone must be removed all the way down to the frontal nasal junction in order for the operation to be successful. As the bone gets quite thick inferiorly, a drill or an ultrasonic bone dissolving device is helpful to remove the bone in that region. At the completion, the frontal bones should move independently. It is important to note that there are veins which bridge between the dura and the bones in this region, and bipolar cautery should be used to coagulate the veins in advance of the bone removal.
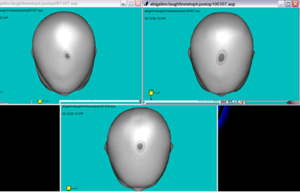
The surgical treatment of this condition should lead to significant improvement in the forehead shape regardless of the modality of treatment (Figure 3). The mid-face remains somewhat narrow in all children treated for metopic craniosynostosis, and this is equally true of open or endoscopic techniques. With the open operation the superior portion of the orbit is mechanically moved laterally, but the inferior portion of the orbit is not adjusted. There is no justification to support the belief that open surgery corrects hypotelorism (smaller distance between the eyes) better than endoscopic surgery (24,40).
Unilateral coronal craniosynostosis
Unilateral coronal craniosynostosis tends to be a much more deforming condition then the simplicity of the suture fusion would imply. Because it is an asymmetric process, the results to symmetry are far more significant, and it is therefore far more difficult to get an adequate surgical result. The condition results not only in flattening of the brow and forehead on the affected side, but marked deviation of the nose towards the affected side. This deviation continues all the way down to the point of the chin (41). In addition, the ear on the affected side is advanced forward. It has been long established that getting adequate correction of the facial asymmetry via the open procedures is technically very challenging. In addition, surgeons advocate doing an overcompensation of the forehead to try to account for the unsteady growth that occurs over the next 1 to 2 decades, and the revision rates are definitely higher than for the midline craniosynostosis conditions (42-44). Interestingly, and surprisingly, the results of the endoscopic surgery seem to mitigate against many of these problems (41).
Surgically, the treatment of unilateral coronal craniosynostosis is fairly simple. A 2 cm incision perpendicular to the fused suture is outlined, generally at the midpoint between the anterior fontanel and the lateral canthus of the eye. A burr hole is placed using a high-speed drill, and then in standard fashion the endoscope is used to separate the dura off of the under surface of the bone. Dissection is continued towards the anterior fontanel, and a 1 cm strip craniectomy is performed. Attention is then turned towards the inferior region, and the 1 cm strip craniectomy is continued down to the lateral canthus. As the sphenoid ridge deviates medially towards the orbital roof, which it does so in a pathological fashion in this condition, it is important to deviate behind the ridge and continue the bone dissection until the lateral canthus is reached inferiorly. At the completion of surgery the frontal and parietal bones should move independently.
The minimally invasive endoscopic treatment of this condition has offered several very unexpected benefits with regard to the facial features and ophthalmologic complications of the condition. It has only been through years of follow-up that we have been able to appreciate the unanticipated benefits of treating this endoscopically at an early age. These benefits are enumerated below.
The facial distortion from unilateral coronal craniosynostosis is quite significant. As mentioned above, there is a marked deviation of the nose towards the affected side, and this continues all the way down to the point of the chin. One of the early benefits of the endoscopic operation is that the nasal and facial features start to correct fairly quickly, and studies have shown that the correction is significantly better than with the open techniques (41). This is likely a result of doing the surgery at an early age, and anecdotally this had been described by surgeons decades ago when they were doing open strip craniectomies.
Strabismus is a very common associated finding with unilateral coronal craniosynostosis, because the orbit on the affected side is significantly higher and shallower than the contralateral side. Authors have described that up to 70% of infants with unilateral coronal craniosynostosis have associated strabismus, which may present as an obvious misalignment of the eyes, or more subtly as a head tilt. Ophthalmologists also consider this a particularly difficult strabismus to correct surgically. Two studies have now shown a significant improvement in strabismus after the endoscopic release of unicoronal craniosynostosis, with a sevenfold risk ratio reduction regarding the need for subsequent surgery on the eye (45,46).
