Neonatal transport metrics and quality improvement in a regional transport service
Introduction
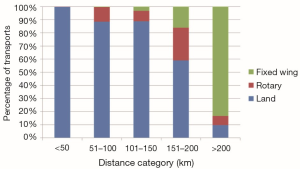
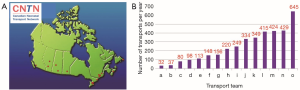
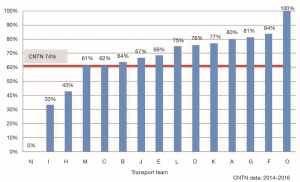
Pediatric critical care transport by specialized teams results in improved outcomes compared with transport by non-specialized teams (1) with decreased unplanned events such as airway-related events, cardiopulmonary arrest, sustained hypotension, and loss of crucial intravenous access; and lower mortality rates (2). Neonatal transports constitute a subgroup of pediatric critical care transports that rely on the expert skills of specialized neonatal transport teams (NTTs) and efficient systems to provide safe and timely transport to tertiary centers. Review of the demographics for NTTs across Canada shows that there are wide variations in the volume of transports, mode of transport and team composition (Figures 1-3). In the United States, Karlsen et al. reported wide variation in many aspects of neonatal transport including transport training and certification, use of protocols to guide transport care, and quality assurance activities (3).
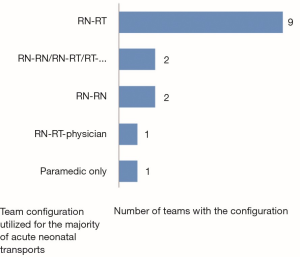
Whether these variations in the demographics of transport teams lead to differences in performance and outcomes is unclear. For team composition, comparison of transport teams with physicians versus teams without physicians have not shown consistent advantages of one team over the other. Leslie et al. showed that although nurse practitioner teams took longer to stabilize infants compared with physician teams, the patient’s physiological condition was improved as measured by the changes in temperature and oxygen saturation when the nurse practitioner team was utilized (4). King reported the effect on patient outcomes after change of team composition from nurse-physician team to a nurse only team in neonatal and pediatric transports (5). There were no deaths during transport in both groups, but team response times were significantly shorter for the nurse-only team. A cost analysis has shown that the nurse (RN)/RN model is usually the least costly (6).
Neonatal transport programs require a major investment of financial and human resources for specialized equipment and in the advanced training of personnel. Transport programs have wide variation in processes and practices which are costly to maintain, thus benchmarking of the performance of transport programs is imperative to evaluate the quality of care and identify opportunities for improvement. The care delivered in the transport environment is distinct from the neonatal intensive care unit (NICU), and significantly affected by technical and logistical issues such as equipment, NTT availability, and travel distance. Thus, it is essential to factor in these technical and logistical issues during the interpretation of transport quality indicators.
The American Academy of Pediatrics (AAP) Section on Transport Medicine, Canadian Paediatric Society, and transport experts in the UK have strongly recommended the development of benchmarking and standards for transport performance (7-9). However, quality metrics for neonatal/pediatric transport are only recently being developed (10) and where indicators exist; there is no consensus on the reference standards to use to evaluate the performance of transport programs (11).
Previous reports of quality metrics in pediatrics have included both neonatal and pediatric transports; but the neonatal population has unique considerations from that of older pediatric patients. Focusing on neonatal transports, this review aims to outline the important quality metrics that can be used for benchmarking, and important factors to consider when utilizing these metrics. To demonstrate the use of these metrics for quality improvement, the experience of the neonatal transport program based at a quaternary children’s hospital, the Hospital for Sick Children in Toronto, Canada will be described.
Quality metrics for neonatal transport
The Canadian Neonatal Transport Network (CNTN) was founded in June 2013 and is based at the Hospital for Sick Children. The primary goal of the CNTN was to develop a national neonatal transport database to allow benchmarking and improve quality of care and outcomes. The CNTN includes all of the 16 NTTs in Canada who conduct approximately 5,000 neonatal interfacility transports annually and enter data on their transports into a common database.
