
Clinical value of virtual touch tissue imaging quantification in diagnosis and treatment of congenital muscular torticollis in children
Introduction
Congenital muscular torticollis (CMT) refers to a neck deformity that is mainly caused by the contracture of sternocleidomastoid muscle (SCM). The typical clinical manifestation is that the head is biased toward the affected side and the mandible is rotated to the healthy side (1,2). The pathogenesis of CMT are generally considered to be related to the degeneration of SCM cells and interstitial hyperplasia/fibrosis (3). Clinically, a positive correlation has been observed between the hardness and fibrosis of CMT lesions. As a technique for elastography, the virtual touch tissue imaging quantification (VTIQ) technique can quantitatively evaluate the elasticity of SCM, assess the SCM lesions objectively, and determine the hardness of SCM (4). The pulsed sound beam reflected by the probe excites the tissue to produce tiny displacements, and then the shear wave velocity (SWV) during tissue displacement is calculated. SWV can quantitatively reflect the elastic characteristics of the tissues and the hardness of the reactive tissues (5). The lower the SWV, the better the tissue elasticity is and the lower the hardness is. On the contrary, the tissue is hard and the elasticity is poor in severe fibrotic tissues (6). In this study, VTIQ was used to quantitatively analyze the hardness of bilateral SCM in CMT children, and the value of VTIQ in the diagnosis and treatment of CMT was further evaluated in CMT children who received non-surgical treatment or surgery.
Methods
Subjects
Sixty-two CMT outpatient children diagnosed with CMT were recruited from the clinics between January 2018 and June 2019. There were 43 males and 19 females with the mean age of 5.7±0.9 months (range, 16 days to 1 year). Children who underwent non-surgical massage were followed up. Twenty-three CMT children who underwent surgery in our hospital in the same period were also recruited. There 15 males and 8 females with the mean age of 5.0±3.5 years (range, 1–12 years). In all the patients, cervical X-ray and ophthalmologic examination were performed to exclude the skeletal torticollis, and the immune system disorder, blood system disorder and other congenital malformations were also excluded. This study was approved by the Institutional Review Board of Second Affiliated Hospital of Wenzhou Medical University (No. L-2019-13).
CMT was diagnosed according to the following criteria: (I) the typical clinical manifestations include that the head is biased to the affected side and the mandible is rotated to the healthy side; (II) the range of neck motion is limited; (III) there is hard or palpable mass at the neck; (IV) ultrasound examination shows focal or diffuse thickening of the affected SCM as compared to the adjacent normal tissue or contralateral SCM.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (I) children were diagnosed with CMT; (II) all the children received ultrasound examination by the same experienced physicians in our department; (III) CMT patients who received non-surgical treatment in the present study were initially diagnosed with CMT in our hospital and did not receive prior treatment; (IV) in CMT patients who recovered during the follow-up period, ultrasound examination showed the thickness of SCM returned to normal, regardless the echoes on ultrasonography; (V) patients who underwent surgical treatment received pre-operative ultrasound examination.
The exclusion criteria were as follows: (I) the torticollis was bone disease or ocular disease, or postural torticollis/spastic torticollis was diagnosed; (II) patients did not receive follow-up by ultrasonography; (III) the thickness of SCM was still abnormal on ultrasonography during the post-operative follow-up period; (IV) patients had other diseases (such as immune disease or hematological disease); (V) patients had other congenital deformities.
Instruments and methods
The patients received ultrasonography by using the SIEMENS ACUSON Oxana 2 ultrasound system with a probe at 4.0–9.0 MHz and built-in VTIQ imaging software. The child lied in a supine position with his head towards one side. For crying children who could not cooperate with the examinations, oral 10% chloral hydrate was administered at 0.5 mL/kg for sedation. Firstly, conventional two-dimensional ultrasound and color Doppler ultrasound examinations were performed at bilateral SCMs, and the shape, size, internal echo and blood flow of the lesioned SCM were determined. Subsequently, VTIQ was done at the long axis of the SCM. The region of interest (ROI) was defined at the thickest site of bilateral SCM. The SWV of bilateral SCMs was measured at the same level. Each measurement was performed 6 times, and an average was calculated. If the child had a short neck, the SWV should be measured repeatedly to improve the accuracy.