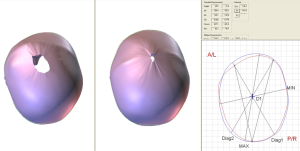
With regard to the flattening of the forehead, there is no doubt that the improvement is much slower with the minimally invasive techniques than with an open frontal orbital advancement. However, it has been gratifying to see that the changes continue to improve for approximately 4 to 5 years (Figure 4). This is in contrast to the open procedures, for which the correction tends to be perfect, or even overcorrected, at the time of surgery, but with a somewhat high regression rate. What we have noticed in follow-up imaging on the children who have undergone endoscopic treatment is that the majority of them form a normal looking coronal suture as the bone fills back in. This raises very interesting questions regarding the genetics of the condition. Obviously children with unilateral coronal craniosynostosis are capable of forming a normal suture, as they do so on the contralateral side. There would appear to be some time-dependent external factors that cause the suture to fuse on only one side during pregnancy, such as external pressure on that side based on intrauterine positioning. In opening the suture endoscopically, with minimal disturbance of the surrounding soft tissues and bone, it is almost as if the genetic clock is being reset and a new suture is now formed. The clinical consequence of this is that the growth continues to improve gradually for many years. In our busy craniofacial clinic there is fairly consistent agreement that the best results of this condition, looking out 5 to 10 years, are in those children that have had the suture treated endoscopically followed by orthotic therapy.
Bilateral coronal craniosynostosis
Bilateral coronal craniosynostosis can happen sporadically, but has a much higher association with syndromic conditions than single suture craniosynostosis. The classic cranial dysmorphology from this is called turribrachycephaly, which indicates a towering head shape which is very flat in the frontal region. Children with this condition should be screened by a geneticist; arguably this is true for all children with craniosynostosis, but for this particular condition the association with genetic mutations is even higher (47). As such, the rate of re-fusion of the sutures and the need for subsequent reoperation is higher with either endoscopic or open techniques (35).
In the experience at our center approximately 30% of children with bilateral coronal synostosis will require a 2nd operation, as the sutures refuse too quickly and brain growth becomes limited. This is often expressed by a falloff in the head circumference percentiles. One can reasonably ask why consider minimally invasive surgery if there is a high rate for subsequent surgery. The benefit of the early endoscopic surgery for this condition is that the classic turribrachycephaly tends to worsen over the first several months of life if not treated early, and becomes so severe that it is quite difficult to correct even with large open operations. In fact, in many parts of the world it is becoming the standard of care to expand out the occipital region in the first 2 to 3 months of life in children with bilateral coronal craniosynostosis. Although this may seem counterintuitive, by moving out the back of the skull the marked growth in the height of the skull is reduced (48-52). Similarly, using endoscopic techniques to open the coronal sutures leads to a marked reduction in the height of the head. This reduction in the subsequent dysmorphology over the first year of life, in addition to the fact that the majority of patients only require one surgery, is the reason that minimally invasive endoscopic surgery can be considered for this condition (8,13,53).
The surgical technique is identical to the correction of unilateral coronal craniosynostosis, with the obvious exception that the surgery is performed bilaterally. The postoperative adjuvant therapy is to direct growth towards the front of the head, thereby reducing the growth in the height of the head. The typical preoperative cephalic index in these children is 0.9-1.0, and with successful surgery this should be reduced by 0.1. As mentioned, it is imperative to follow the head circumference closely to look for any sign of growth retardation as an indicator of suture re-fusion.
Lambdoid craniosynostosis
Lambdoid craniosynostosis is by far the least common form of sutural fusion, excluding unusual combinations of sutures that are sporadically seen. It is important to understand that the vast majority of children presenting with flattening in the occiput do not have lambdoid synostosis, but have deformational plagiocephaly. In fact, whereas deformational changes are seen in upwards of 20% of the population, lambdoid synostosis is only seen in about two or three out of every 100,000 children. One distinctive feature on clinical exam is that with deformational plagiocephaly the occiput, ear, and forehead are all advanced on the same side, whereas with lambdoid synostosis the forehead is essentially normal and the ear is posteriorly displaced on the side of the flattening.