Quality metrics for the CNTN were defined shortly after the inception of the CNTN during the development of the CNTN database. The potential list of metrics was generated following a review of the literature and metrics proposed by other neonatal/pediatric transport groups (7,11,12). A face to face meeting with the medical director and/or manager representative(s) from all 16 neonatal teams occurred in Oct 2013 to develop standardized quality metrics. The final list of metrics was determined by national consensus utilizing the nominal group technique (13).
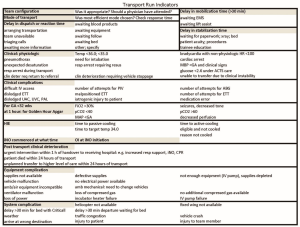
The Institute of Medicine’s domains of quality (14) were utilized to categorize the indicators as these domains were deemed highly relevant for evaluation of transport programs. The six domains and representative metrics in neonatal transport adopted by the CNTN are compared with those utilized by other programs in Table 1. Review of this table demonstrates that many of the metrics are consistent across the different programs which validate their importance and acceptance.

Full table
Expanding the scope of work by NTTs to our obstetrical communities
Maternal transfer to an appropriate facility, is one of four high-evidence based practices during the perinatal management of neonates born at <32 weeks gestational age (GA) shown to reduce mortality by 18% without an increase in severe morbidity (16). Canadian national guidelines recommend that deliveries at <32 weeks GA occur in a high-risk perinatal center (17). This recommendation is based on improved outcomes for infants born at high-risk obstetrical sites compared with those born at non-high-risk obstetrical sites and transported to tertiary neonatal units after delivery (18). Despite these recommendations, 28% of deliveries of infants of GA <29 weeks in Canada occur in a non-perinatal (outborn) centre (19) and outborn deliveries in Canada remain one of the highest internationally compared with rates of 15% in Australia (20) and 16% in the United States (21). Perinatal centres and transport programs can have an important role in effecting a decrease in outborn deliveries. An obstetric indicator, number of deliveries at GA <32 weeks in non-tertiary centers is among the CNTN quality indicators. Inclusion of this metric highlights the importance of promoting and advocating for maternal transfers for preterm deliveries in order to improve outcomes. This is in the quality domain of equity to ensure that mothers in all regions can have access to the appropriate level of care for best neonatal outcomes. In addition, modifiable obstetrical interventions which have been shown to improve neonatal outcomes such as administration of antenatal steroids, magnesium sulfate and delayed cord clamping for preterm deliveries is important to promote in non-tertiary centers (16,22,23).
NTTs have a key leadership role in their region among the non-tertiary sites. Tracking of preterm deliveries <32 weeks at non-tertiary sites with feedback to their non-tertiary sites to promote maternal transfers may be one of the most impactful interventions to improve neonatal outcomes. The New South Wales region of Australia has been successful in the reduction of non-tertiary deliveries where statewide coordinated strategies including a perinatal telephone advice line to optimize in utero transfers were effective in reducing non-tertiary hospital births at GA <29 weeks from 19.7% to 14.9% (20). In the greater Cincinnati area, perinatal outreach education to providers at non-specialty perinatal centers promoted maternal transfer at <32 weeks to decrease outborn deliveries from 25% to 11.8% between 1995–1997 vs. 2003–2007 (21).
Methodological considerations for benchmarking
Standardize definitions, especially transport times
Karlsen demonstrated the importance of standardized definitions in her report of a survey of American transport teams, as she found that data quality was hindered by inconsistency in the definitions of the variables and indicators collected; and data quality was insufficient to allow benchmarking for comparisons across programs (3).
The nomenclature and descriptors for key transport time metrics that are used by different transport services (11,15,24) are summarized in Table 2. Transport times which are the mainstay of measurement for the quality domains of timeliness and efficiency are bogged down by inconsistencies in their definitions in publications and reports (25). The duration of time for care provided by the transport team at the referral site has been labelled variably as scene time (10) and stabilization time (11). The duration of time for the transport team to depart from their home site has been labelled as response time (26) or more commonly, mobilization time (12,15). There are commonalities in the choice of metrics and definitions among the teams, but future reports and publications should strive to align nomenclature and descriptors with those summarized in Table 2.
