
Trends in centralization of very preterm deliveries and neonatal survival in Finland in 1987–2017
Introduction
Centralization of perinatal care of very preterm infants entails transferring mothers who are expected to deliver before 32 gestational weeks to maternity hospitals with sufficiently equipped and staffed neonatal units for the care of their preterm infants; these hospitals are referred to as level 3 hospitals (1) in this review. Centralization has been recommended worldwide for decades (2).
Evidence supporting centralization
Several large multicenter studies have shown strikingly similar results regarding increased mortality in infants born in level 2 hospitals compared to level 3 hospitals (3-8). In a cohort from the Cincinnati region (848 very low birth weight infants, 19 hospitals), Warner et al. showed an odds ratio of 2.64 for death or major morbidity among infants born in lower-level hospitals. In Sweden, Johansson et al. (2,285 very preterm infants, nationwide study) showed two-fold odds of death for infants born before 28 gestational weeks, and an odds ratio of 1.33 for infants born before 32 gestational weeks. Chien et al. (3,769 very preterm infants, 17 hospitals) showed that the odds ratio of death was 1.7 for very preterm infants born in lower-level hospitals in Canada. Similarly, Cifuentes and colleagues (16,732 infants with birth weight <2,000 grams, statewide study) showed over two-fold odds of death among very low birth weight infants (birth weight <1,500 grams) in California. In 2007 Phibbs et al. (48,237 very low birth weight infants, statewide study) showed that very low birth weight infants had a higher risk of mortality if they were born in lower-level hospitals (odds ratio 1.22 to 2.72), but also if they were born in level 3 hospitals with <100 annual very low birth weight admissions (odds ratio 1.19 to 1.78). A systematic review identified 37 studies on very low birth weight infants and 4 studies on very preterm infants. They summarized findings regarding mortality and concluded an odds ratio of 1.62 in very low birth weight infants and 1.55 in very preterm infants born in level 2 hospitals compared to level 3 hospitals. Several studies have also indicated that increased survival does not necessarily increase the risk for short-term (9,10) or long-term morbidities (11).
The PERFECT (Performance, Effectiveness and Cost of Care Episodes) Preterm Infant Study studied the effects of delivery hospitals level on mortality and long-term morbidities up to 5 years of age. The PERFECT Preterm Infant Study was initiated in Finland in 2004 as a large consortium including the National Institute of Health and Welfare and all five university hospital districts (12). It showed that mortality was two-fold among very preterm infants born in level 2 hospitals, compared to infants born in level 3 hospitals in Finland in 2000 through 2003 (13). Importantly, the increased survival was not associated with an increased risk of long-term morbidities (14-16). Further analyses revealed that the increase in mortality among very preterm infants born in level 2 hospitals was explained by a higher risk of death among those born outside of office hours (nights, weekends and holidays) (12). This is very relevant, because 60% of very preterm deliveries took place outside of office hours.
Centralization in Finland in 1987–2017
Finland is a sparsely populated country with approximately 5.5 million inhabitants and 50,000–60,000 annual deliveries. Currently, there are five university hospitals in Finland, which all serve as regional level 3 perinatal centers, 17 level 2 maternity hospitals, and one level 1 maternity hospital. The distances between level 3 hospitals and lower-level maternity hospitals range from 15 kilometers to >300 kilometers. The rates of prematurity (birth before 37 gestational weeks, 5.9% in 2017), perinatal mortality (including stillborn infants, 3.9/1,000 newborns in 2017) and infant mortality (1.9/1,000 live births in 2017) are among the lowest in the world (17).
The National Institute for Health and Welfare governed by the Ministry of Social Affairs and Health monitors, studies and develops the health of the population in Finland. The Medical Birth Register, since 1987, is one of the national registers run by the National Institute for Health and Welfare. It covers all pregnancies, fetal deaths, births and early neonatal deaths. It is linked to several other registers including the Cause of Death Register to complete missing cases and extend the data on mortality up to 1 year. The Very Preterm Infant Register has collected data on treatments and neonatal outcomes of infants born below 32 gestational weeks or with a birth weight ≤1,500 grams as a part of the Medical Birth Register since 2005.
Data from the Medical Birth Register shows that the proportion of live-born very preterm infants delivered in level 3 hospitals increased from 63% in 1987 to 95% in 2017 (Figure 1). The proportion of very preterm infants born in level 3 hospitals in the late 1980s largely reflected the proportion of population living in the areas of these level 3 hospitals. A clear trend towards centralization can be seen from year 1999 onwards.