The surgery to correct lambdoid craniosynostosis involves two incisions, both perpendicular to the suture. One is at the superior end of the suture, where it meets the sagittal suture, and the other at the inferior end of the suture. The bony removal traverses the transverse sinus, and care must be taken in this region. Thankfully, the dura separates from the bone very easily when the suture is used, unlike how it handles at a normal suture.
Similar to unilateral coronal craniosynostosis, lambdoid craniosynostosis tends to make the skull very asymmetric. Many of the changes, such as a windswept appearance of the skull (literally meaning that the skull appears to be blown over towards one side), are very difficult to correct in an open operation. The experience with using minimally invasive endoscopic techniques is relatively limited due to the rarity of the condition, but at our institution we have found the results to be excellent. Likely because of the much younger age at surgery, and the early use of the helmet to gradually pushed the head back, there seems to be much more correction of the overall deformity. Either open or endoscopic techniques are more than adequate for correcting the flattening of the occiput on the affected side, but in our experience the earlier surgery seems to offer a better correction of the secondary changes in the skull. Overall, there is inadequate experience due to the rarity of this condition to draw any firm conclusions, but it is quite clear endoscopic procedures are promising for this condition.
Safety of surgery
In the early days of minimally invasive endoscopic surgery for craniosynostosis there was significant concern by many that the lack of complete visualization of the structures in an open fashion would lead to increased complications. It is now quite clear, and supported by close to two decades of experience, that endoscopic surgery is simply better tolerated by the baby and is, by all measures, as safe as, or safer than open techniques (25,54-57). Multiple studies have now shown that the endoscopic techniques afford a much shorter surgical time, significantly less blood loss and significantly lower blood transfusion rates. A study was performed at our institution looking consecutively at the first 100 patients who underwent this procedure. The average surgical time was 48 min, with an average estimated blood loss of 23 mL. Eight infants required blood transfusion (25). It was determined that the transfusion rates were much higher in infants under 5 kg, and therefore, with rare exceptions, we now wait for the infants to attain a weight of 5 kg before surgery, which is generally achieved by 8 to 10 weeks. The transfusion rates have dropped down to approximately 2%. The children are not admitted to the intensive care unit unless there is a confounding medical condition, and the vast majority of children are discharged on postoperative day one.
There is increasing concern about the use of anesthesia in infants due to the potential for neurotoxicity. There are competing concerns including both younger age at anesthesia, as well as longer duration of anesthesia, both being associated with possible worse outcomes. A recent study has shown a measurable decline in subsequent performance on cognitive tests for every additional 30 minutes under anesthesia in children who had undergone cranial vault surgery for single suture craniosynostosis (58). Therefore, although the surgery for minimally invasive release is done earlier, the marked reduction in time under anesthesia may favor this technique with regard to neurocognitive outcomes.
Cost of surgery
Multiple studies have now established that the minimally invasive endoscopic treatment for craniosynostosis offers a significant cost savings (59,60). These results are perhaps surprising because of the need for postoperative adjuvant therapies such as a helmet, and the increased disruption to family time and parental earnings as a result of more frequent trips to the medical facility. However, this must be balanced against the much shorter initial hospital time as well. In one study, the relative one-year costs, including all parental time and the cost of postoperative helmets, showed that the endoscopic treatment was 40% of the open treatment cost for the same condition (59). In the era where the value of medical procedures needs to be closely evaluated, if there is an equally efficacious procedure that is a substantial cost savings this component of care cannot be overlooked.