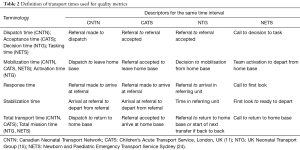
Full table
Once the definitions of transport times have been standardized, the next challenge is in the determination of reference standards for benchmarking as large variations have been reported (4,24,27-31). The Infant Transport Team of British Columbia published their standards for transport times, with ‘response’ times of 15 min for transport requests of very unstable patients by land and 1 hour by air (26). However, their definition of ‘response’ time was in fact mobilization time as defined by other transport systems (see Table 2). Moreover, these recommended standards have not been tested for validity and generalizability.
The optimal stabilization time is not known and it is recognized that shorter stabilization times which are targeted in the adult population (32), do not result in better outcomes for neonates (2,33). Neonatal patients have longer stabilization times compared with pediatric patients (median stabilization time of 80 vs. 45 min) (31); and neonates with a higher severity of illness (defined as ventilated and on inotropes) have longer stabilization times compared with non-ventilated neonates (median stabilization time 125 vs. 63 min) (31).
Rather than minimization of stabilization times, a major goal is to expedite (I) the arrival of the NTT at the referral site (response time) so that the infant can benefit from their advanced skills; and (II) the arrival of the infant at the destination hospital for definitive care (34). However, from an evaluation of performance perspective, these times must be corrected for distance, weather and available modes of transport, as these factors are beyond the control of transport teams (24).
Benchmarks for transport times can be determined by service standards, e.g., land vehicle response time of 15 min by paramedic services for critical transports; or expert consensus. However, benchmarks can be derived by data using the regional performance such as national medians and interquartile ranges for continuous variables and odds ratios with 95% confidence intervals for proportions. The Ground and Air Medical qUality Transport (GAMUT) QI collaborative uses the Achievable Benchmarks of Care (ABC) method (35) to determine reference standards. The ABC method establishes the performance level consistently being attained by the best participants that account for at least 10% of the overall population. A major advantage of this method is that it allows the comparison of performance between groups of varying sizes.
Reporting of low frequency events
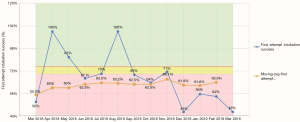
Some of the teams in Canada have low transport volumes, or some of the indicators involve a small number of cases even for high volume teams. An example of a low frequency event is endotracheal intubation which has decreased in neonatology due to the preference for non-invasive ventilation as the primary mode of respiratory support even for extremely premature infants. For infrequent events, monthly rates may have major fluctuations even with small changes in the number of events, and true trends may be difficult to visualize. A clearer report of the changes in rates over time can be visualized using the moving average. See Figure 4 for rates for first attempt intubation shown by month and by 12-month moving average using hypothetical data. This example demonstrates how the format of data reports can have a major influence on the utility of the data. In addition, any comparative analysis of indicators should adjust for the volume of service for low frequency events.
Ensure comparison of similar populations
The populations being analyzed need to be clearly defined as different populations can have major differences in outcomes. For example, we need to distinguish between interfacility transports compared with on-scene transports; between transports to a higher level of care compared with lateral or return transfers; between neonates that are admitted to tertiary sites compared to non-tertiary sites; and between neonates that are only admitted to intensive care units compared to all units. For this latter comparator, the neonatology literature demonstrated that mortality rates can be significantly underreported if only patients surviving to NICU admission are included compared to all deliveries which include a significant proportion of delivery room deaths (36).
Another inconsistency in the populations analyzed is in the definition of a neonate, which has not been well standardized across reports. For example, GAMUT utilizes age <29 days (12), whereas CNTN utilizes corrected GA up to 44 weeks for preterm infants.