Statistical analysis
Statistical analysis was performed using SPSS version 22.0 (Statistical Product and Service Solutions, NY, USA). The quantitative data are expressed as mean ± standard deviation (
Results
SWV of bilateral SCMs in 62 CMT patients before and after non-surgical treatment
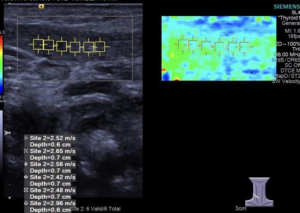
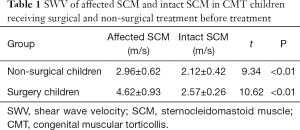
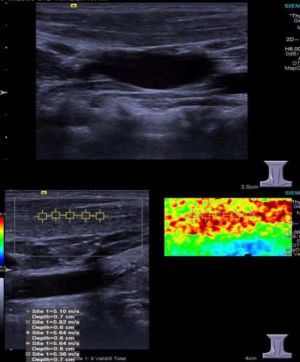
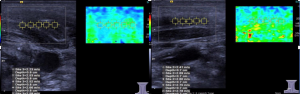
The elastic ultrasound images of the intact SCM in 62 CMT outpatients showed a uniform green with a small amount of blue (Figure 1). The mean SWV of intact SCM was 2.12±0.42 m/s. Ultrasound-elastic images of SCM thickening or mass at the affected side showed a mixed distribution of green and blue (Figure 2), and the SWV of affected SCM was 2.96±0.62 m/s, which was significantly higher than that of the intact SCM before massage (P<0.01).
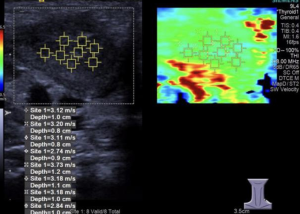
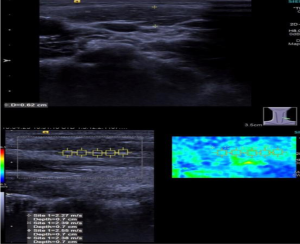
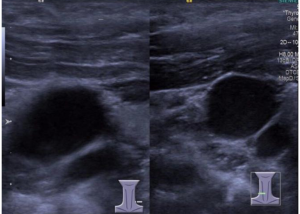
SWV of bilateral SCMs in 23 CMT controls before surgery
In 23 patients undergoing surgical treatment, the mean SWV of intact SCM was 2.57±0.26 m/s (Figure 3) and the mean SWV of affected SCM was 4.62±0.93 m/s, showing significant difference between them (Figure 4). In addition, the mean SWV of affected SCM was significantly higher than that of 62 outpatients (P<0.01) (Table 1).
Full table
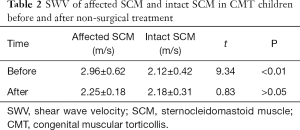
SWV of bilateral SCMs in 62 CMT children after non-surgical treatment
In 62 children who underwent non-surgical massage, the conventional ultrasound images of affected SCM showed the thinning of SCM or a reduction of local mass and a local increase in the echo (Figure 5). The mean SWV of affected SCM in 62 CMT children was 2.25±0.18 m/s, and the mean SWV of intact SCM was 2.18±0.31 m/s after massage (Figure 6, Table 2) There was no significant difference in the SWV between affected SCM and intact SCM after massage (P>0.05). The average SWV after massage was markedly lower than that before treatment (P<0.01).
Full table
Discussion
CMT is one of the most common congenital musculoskeletal diseases in newborns and infants, with an incidence of 0.3–1.9% (7). The main clinical manifestations include the head being biased to the affected side after birth and presence of a hard tumor-like mass at the affected SCM. If not treated, the head may be inclined to the affected side, and the face inclined to the intact side. The patients will develop forward tilt, atrophy of the affected SCM, and asymmetrical facial development and bilateral eye splitting. Finally, these may cause other secondary malformations, such as cervical scoliosis, vertebral wedge deformation, and strabismus, seriously affecting the normal development of infants and young children (8). Ultrasound is a main tool for the diagnosis of CMT. Conventional high-frequency ultrasound diagnosis can accurately detect the thickness of SCM. The ultrasound of CMT is divided into local mass and uniform thickening. On ultrasound examination, the affected SCM showed thickening at middle to lower part, and the internal muscular fibers became thickened with enhanced echoes; once mass-like echoes were present, heterogeneous hypointensity was observed in the mass, and the bigger mass could display mixed echoes. Pathologically, over-expression of type I, III, and IV collagen fibers has been found in the stroma, resulting in the fibrosis of SCM in CMT patients (9). According to the degree of SCM fibrosis on ultrasonography in CMT children, Tatli et al. (10) classified CMT as follows: type I, thickening of affected SCM, uneven echo or normal, peripheral muscle texture clear; type II, the affected SCM is diffuse in the normal muscle texture background. Strong echo: type III, a cluttered strong echo for the whole SCM, normal muscle texture firefighting: type IV, the whole SCM has a banded strong echo and the normal muscle texture disappears. However, the classification based on conventional ultrasound findings is greatly influenced by the resolution of ultrasound system and the subjective assessment of the sonographer. Thus, it is not an objective examination, has a poor reliability is poor, and can’t determine the degree of the lesion. Shi et al. (11) found that there was a positive correlation between tissue hardness and tissue fibrosis, and the elasticity of SCM is a more effective and objective indicator in the diagnosis of CMT (12). With the development of elastographic technology, the VTIQ technique can more objectively determine the softness and hardness of the lesion. VTIQ is a real-time shear wave elastography (SWE) based on the acoustic radiation. The pulsed sound beam reflected by the probe excites the tissue to produce tiny displacements, and then the SWV during tissue displacement is calculated. SWV can quantitatively reflect the elastic characteristics of the tissues and the hardness of the reactive tissues (5). The elastographic technique can dynamically assess the tissue elasticity as well as the elasticity as a response to counterpressure (hard tissue has lower elasticity and soft tissue has higher elasticity). The lower the SWV, the