Discussion
When the new era minimally invasive endoscopic surgery was introduced there was significant concern that the field of craniofacial surgery was returning to operations that had failed in the past, and that those who ignored history would be forced to repeat it. Craniofacial surgeons were legitimately concerned that strip craniectomy operations had not worked, which is why we had converted to large open cranial vault reconstructive surgery. However, the modern operation is quite philosophically different from the strip craniectomies of the past. First, the operation is done in a way that causes very little surrounding tissue destruction, so that the normal milieu of dura and periosteum is preserved. Secondly, thanks to the experience of prior generations of craniofacial surgeons, it is clear that one cannot simply open the suture and expect adequate surgical outcomes. This is why the post operative adjuvant therapy is so important to achieving the desired results. At this point in time there is simply too much clinical experience, data, and published literature for any reasonable craniofacial surgeon to simply discount minimally invasive techniques, and it is fairly clear that the minimally invasive operations will continue to thrive and gain increasing market share. At least one study has even shown it is a less stressful experience for the family to have their child treated this way (61).
Indeed, as an experience craniofacial surgeon, I would argue that we have now achieved essential parity between open and endoscopic techniques from a cosmetic perspective. This, coupled with a markedly decreased surgical time, and an operation that is tolerated much better by families and infants (61), indicates that this operation has a meaningful place in the treatment of children with craniosynostosis. However, it is probably no longer enough to only look at the cosmetic outcomes in children with craniosynostosis, and as a community of craniofacial surgeons we need to be evaluating these children more scientifically. Over the next 1 to 2 decades we will see marked advances in the genetics of craniosynostosis (47), which will truly help us understand the conditions much better. We also need to strive to look at neurocognitive outcomes, as the ultimate goal is not simply to have a child with a good cosmetic outcome, but to maximize brain growth and development. At least one recent study, not involving children who have undergone minimally invasive surgery, has shown cognitive differences based on treatment type (62). This study involved an expansion technique versus a compression technique (the width was expanded but the length was actually compressed at surgery), and showed that the cranial vault expansion technique had improved cognitive outcomes. This is not comparable to the minimally invasive operation, which involves directed growth, but no compression. Indeed, in the minimally invasive surgery, although the correction is not immediate, it is still achieved earlier in the patient’s life than doing a cranial vault reconstruction, which is usually done at 6-9 months, as opposed to 3 months, of age. Doctors Jimenez and Barone have pushed the envelope with the development of these minimally invasive endoscopic techniques, and as a community we need to take it to the next step, truly establishing the overall developmental outcomes in these children.
Conclusions
Minimally invasive endoscopic techniques are excellence alternatives to open craniofacial repairs, and this is now supported by nearly two decades of literature. Factors which favor a good outcome from minimally invasive surgery include a younger age at surgery than open surgery, and effective postoperative adjuvant therapy, such as an external orthosis, or internal springs, to ensure appropriate skull growth in the desired direction. The benefits of minimally invasive surgery include much shorter surgical times, much less blood loss, and very small, nearly invisible, incisions. Modern craniofacial centers should be able to offer both minimally invasive and open techniques for the care and treatment of their children.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Clayman MA, Murad GJ, Steele MH, et al. History of craniosynostosis surgery and the evolution of minimally invasive endoscopic techniques: the University of Florida experience. Ann Plast Surg 2007;58:285-7. [PubMed]
- Kaufman BA, Muszynski CA, Matthews A, et al. The circle of sagittal synostosis surgery. Semin Pediatr Neurol 2004;11:243-8. [PubMed]
- Mehta VA, Bettegowda C, Jallo GI, et al. The evolution of surgical management for craniosynostosis. Neurosurg Focus 2010;29:E5. [PubMed]
- Barone CM, Jimenez DF. Endoscopic craniectomy for early correction of craniosynostosis. Plast Reconstr Surg 1999;104:1965-73; discussion 1974-5.