In order to ensure standardization of definitions and study populations for benchmarking, a robust method would be to collect raw data from the multiple comparator sites utilizing a common database, and these data sent to a central site where the analyst can standardize definitions and populations. The ability to utilize one common database for all Canadian NTTs is one of the strengths of the CNTN database; whereas limitations of other databases that rely on entry of aggregate data by individual sites (12,15), is that definitions or populations maybe subjectively determined and thus less standardized, even if the numerators and denominators are objectively defined.
Customized selection of quality metrics
Many of the transport metrics are relevant for transports for all populations. However, the benchmarks for some, such as stabilization time will require adjustment based on age group as neonatal transports have been shown to have much longer stabilization times compared with pediatric transports (31).
GAMUT services transports of all ages and has proposed 27 quality metrics among which 17 were relevant for neonates (12). This highlights the importance of customization of quality metrics based on the age of the population, and that neonate-specific metrics should be further delineated.
One of the conditions that are more common among neonates who are transported is hypoxic ischemic encephalopathy (HIE). For neonates with HIE who are eligible for therapeutic hypothermia (TH), NTTs have a vital role in the timely initiation of TH within 6 hours of birth in order to improve outcomes (37). This has been recognized by NTTs and timely initiation of TH has been included as a quality indicator by the CNTN and Neonatal Transport Group (see Table 1).
There are several neonatal conditions with best practice standards that can be utilized to set benchmarks for the neonatal transported population. The care of preterm infants during the “Golden Hour” after delivery can be optimized to minimize their risk of intraventricular hemorrhage (IVH), especially since the risk of IVH is greater in neonates born in non-tertiary centers compared with those born in tertiary centers (18). Prevention of hypocarbia or hypercarbia, and avoidance of excessive fluid boluses are two important practices to target as metrics for NTTs which can decrease the risk of IVH (38). Another potential neonatal quality metric is to minimize stabilization and NICU admission times to be shorter than the typical times for neonates who have time sensitive conditions such as duct dependent cardiac lesions or surgical emergencies due to bilious vomiting or intestinal perforation.
Risk adjustment of metrics for severity of illness—an ongoing challenge
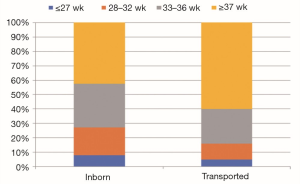
Neonates transported to NICUs differ from neonates born in perinatal centers in demographic characteristics such as GA as shown in Figure 5 and most responsible problem as shown in Table 3. Due to the wide heterogeneity in conditions and varying severity of illness among neonatal transports, an objective and reliable tool to measure severity of illness is required to allow risk adjustment for comparison of outcomes. However, this has been difficult to achieve and a major gap exists in this area.
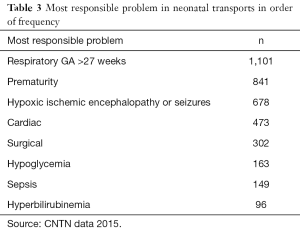
Full table
Due to the heterogeneity of conditions, a physiology based score based on objective parameters prior to NTT interventions would be most pertinent. The most commonly utilized measure of severity of illness in neonatal transport has been the transport risk index of physiologic stability (TRIPS) score (39). The TRIPS score was developed with the purpose to assess changes in patient status as a result of the transport process, and a worsening in the TRIPS score has been associated with increased mortality. Higher TRIPS scores have been associated with an increase in 7-day mortality and severe IVH risk.
The individual components of the TRIPS score represent physiologic parameters: temperature, blood pressure, respiratory status and response to noxious stimuli. Changes in these components can be a proxy for improvement or deterioration in clinical status. The change in TRIPS score may have face validity as a measure of quality of care. While these parameters may be modifiable with clinical interventions in some cases; in other cases, the changes in TRIPS scores may not necessarily be due to quality of care but rather due to non-preventable clinical deterioration. To account for changes in the severity of illness scores such as the TRIPS score due to factors beyond quality of care, a group from California are utilizing the Quality Change Point 10th percentile from their network to evaluate the quality of care provided by the transport team (40). For the TRIPS score, the narrow spectrum of values utilized to derive the score require further review to consider different blood pressure parameters for varying GAs.