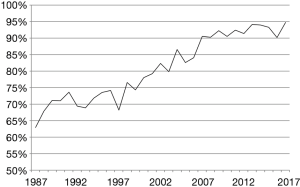
The latest increase in centralization can be seen between years 2006 (84%) and 2007 (90%). This was related to the PERFECT study results that supported centralization and were implemented by clinicians nationwide. The centralization was further enforced in 2010 by the Finnish Ministry of Social Affairs and Health, which stated that all deliveries below 32 gestational weeks or with an expected birth weight below 1,500 g should be centralized to level 3 hospitals (18).
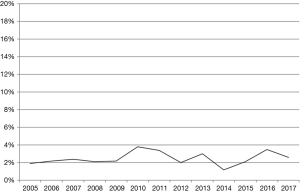
Increased centralization of very preterm deliveries should decrease the need for postnatal transfers of sick preterm infants. The information of early postnatal transfers (within 48 hours after birth) has been available in the Very Preterm Infant Register since 2005. The data shows that early postnatal transfers of very preterm infants in Finland have remained rare (2% to 4% of all very preterm infants) throughout the 12-year time period (Figure 2).
Survival of very preterm infants in Finland in 1987–2017
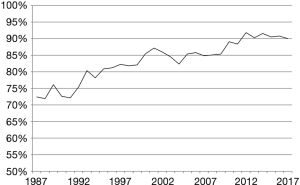
The data from the Medical Birth Register shows that the survival of live-born very preterm infants increased from 72% in 1987 to 90% in 2017 (Figure 3). There are many potential reasons for the improved survival. The first increase in survival occurred between 1991 and 1993, which is likely to reflect the emergence of commercial availability of surfactant. There was another turning point in survival in 2009 when the survival started to increase from 85% and reached 92% in 2012. This coincides with the latest improvement in centralization.
Discussion
The centralization of very preterm deliveries has succeeded remarkably well in Finland. The centralization was followed by an improvement in survival.
There are several examples of similar centralization initiatives in other countries that have failed. Germany has traditionally had a large number of small neonatal hospitals. In 2010, supported by a study by Bartels et al. (19) which showed improved outcomes in level 3 hospitals with >36 annual admissions of very preterm infants, the Federal Joint Committee (Gemeinsamer Bundesausschuss) in Germany dictated new volume requirements for level 3 hospitals (20). After this initiative, however, several German neonatal hospitals filed litigations challenging this decision, and won (21). As a result, there are currently over 160 neonatal hospitals designated to the highest level of care in Germany, one quarter of which care for less than 36 very preterm infants annually (22). In the UK, a nationwide reorganization into managed clinical networks was undertaken in 2003, with the aim to increase maternal transfers to level 3 hospitals in high-risk pregnancies, and thus decrease early postnatal transfers of infants. Even if the centralization rate rose from 18% to 49% among deliveries at 27 to 28 gestational weeks, the rate of early postnatal transfers also rose from 7% to 12% (23). Obstacles such as staffing shortages, overcrowded level 3 hospitals and lack of coordination between obstetric and neonatal services have been suggested as underlying causes of increased postnatal transfers of very preterm infants in the UK (24-26). In California, the overall centralization rate was 51% in 1993, but decreased to 44% by the year 2000 (27). The de-centralization was more pronounced in areas where new level 2 hospitals were opened (57% in 1993 to 38% in 2000).
The success of centralization in Finland seems to be exceptional. A governmentally funded health care system seems to be able to facilitate this type of organizational changes, as financial interests are not contradicting centralization. It is also likely that the implementation of centralization succeeds better when clinicians are involved in generating the scientific evidence and in the implementation process.
Low mortality rates have been achieved in the era of centralized perinatal care in Finland (28-30). In New South Wales, Australia, a telephone service providing perinatal guidance to obstetricians and coordinating maternal transfers was implemented, and a subsequent increase in centralization from 80% to 85% was seen among deliveries at <28 gestational weeks, accompanied by a decrease in overall neonatal mortality (31). A similar centralization strategy was implemented in the greater Cincinnati region in the early 2000s, where the centralization rate increased from 75% to 89% following a perinatal outreach program (32).