- Jimenez DF, Barone CM, Cartwright CC, et al. Early management of craniosynostosis using endoscopic-assisted strip craniectomies and cranial orthotic molding therapy. Pediatrics 2002;110:97-104. [PubMed]
- Mackenzie KA, Davis C, Yang A, et al. Evolution of surgery for sagittal synostosis: the role of new technologies. J Craniofac Surg 2009;20:129-33. [PubMed]
- McCarthy JG, Warren SM, Bernstein J, et al. Parameters of care for craniosynostosis. Cleft Palate Craniofac J 2012;49 Suppl:1S-24S. [PubMed]
- Proctor MR. Endoscopic cranial suture release for the treatment of craniosynostosis--is it the future? J Craniofac Surg 2012;23:225-8. [PubMed]
- Stelnicki EJ. Endoscopic treatment of craniosynostosis. Atlas Oral Maxillofac Surg Clin North Am 2002;10:57-72. [PubMed]
- Warren SM, Proctor MR, Bartlett SP, et al. Parameters of care for craniosynostosis: craniofacial and neurologic surgery perspectives. Plast Reconstr Surg 2012;129:731-7. [PubMed]
- Cuschier A, Terblanche J. Laparoscopic cholecystectomy: evolution, not revolution. Surg Endosc 1990;4:125-6. [PubMed]
- Keith RG. Laparoscopic cholecystectomy: let us control the virus. Can J Surg 1990;33:435-6. [PubMed]
- Berry-Candelario J, Ridgway EB, Grondin RT, et al. Endoscope-assisted strip craniectomy and postoperative helmet therapy for treatment of craniosynostosis. Neurosurg Focus 2011;31:E5. [PubMed]
- David LR, Plikaitis CM, Couture D, et al. Outcome analysis of our first 75 spring-assisted surgeries for scaphocephaly. J Craniofac Surg 2010;21:3-9. [PubMed]
- Davis C, Windh P, Lauritzen CG. Spring expansion is influenced by cranial biomechanics. J Craniofac Surg 2010;21:843-6. [PubMed]
- Davis C, Lauritzen CG. The biomechanical characteristics of cranial sutures are altered by spring cranioplasty forces. Plast Reconstr Surg 2010;125:1111-8. [PubMed]
- de Faria Valle Dornelles R, Cardim VL, de Campos Fonseca Pinto AC, et al. Skull base cephalometric changes in cranial expansion by springs. J Craniofac Surg 2011;22:1496-501. [PubMed]
- Lauritzen CG, Davis C, Ivarsson A, et al. The evolving role of springs in craniofacial surgery: the first 100 clinical cases. Plast Reconstr Surg 2008;121:545-54. [PubMed]
- Tunçbilek G, Kaykçoğlu A, Bozkurt G, et al. Spring-mediated cranioplasty in patients with multiple-suture synostosis and cloverleaf skull deformity. J Craniofac Surg 2012;23:374-7. [PubMed]
- Jimenez DF, Barone CM. Endoscopic craniectomy for early surgical correction of sagittal craniosynostosis. J Neurosurg 1998;88:77-81. [PubMed]
- Jimenez DF, Barone CM. Endoscopic techniques for craniosynostosis. Atlas Oral Maxillofac Surg Clin North Am 2010;18:93-107. [PubMed]
- Chaichana KL, Jallo GI, Dorafshar AH, et al. Novel use of an ultrasonic bone-cutting device for endoscopic-assisted craniosynostosis surgery. Childs Nerv Syst 2013. [Epub ahead of print]. [PubMed]
- Jimenez DF, Barone CM, McGee ME, et al. Endoscopy-assisted wide-vertex craniectomy, barrel stave osteotomies, and postoperative helmet molding therapy in the management of sagittal suture craniosynostosis. J Neurosurg 2004;100:407-17. [PubMed]
- Ridgway EB, Berry-Candelario J, Grondin RT, et al. The management of sagittal synostosis using endoscopic suturectomy and postoperative helmet therapy. J Neurosurg Pediatr 2011;7:620-6. [PubMed]
- Meier PM, Goobie SM, DiNardo JA, et al. Endoscopic strip craniectomy in early infancy: the initial five years of anesthesia experience. Anesth Analg 2011;112:407-14. [PubMed]