There are other severity of illness measures that are not included in the TRIPS score, such as level of respiratory support, fractional inspired concentration of oxygen, and hemodynamic support; that have been utilized individually or in combination with other factors as measures of severity of illness among transported patients (31,41-44). These additional parameters require further study through comparison with TRIPS scores and association with outcomes but do have potential utility due to ease of use.
The mortality index for neonatal transportation (MINT) score has been shown to correlate with mortality and was proposed as a measure of severity of illness which can assist with effective triage at the time of the first telephone contact by the referring hospital with the transport team (42). This early determination of severity of illness can help decide which infants may benefit from the presence of a physician or a more timely response. However, its use has not been widely adopted due to the large number of transports with missing data for 2 of the score’s 7 main components (paO2 and pH) which require the availability of an arterial blood gas measurement.
It is also important to recognize that some of the metrics should take into account patient demographics that increase baseline risk such as GA for hypothermia, intubation success rates, and PIV insertion success rates; and distance as an important determinant of risk for hypothermia and time to target temperature for TH.
Utilization of quality metrics
A major purpose of transport databases is to generate reports which can be used by teams to drive quality improvement. Benchmarking of performance can guide how to target funding and educational efforts. Several regions and programs are currently utilizing these metrics for benchmarking and quality improvement.
The Pediatric Intensive Care Audit Network (45) and United Kingdom Neonatal Transport Group (15) have been utilizing their databases to compare activity and severity of illness, which has provided support for service development and procurement of new equipment.
Internationally, more than 350 transport programs including adult, pediatric and neonatal populations submit their summary data to the Ground and Air Medical qUality Transport (GAMUT) database (12). The GAMUT database provides a basis for transport teams to track, report and analyze their team activity and compare them with other teams world-wide. Use of timely comparator reports such as those generated by GAMUT can promote review of local data, and increase dialogue and sharing of practices with other programs.
Within Canada, the CNTN database collects granular data from all 16 NTTs in Canada onto a customized common database which provides a rich source of data for reporting and benchmarking. A site reporting application is available to all NTTs to generate local data reports in real time. This application is being utilized at SickKids to generate reports which are used to conduct daily reviews of runs that have occurred in the previous 24 hours with front line clinicians. A focus of the review is to audit the accuracy and completeness of data collection, and review metrics to compare with local program and national benchmarks. The metrics reviewed during these run reviews are summarized in Figure 6. This regular audit and feedback process enhances front line NTT engagement through a better understanding of how the data are used to improve processes and outcomes. At SickKids, data are collected prospectively in real time by front line transport team members and entered onto the CNTN database as part of their routine documentation at the end of their transport run. This direct involvement in data entry with the audit process during run reviews rather than having non-clinical data abstractors enter the data retrospectively, promotes data accuracy and completeness. The CNTN quality metrics are being utilized by the HSC NTT medical directors and managers on a monthly basis to track team performance, identify areas for improvement, and evaluate changes in outcomes over time after implementation of interventions.
Within the CNTN, the tracking of data has provided an impetus for the sharing of best practices. CNTN conducts regular web conferences with all 16 NTTs in Canada, where the quality metrics are reviewed. After review of the metrics, the topics of highest relevance and importance are chosen by CNTN members for further discussion. Transport teams that have previously worked in silos are able to utilize these comparisons to identify areas of strength and share best practices; and identify areas in need for improvement to help focus quality improvement efforts. During a recent CNTN web conference, we focused on TH in transport where we presented data on national variations in the time to target temperature after initiation of TH (see Figure 7). We shared national practices including the recent implementation of the cooling blanket in transport by 2 teams, management of cases with mild encephalopathy, and guidelines for anticonvulsant therapy. During another web conference, intubation success rates were compared nationally which led to the sharing of practices for training in endotracheal intubation.