Centralization of very preterm deliveries has the potential to decrease the costs of care. The decrease can be induced in part by decreasing the amount of postnatal transfers. Aside from the direct cost of the postnatal transfer (33), early postnatal transfer can increase costs indirectly via morbidities such as intraventricular hemorrhage, which is associated with neurodevelopmental impairment (34-37). As shown by Korvenranta et al., health care costs of very preterm infants are twice as high during the initial hospitalization if the infant has two or more long-term morbidities (38). The costs during the fifth year of life are three times higher for very preterm infants with morbidities compared to infants without morbidities, and even six times higher for very preterm infants with cerebral palsy (39). Nonetheless, the potential costs associated with in utero transfers and centralizing mothers to level 3 hospitals also need to be accounted for. However, we have previously shown that in Finland, these costs are relatively low; centralized mothers spend a mean of 4 days in level 3 hospitals prior to delivery, which approximates to a need for two antenatal beds per 10,000 deliveries (40). The need for antenatal beds in the whole population, i.e., including mothers that already lived within the level 3 hospital areas, was approximately 5 per 10,000 deliveries.
Future challenges include sustaining the positive changes. This requires policy-makers to be aware of any arising financial interests, tackle any personnel shortages and keep the whole referral chain informed of the positive effects of centralization. Continuous benchmarking and quality improvement incentives are good ways to keep all clinicians convinced to keep referring very preterm deliveries to level 3 hospitals. International collaboration and high quality national registers are imperative to achieve this.
Conclusions
The experience in Finland shows that centralization of care can be achieved if the initiative is clinician-driven and if the staffing and infrastructure are adequate. The price of centralization is low when measured as antenatal bed occupancy in level 3 hospitals, and the gain might be increased survival for very preterm infants. A new Finnish study comparing mortality and other outcomes before and after this paradigm change is called for.
Acknowledgments
The authors thank Anna Heino at the National Institute for Health and Welfare for technical and administrative support.
Funding: This work was supported by personal research grants awarded to Dr. Helenius by State Research Funding, Hospital District of Southwest Finland (grant number 13243).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- American Academy of Pediatrics Committee on Fetus And Newborn. Levels of neonatal care. Pediatrics 2012;130:587-97. [Crossref] [PubMed]
- Ryan GM Jr. Toward improving the outcome of pregnancy: recommendations for the regional development of perinatal health services. Obstet Gynecol 1975;46:375-84. [PubMed]
- Chien LY, Whyte R, Aziz K, et al. Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol 2001;98:247-52. [PubMed]
- Cifuentes J, Bronstein J, Phibbs CS, et al. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics 2002;109:745-51. [Crossref] [PubMed]
- Johansson S, Montgomery SM, Ekbom A, et al. Preterm delivery, level of care, and infant death in Sweden: A population-based study. Pediatrics 2004;113:1230-5. [Crossref] [PubMed]
- Warner B, Musial MJ, Chenier T, et al. The effect of birth hospital type on the outcome of very low birth weight infants. Pediatrics 2004;113:35-41. [Crossref] [PubMed]
- Phibbs CS, Baker LC, Caughey AB, et al. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med 2007;356:2165-75. [Crossref] [PubMed]
- Lasswell SM, Barfield WD, Rochat RW, et al. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA 2010;304:992-1000. [Crossref] [PubMed]
- Costeloe KL, Hennessy EM, Haider S, et al. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ 2012;345:e7976. [Crossref] [PubMed]
- Marlow N, Bennett C, Draper ES, et al. Perinatal outcomes for extremely preterm babies in relation to place of birth in England: the EPICure 2 study. Arch Dis Child Fetal Neonatal Ed 2014;99:F181-8. [Crossref] [PubMed]
- Younge N, Goldstein RF, Bann CM, et al. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med 2017;376:617-28. [Crossref] [PubMed]
- Lehtonen L, Rautava L, Korvenranta E, et al. PERFECT preterm infant study. Ann Med 2011;43 Suppl 1:S47-53. [Crossref] [PubMed]
- Rautava L, Lehtonen L, Peltola M, et al. The effect of birth in secondary- or tertiary-level hospitals in Finland on mortality in very preterm infants: A birth-register study. Pediatrics 2007;119:e257-63. [Crossref] [PubMed]
- Rautava L, Häkkinen U, Korvenranta E, et al. Health-related quality of life in 5-year-old very low birth weight infants. J Pediatr 2009;155:338-43.e1-3.