- Jimenez DF, Barone CM, McGee ME. Design and care of helmets in postoperative craniosynostosis patients: our personal approach. Clin Plast Surg 2004;31:481-7. vii. [PubMed]
- Seymour-Dempsey K, Baumgartner JE, Teichgraeber JF, et al. Molding helmet therapy in the management of sagittal synostosis. J Craniofac Surg 2002;13:631-5. [PubMed]
- Marchac A, Arnaud E. Cranium and midface distraction osteogenesis: current practices, controversies, and future applications. J Craniofac Surg 2012;23:235-8. [PubMed]
- Oh TS, Ra YS, Hong SH, et al. Cranial compression using distractors in reverse fashion as an alternative method for correcting scaphocephaly in older patients. Pediatr Neurosurg 2013;49:1-10. [PubMed]
- Park DH, Yoon SH. The trans-sutural distraction osteogenesis for 22 cases of craniosynostosis: a new, easy, safe, and efficient method in craniosynostosis surgery. Pediatr Neurosurg 2011;47:167-75. [PubMed]
- Sargent LA, Griner D. Use of osteogenesis distractors in cloverleaf skull reconstruction. Ann Plast Surg 2013;70:546-8. [PubMed]
- Tellado MG, Lema A. Coronal suturectomy through minimal incisions and distraction osteogenesis are enough without other craniotomies for the treatment of plagiocephaly due to coronal synostosis. J Craniofac Surg 2009;20:1975-7. [PubMed]
- Jenkins GH, Smith NR, McNeely PD. Pancraniosynostosis following endoscope-assisted strip craniectomy and helmet orthosis for sagittal suture craniosynostosis in a nonsyndromic patient. J Neurosurg Pediatr 2013;12:77-9. [PubMed]
- Adamo MA, Pollack IF. A single-center experience with symptomatic postoperative calvarial growth restriction after extended strip craniectomy for sagittal craniosynostosis. J Neurosurg Pediatr 2010;5:131-5. [PubMed]
- Bastidas N, Mackay DD, Taylor JA, et al. Analysis of the long-term outcomes of nonsyndromic bicoronal synostosis. Plast Reconstr Surg 2012;130:877-83. [PubMed]
- Agrawal D, Steinbok P, Cochrane DD. Long-term anthropometric outcomes following surgery for isolated sagittal craniosynostosis. J Neurosurg 2006;105:357-60. [PubMed]
- Doumit GD, Papay FA, Moores N, et al. Management of Sagittal Synostosis: A Solution to Equipoise. J Craniofac Surg 2014. [Epub ahead of print]. [PubMed]
- Shah MN, Kane AA, Petersen JD, et al. Endoscopically assisted versus open repair of sagittal craniosynostosis: the St. Louis Children’s Hospital experience. J Neurosurg Pediatr 2011;8:165-70. [PubMed]
- van Veelen ML, Mathijssen IM. Spring-assisted correction of sagittal suture synostosis. Childs Nerv Syst 2012;28:1347-51. [PubMed]
- Keshavarzi S, Hayden MG, Ben-Haim S, et al. Variations of endoscopic and open repair of metopic craniosynostosis. J Craniofac Surg 2009;20:1439-44. [PubMed]
- Tan SP, Proctor MR, Mulliken JB, et al. Early frontofacial symmetry after correction of unilateral coronal synostosis: frontoorbital advancement vs endoscopic strip craniectomy and helmet therapy. J Craniofac Surg 2013;24:1190-4. [PubMed]
- Mesa JM, Fang F, Muraszko KM, et al. Reconstruction of unicoronal plagiocephaly with a hypercorrection surgical technique. Neurosurg Focus 2011;31:E4. [PubMed]
- Lwin CT, Richardson D, Duncan C, et al. Relapse in fronto-orbital advancement: a pilot study. J Craniofac Surg 2011;22:214-6. [PubMed]