Regional databases can be adopted by administrative advisory bodies to measure resource allocation and evaluate practices. Many of the CNTN indicators have been adopted by the Ontario Provincial Council for Maternal and Child Health as quality indicators to allow tracking of quality of care and resource utilization at a provincial level. These indicators are being utilized to monitor changes after implementation of quality improvement initiatives, for service accountability, and strategic planning and system monitoring. For example, review of metrics on land vehicle response times for transport teams identified a major discrepancy among teams in Ontario. This data provided strong support for a proposal submitted to our ministry for dedicated land ambulances for each of the teams in Ontario (46).
Summary and future directions
The need for benchmarking in neonatal transport is universally accepted. The recommended quality metrics for neonatal transport are consistent across reports and utilize the framework for domains of quality by the Institute of Medicine. The systems indicators can be utilized by all age groups; whereas clinical indicators require customization for the neonatal population. Metrics tracked by NTTs should include preterm deliveries in non-tertiary centers in their regions, as NTTs have a key leadership role to promote maternal transfers including audit and feedback to non-tertiary obstetrical sites.
There is a need for centralized data collection or utilization of common databases to allow standardation of definitions and populations across regions and internationally. While specific regions have centralized databases, improved harmonization of definitions, populations and indicators across regions is required to broaden the net for collaboration. The barriers to this collaboration include limited resources to enter data and funding to hire analysts for real time data management.
To support valid comparisons for benchmarking, further work is required to determine reference standards for benchmarking regionally and internationally; and the development of easy to apply risk adjustment scores to assist with triaging and comparison of outcomes. Metrics for specific conditions commonly managed in neonatal transport such as that currently utilized for timely initiation of TH in HIE require further derivation and implementation.
Significant progress has been made in the development of databases and quality metrics in neonatal transport. In order to achieve the maximal return from these efforts, the data must be utilized to generate meaningful reports to drive and evaluate improvement. The focus of future work should be to develop real time benchmarking reports that are easy to access by all teams and are visually impactful; followed by incentives to ensure that transport programs are continually reviewing their metrics; then the provision of a venue to ensure regular dialogue with other teams. These initiatives will set the momentum to engage teams in continuous quality improvement where current best practices are shared, and new interventions can be formulated and implemented.
Acknowledgments
Site Investigators of the Canadian Neonatal Transport Network: Avash Singh, Joseph Ting, and Michael Castaldo, British Columbia Children’s & Women’s Hospital, Vancouver, British Columbia; Anne Tierney and Sumesh Thomas, Foothills Medical Centre and Alberta Children’s Hospital, Calgary, Alberta; Ernesto Phillips, Paul Byrne, and Jennifer Toye, Royal Alexandra Hospital and Stollery Children’s Hospital, Edmonton, Alberta; William Bingham and Sibasis Daspal, Royal University Hospital, Saskatoon Saskatchewan; Zarin Kalapesi, Regina General Hospital, Regina Saskatchewan; Rebecca Caces & Michael Narvey, Winnipeg Health Sciences Centre, Winnipeg Manitoba; Henry Roukema, London Health Sciences Centre, London, Ontario; Michael Marrin, McMaster Children’s Hospital, Hamilton, Ontario; Stephanie Redpath, Children’s Hospital of Eastern Ontario, Ottawa, Ontario; Hilary Whyte, Hospital for Sick Children, Toronto, Ontario; Louis Beaumier and Thérèse Perrault, Montreal Children’s Hospital, Montreal Quebec; Geneviève Piuze, Centre Hospitalier Universitaire de Québec, Laval, Quebec; Edith Massé, Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, Quebec; Krista Jangaard and Balpreet Singh, IWK Health Centre, Halifax, Nova Scotia; Akhil Desphpandey, Janeway Children’s Health & Rehabilitation Center, St. John’s, Newfoundland.