- Rautava L, Häkkinen U, Korvenranta E, et al. Health and the use of health care services in 5-year-old very-low-birth-weight infants. Acta Paediatr 2010;99:1073-9. [Crossref] [PubMed]
- Rautava L, Andersson S, Gissler M, et al. Development and behaviour of 5-year-old very low birthweight infants. Eur Child Adolesc Psychiatry 2010;19:669-77. [Crossref] [PubMed]
- THL. Perinataalitilasto-synnyttäjät, synnytykset ja vastasyntyneet 2017. Cited 2019 Apr 9. Available online: http://www.stat.fi/til/synt/2017/synt_2017_2018-04-27_tie_001_fi.html
- Ministry for Social Affairs and Health. Sosiaali-ja terveysministeriö yhtenäiset päivystyshoidon perusteet työryhmän raportti. Cited 2019 Apr 23. Available online: http://urn.fi/URN:ISBN:978-952-00-2963-0
- Bartels DB, Wypij D, Wenzlaff P, et al. Hospital volume and neonatal mortality among very low birth weight infants. Pediatrics 2006;117:2206-14. [Crossref] [PubMed]
- Ehrich J, Grote U, Gerber-Grote A, et al. The child health care system of Germany. J Pediatr 2016;177S:S71-86. [Crossref] [PubMed]
- Poets CF. Perinatal regionalisation in the UK: an international perspective. Arch Dis Child Fetal Neonatal Ed 2014;99:F176. [Crossref] [PubMed]
- Perinatalzentren. Cited 2019 May 21. Available online: https://perinatalzentren.org/krankenhaussuche.php
- Gale C, Santhakumaran S, Nagarajan S, et al. Impact of managed clinical networks on NHS specialist neonatal services in England: population based study. BMJ 2012;344:e2105. [Crossref] [PubMed]
- Bliss baby report 2015 - England. Cited 2019 May 24. Available online: http://www.bliss.org.uk/babyreport
- Kempley ST, Baki Y, Hayter G, et al. Effect of a centralised transfer service on characteristics of inter-hospital neonatal transfers. Arch Dis Child Fetal Neonatal Ed 2007;92:F185-8. [Crossref] [PubMed]
- Gale C, Hay A, Philipp C, et al. In-utero transfer is too difficult: results from a prospective study. Early Hum Dev 2012;88:147-50. [Crossref] [PubMed]
- Haberland CA, Phibbs CS, Baker LC. Effect of opening midlevel neonatal intensive care units on the location of low birth weight births in California. Pediatrics 2006;118:e1667-79. [Crossref] [PubMed]
- Smith LK, Morisaki N, Morken NH, et al. An international comparison of death classification at 22 to 25 weeks’ gestational age. Pediatrics 2018;142:e20173324. [Crossref] [PubMed]
- Helenius K, Sjörs G, Shah PS, et al. Survival in very preterm infants: An international comparison of 10 national neonatal networks. Pediatrics 2017;140:e20171264. [Crossref] [PubMed]
- Zeitlin J, Mortensen L, Cuttini M, et al. Declines in stillbirth and neonatal mortality rates in Europe between 2004 and 2010: results from the Euro-Peristat project. J Epidemiol Community Health 2016;70:609-15. [Crossref] [PubMed]
- Lui K, Abdel-Latif ME, Allgood CL, et al. Improved outcomes of extremely premature outborn infants: effects of strategic changes in perinatal and retrieval services. Pediatrics 2006;118:2076-83. [Crossref] [PubMed]
- Binder S, Hill K, Meinzen-Derr J, et al. Increasing VLBW deliveries at subspecialty perinatal centers via perinatal outreach. Pediatrics 2011;127:487-93. [Crossref] [PubMed]
- Mistry H, Dowie R, Franklin RC, et al. Costs of neonatal care for low-birthweight babies in English hospitals. Acta Paediatr 2009;98:1123-9. [Crossref] [PubMed]
- Shlossman PA, Manley JS, Sciscione AC, et al. An analysis of neonatal morbidity and mortality in maternal (in utero) and neonatal transports at 24-34 weeks’ gestation. Am J Perinatol 1997;14:449-56. [Crossref] [PubMed]
- Hohlagschwandtner M, Husslein P, Klebermass K, et al. Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet 2001;265:113-8. [Crossref] [PubMed]
- Mohamed MA, Aly H. Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed 2010;95:F403-7. [Crossref] [PubMed]
- Mukerji A, Shah V, Shah PS, et al. Periventricular/intraventricular hemorrhage and neurodevelopmental outcomes: A meta-analysis. Pediatrics 2015;136:1132-43. [Crossref] [PubMed]
- Korvenranta E, Linna M, Rautava L, et al. Hospital costs and quality of life during 4 years after very preterm birth. Arch Pediatr Adolesc Med 2010;164:657-63. [Crossref] [PubMed]
- Korvenranta E, Lehtonen L, Rautava L, et al. Impact of very preterm birth on health care costs at five years of age. Pediatrics 2010;125:e1109-14. [Crossref] [PubMed]
- Helenius K, Helle E, Lehtonen L. Amount of antenatal care days in a context of effective regionalization of very preterm deliveries. J Pediatr 2016;169:81-6. [Crossref] [PubMed]