- Maltese G, Tarnow P, Lindström A, et al. New objective measurement of forehead symmetry in unicoronal craniosynostosis - comparison between fronto-orbital advancement and forehead remodelling with a bone graft. J Plast Surg Hand Surg 2014;48:59-62. [PubMed]
- MacKinnon S, Proctor MR, Rogers GF, et al. Improving ophthalmic outcomes in children with unilateral coronal synostosis by treatment with endoscopic strip craniectomy and helmet therapy rather than fronto-orbital advancement. J AAPOS 2013;17:259-65. [PubMed]
- MacKinnon S, Rogers GF, Gregas M, et al. Treatment of unilateral coronal synostosis by endoscopic strip craniectomy or fronto-orbital advancement: Ophthalmologic findings. J AAPOS 2009;13:155-60. [PubMed]
- Melville H, Wang Y, Taub PJ, et al. Genetic basis of potential therapeutic strategies for craniosynostosis. Am J Med Genet A 2010;152A:3007-15. [PubMed]
- Tovetjärn R, Maltese G, Kölby L, et al. Spring-assisted cranioplasty for bicoronal synostosis. J Craniofac Surg 2012;23:977-81. [PubMed]
- de Jong T, van Veelen ML, Mathijssen IM. Spring-assisted posterior vault expansion in multisuture craniosynostosis. Childs Nerv Syst 2013;29:815-20. [PubMed]
- Goldstein JA, Paliga JT, Bailey RL, et al. Posterior vault distraction with midface distraction without osteotomy as a first stage for syndromic craniosynostosis. J Craniofac Surg 2013;24:1263-7. [PubMed]
- Nowinski D, Di Rocco F, Renier D, et al. Posterior cranial vault expansion in the treatment of craniosynostosis. Comparison of current techniques. Childs Nerv Syst 2012;28:1537-44. [PubMed]
- Arnaud E, Marchac A, Jeblaoui Y, et al. Spring-assisted posterior skull expansion without osteotomies. Childs Nerv Syst 2012;28:1545-9. [PubMed]
- Jimenez DF, Barone CM. Multiple-suture nonsyndromic craniosynostosis: early and effective management using endoscopic techniques. J Neurosurg Pediatr 2010;5:223-31. [PubMed]
- Meier PM, Guzman R, Erb TO. Endoscopic pediatric neurosurgery: implications for anesthesia. Paediatr Anaesth 2014;24:668-77. [PubMed]
- Stricker PA, Fiadjoe JE. Anesthesia for craniofacial surgery in infancy. Anesthesiol Clin 2014;32:215-35. [PubMed]
- Johnson JO, Jimenez DF, Barone CM. Blood loss after endoscopic strip craniectomy for craniosynostosis. J Neurosurg Anesthesiol 2000;12:60. [PubMed]
- Di Rocco C, Tamburrini G, Pietrini D. Blood sparing in craniosynostosis surgery. Semin Pediatr Neurol 2004;11:278-87. [PubMed]
- Naumann HL, Haberkern CM, Pietila KE, et al. Duration of exposure to cranial vault surgery: associations with neurodevelopment among children with single-suture craniosynostosis. Paediatr Anaesth 2012. [Epub ahead of print]. [PubMed]
- Abbott MM, Rogers GF, Proctor MR, et al. Cost of treating sagittal synostosis in the first year of life. J Craniofac Surg 2012;23:88-93. [PubMed]
- Vogel TW, Woo AS, Kane AA, et al. A comparison of costs associated with endoscope-assisted craniectomy versus open cranial vault repair for infants with sagittal synostosis. J Neurosurg Pediatr 2014;13:324-31. [PubMed]
- Kim D, Pryor LS, Broder K, et al. Comparison of open versus minimally invasive craniosynostosis procedures from the perspective of the parent. J Craniofac Surg 2008;19:128-31. [PubMed]
- Hashim PW, Patel A, Yang JF, et al. The effects of whole vault cranioplasty versus strip craniectomy on long-term neuropsychological outcomes in sagittal craniosynostosis. Plast Reconstr Surg 2014. [Epub ahead of print]. [PubMed]