better the tissue elasticity is and the lower the hardness is. On the contrary, the tissue is hard and the elasticity is poor. In addition, the severity of fibrosis is closely related to the elasticity: the more severe the fibrosis, the harder the tissue is (6). Therefore, the VTIQ technique can be used to measure the SWV of bilateral SCMs in children. In this study, VTIQ was used to measure the mean SWV of bilateral SCMs in CMT children. The affected SCM and intact SCM were compared in the same child. The SWV of the affected side was significantly greater than that of the healthy side, which was consistent with previously reported (13-15). This indicates that the measurement of SWV of the affected SCM and contralateral SCM by VTIQ can be used in the diagnosis of CMT in children. At the same time, SWV as a quantitative index may objectively evaluate the degree of fibrosis of SCM: the higher the degree of fibrosis, the greater the SWV is.
Currently, CMT is managed with non-surgical and surgical treatments. If the diagnosis and non-surgical treatment are performed timely, the cure rate can reach as high as 80% and the prognosis is also favorable (16,17). After non-surgical treatment, the therapeutic efficacy was assed according to the criteria for the assessment of recovery in patients (18). In CMT patients, functional recovery after treatment is scored based on following conditions: head and neck rotation, lateral deviation and facial deformity. However, these evaluations and scorings are more subjective and there are no quantitative parameters. The characteristics of CMT on high-frequency ultrasonography are different with age and the progression of treatment. Luan et al. divided SCM into four types according to the echogenicity and intensity of SCM texture on ultrasound examination (19). However, the conventional ultrasound is a subjective examination in the assessment of SCM echoes, which is usually dependent on the experience of the examiner. In this study, the mean SWV of SCM in 62 CMT children was detected before and after massage. Results showed the SWV of affected SCM after treatment was significantly lower than that before treatment. This indicates that the hardness of affected SCM after massage reduces, suggesting the therapeutic effectiveness. There was no significant difference in the SWV of bilateral SCMs in CMT children after massage, indicating that the fibrosis of affected SCM is improved. Therefore, VTIQ provides a quantitative tool for the assessment of hardness of SCM and can be employed to monitor and follow up the efficacy of non-surgical treatment for CMT in children.
Currently, surgical intervention is recommended for the treatment of CMT in children aged 1–4 years (20). Generally, surgery is performed if non-surgical treatment achieves a poor response or the patients are relatively old. Thus, patients in the surgery group were older in our study. There is evidence showing that the CMT in children aged as young as 8 months can also be managed with surgical intervention (21); the therapeutic efficacy of non-surgical treatment for more than 6 months is unfavorable because the head tilt and muscle tightening remained (21). Thus, some clinicians recommend that surgery should be treated as soon as possible, especially for children younger than 1 year. However, the application of surgical intervention is mainly dependent on the clinical manifestations and physical examination of SCM in the CMT children. In the present study, 23 patients who underwent surgery were recruited as controls. The mean SWV of affected SCM was significantly higher than that of intact SCM. Moreover, the mean pre-treatment SWV of affected SCM in 23 patients was markedly higher than that of 62 CMT patients receiving non-surgical treatment (P<0.01). Of note, the degree of fibrosis will gradually increase with age and may even cause severe deformity of the head and face. If the average SWV of affected SCM remains unchanged after treatment, surgical intervention should be performed as soon as possible, regardless of age, or the delayed treatment will worsen the prognosis. Thus, VTIQ has a role in the assessment of therapeutic efficacy in children with CMT because it can provide information to guide the clinical treatment of CMT.
VTIQ is of great significance in the early diagnosis and treatment of CMT, but there were limitations in the present study: (I) cases of non-surgical treatment are not obvious; (II) the number of CMT patients receiving surgical intervention was still small and there were no pathological results. Only the surgeon observed the muscle atrophy, degeneration and fibrosis according to the operation, and did not pass the pathological diagnosis and the SWV value of VTIQ. The critical value of surgical and non-surgical treatments is needed to be further studied in the sample to determine the critical value to choose the appropriate surgical treatment opportunity; (III) currently, there is no comprehensive evaluation system which integrates the VTIQ technique and clinical assessment of therapeutic efficacy. It is necessary to confirmed our findings in more studies with large sample size and long follow-up.