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Edge WE, Kanter RK, Weigle CG, et al. Reduction of morbidity in interhospital transport by specialized staff. Crit Care Med 1994;22:1186-91. [Crossref] [PubMed]
- Orr RA, Felmet KA, Han Y, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics 2009;124:40-8. [Crossref] [PubMed]
- Karlsen KA, Trautman M, Price-Douglas W, et al. National survey of neonatal transport teams in the United States. Pediatrics 2011;128:685-91. [Crossref] [PubMed]
- Leslie A, Stephenson T. Neonatal transfers by advanced neonatal nurse practitioners and paediatric registrars. Arch Dis Child Fetal Neonatal Ed 2003;88:F509-12. [Crossref] [PubMed]
- King BR, King TM, Foster RL, et al. Pediatric and neonatal transport teams with and without a physician: a comparison of outcomes and interventions. Pediatr Emerg Care 2007;23:77-82. [Crossref] [PubMed]
- Lee SK, Zupancic JA, Sale J, et al. Cost-effectiveness and choice of infant transport systems. Med Care 2002;40:705-16. [Crossref] [PubMed]
- Stroud MH, Trautman MS, Meyer K, et al. Pediatric and neonatal interfacility transport: results from a national consensus conference. Pediatrics 2013;132:359-66. [Crossref] [PubMed]
- Whyte HE, Jefferies AL. Canadian Paediatric Society, Fetus and Newborn Committee. The interfacility transport of critically ill newborns. Paediatr Child Health 2015;20:265-75. [Crossref] [PubMed]
- Fenton AC, Leslie A. The state of neonatal transport services in the UK. Arch Dis Child Fetal Neonatal Ed 2012;97:F477-81. [Crossref] [PubMed]
- Bigham MT, Schwartz HP. Ohio Neonatal/Pediatric Transport Quality Collaborative. Quality metrics in neonatal and pediatric critical care transport: a consensus statement. Pediatr Crit Care Med 2013;14:518-24. [Crossref] [PubMed]
- Ramnarayan P. Measuring the performance of an inter-hospital transport service. Arch Dis Child 2009;94:414-6. [Crossref] [PubMed]
- Available online: http://gamutqi.org/GAMUT%20Metrics_version%205.16.2016.pdf
- Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995;311:376-80. [Crossref] [PubMed]
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st Century. Washington, D.C: National Academy Press, 2001.
- Available online: >https://ukntg.net/annual-reports/
- Zeitlin J, Manktelow BN, Piedvache A, et al. Use of evidence based practices to improve survival without severe morbidity for very preterm infants: results from the EPICE population based cohort. BMJ 2016;354:i2976. [Crossref] [PubMed]
- Society of Obstetricians and Gynaecologists of Canada. Maternal transfer policy. Obstet Gynaecol Can 2005;27:956-8. [Crossref]
- Chien LY, Whyte R, Aziz K, et al. Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol 2001;98:247-52. [PubMed]
- Shah PS, Sankaran K, Aziz K, et al. Outcomes of preterm infants <29 weeks gestation over 10-year period in Canada: a cause for concern? J Perinatol 2012;32:132-8. [Crossref] [PubMed]
- Lui K, Abdel-Latif ME, Allgood CL, et al. Improved outcomes of extremely premature outborn infants: effects of strategic changes in perinatal and retrieval services. Pediatrics 2006;118:2076-83. [Crossref] [PubMed]
- Binder S, Hill K, Meinzen-Derr J, et al. Increasing VLBW deliveries at subspecialty perinatal centers via perinatal outreach. Pediatrics 2011;127:487-93. [Crossref] [PubMed]
- Crowther CA, Hiller JE, Doyle LW, et al. Effect of magnesium sulfate given for neuroprotection before preterm birth: a randomized controlled trial. JAMA 2003;290:2669-76. [Crossref] [PubMed]
- Tarnow-Mordi W, Morris J, Kirby A, et al. Delayed versus immediate cord clamping in preterm infants. N Engl J Med 2017;377:2445-55. [Crossref] [PubMed]