VTIQ can measure the SWV of SCM to quantitatively and objectively evaluate the degree of fibrosis of SCM in CMT children. Thus, VTIQ may be employed in the diagnosis of CMT and in the evaluation of post-treatment efficacy which are beneficial for the clinical decision-making.
Acknowledgments
Funding: This study was supported by the Project of Science and Technology Bureau of Wenzhou City (Y20170831).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of Second Affiliated Hospital of Wenzhou Medical University (No. L-2019-13).
References
- Kaplan SL, Coulter C, Sargent B. Physical Therapy Management of Congenital Muscular Torticollis: A 2018 Evidence-Based Clinical Practice Guideline From the APTA Academy of Pediatric Physical Therapy. Pediatr Phys Ther 2018;30:240-90. [Crossref] [PubMed]
- Tessmer A, Mooney P, Pelland L. A developmental perspective on congenital muscular torticollis: a critical appraisal of the evidence. Pediatr Phys Ther 2010;22:378-83. [Crossref] [PubMed]
- Ryu JH, Kim DW, Kim SH, et al. Factors Correlating Outcome in Young Infants With Congenital Muscular Torticollis. Can Assoc Radiol J 2016;67:82-7. [Crossref] [PubMed]
- Xiao P, Zhu S, Liu R, et al. Evaluation of sternocleidomastoid muscle fibrosis after radiotherapy for nasopharyngeal carcinoma. Chin J Ultra Imag 2016;25:159-62.
- Piscaglia F, Salvatore V, Di Donato R, et al. Accuracy of VirtualTouch Acoustic Radiation Force Impulse (ARFI) imaging for the diagnosis of cirrhosis during liver ultrasonography. Ultraschall Med 2011;32:167-75. [Crossref] [PubMed]
- Zhang YF, Xu HX, He Y, et al. Virtual touch tissue quantification of acoustic radiation force impulse: a new ultrasound elastic imaging in the diagnosis of thyroid nodules. PLoS One 2012;7:e49094. [Crossref] [PubMed]
- Do TT. Congenital muscular torticollis: current concepts and review of treatment. Curr Opin Pediatr 2006;18:26-9. [PubMed]
- Li Z, Wang H, Ji S. Practical pediatric surgery. Beijing: People’s Medical Publishing House, 1997.
- Kang Y. Etiology and pathology of muscular torticollis in infants. Chin J Plast Surg 2008;24:490-2.
- Tatli B, Aydinli N, Caliskan M, et al. Congenital muscular torticollis: evaluation and classification. Pediatr Neurol 2006;34:41-4. [Crossref] [PubMed]
- Shi X, Ai H, Wang J. Preliminary application of ultrasound real-time tissue elastography in diffuse thyroid diseases. Chin J Ultra Imag 2011;20:515-8.
- Ye F, Feng Q. Diagnostic value of ultrasound elastography and conventional ultrasound in congenital muscular torticula. J Clinical Ultra 2013;15:862-4.
- Hong SK, Song JW, Woo SB, et al. Clinical Usefulness of Sonoelastography in Infants With Congenital Muscular Torticollis. Ann Rehabil Med 2016;40:28-33. [Crossref] [PubMed]
- Xu N, Xia B, Tang N, et al. Application of shear wave elastography of sternocleidomastoid in early diagnosis of congenital muscular torticollis. Chin J Ultra 2018;15:111-8.
- Li X, Gao H, Liu Q, et al. Application of real-time tissue elastography in early diagnosis and treatment of muscular torticollis in infants. Chin J Ultra Imag 2016;25:888-91.
- Wang Q, Wang J, Wang J. Application value of ultrasound in children with muscular torticola. Chin Med Clin J 2014;26:1283-5.
- Lee K, Chung E, Lee BH. A comparison of outcomes of asymmetry in infants with congenital muscular torticollis according to age upon starting treatment. J Phys Ther Sci 2017;29:543-7. [Crossref] [PubMed]
- Sun C. Clinical disease diagnosis based on cure and improvement criteria. Beijing: People’s Military Medical Press, 2002:404-5.
- Luan Y, Yin L, Wu Y, et al. Application value of ultrasonic quadrature in diagnosis of congenital muscular torticula. Clin Med 2014;16:827-9.
- Lou Y. Congenital muscular torticollis operation, most suitable for 1~5 years old. Jiangsu Health Care 2017;22:9.
- Liu Y, Zhou G, Fan Y. Early surgical treatment of congenital muscular torticula under ultrasound guidance. Henan J Surg 2007;13:10-1.