- Abdel-Latif ME, Berry A. Dissection of the retrieval times of a centralised transport service, New South Wales, Australia. Arch Dis Child 2009;94:282-6. [Crossref] [PubMed]
- Bagley Thompson C, Schaffer J. Minimum data set development: air transport time-related terms. Int J Med Inform 2002;65:121-33. [Crossref] [PubMed]
- Lupton BA, Pendray MR. Regionalized neonatal emergency transport. Semin Neonatol 2004;9:125-33. [Crossref] [PubMed]
- Holt J, Fagerli I. Air transport of the sick newborn infant: audit from a sparsely populated county in Norway. Acta Paediatr 1999;88:66-71. [Crossref] [PubMed]
- Moss SJ, Embleton ND, Fenton AC. Towards safer neonatal transfer: the importance of critical incident review. Arch Dis Child 2005;90:729-32. [Crossref] [PubMed]
- Hon KL, Olsen H, Totapally B, et al. Air versus ground transportation of artificially ventilated neonates: comparative differences in selected cardiopulmonary parameters. Pediatr Emerg Care 2006;22:107-12. [Crossref] [PubMed]
- Kempley ST, Baki Y, Hayter G, et al. Effect of a centralised transfer service on characteristics of inter-hospital neonatal transfers. Arch Dis Child Fetal Neonatal Ed 2007;92:F185-8. [Crossref] [PubMed]
- Whitfield JM, Buser MK. Transport stabilization times for neonatal and pediatric patients prior to interfacility transfer. Pediatr Emerg Care 1993;9:69-71. [Crossref] [PubMed]
- Boden WE, Eagle K, Granger CB. Reperfusion strategies in acute ST-segment elevation myocardial infarction: a comprehensive review of contemporary management options. J Am Coll Cardiol 2007;50:917-29. [Crossref] [PubMed]
- McPherson ML, Graf JM. Speed isn't everything in pediatric medical transport. Pediatrics 2009;124:381-3. [Crossref] [PubMed]
- Mori R, Fujimura M, Shiraishi J, et al. Duration of inter-facility neonatal transport and neonatal mortality: Systematic review and cohort study. Pediatr Int 2007;49:452-8. [Crossref] [PubMed]
- Kiefe CI, Weissman NW, Allison JJ, et al. Identifying achievable benchmarks of care: Concepts and methodology. Int J Qual Health Care 1998;10:443-7. [Crossref] [PubMed]
- Ho S, Saigal S. Survival and early outcomes of infants of borderline viability. Neoreviews 2005;6:e123-32. [Crossref]
- Papile LA, Baley JE, Benitz W, et al. Hypothermia and neonatal encephalopathy. Pediatrics 2014;133:1146-50. [Crossref] [PubMed]
- Nosherwan A, Cheung PY, Schmölzer GM. Management of extremely low birth weight infants in delivery room. Clin Perinatol 2017;44:361-75. [Crossref] [PubMed]
- Lee SK, Zupancic JA, Pendray M, et al. Transport risk index of physiologic stability: a practical system for assessing infant transport care. J Pediatr 2001;139:220-6. [Crossref] [PubMed]
- Gould JB, Danielsen BH, Bollman L, et al. Estimating the quality of neonatal transport in California. J Perinatol 2013;33:964-70. [Crossref] [PubMed]
- Singh JM, MacDonald RD, Bronskill SE, et al. Incidence and predictors of critical events during urgent air–medical transport. CMAJ 2009;181:579-84. [Crossref] [PubMed]
- Broughton SJ, Berry A, Jacobe S, et al. The mortality index for neonatal transportation score: a new mortality prediction model for retrieved neonates. Pediatrics 2004;114:e424-8. [Crossref] [PubMed]
- Orr RA, Venkataraman ST, Mccloskey KA, et al. Measurement of pediatric illness severity using simple pretransport variables. Prehosp Emerg Care 2001;5:127-33. [Crossref] [PubMed]
- Markakis C, Dalezios M, Chatzicostas C, et al. Evaluation of a risk score for interhospital transport of critically ill patients. Emerg Med J 2006;23:313-7. [Crossref] [PubMed]
- Available online: https://www.picanet.org.uk/
- Redpath S, Deboer J. Big advancements in safely delivering tiny packages: Ottawa paramedic service and the Children’s Hospital of Eastern Ontario partner in the creation of a specialized neonatal transport unit. Canadian Paramedicine 2018. Available online: https://canadianparamedicine.ca/online-edition/august-september-2018-full-edition/