An overarching approach for acute care delivery: extension of the acute care model to the entire inpatient admission
Introduction
The initial care models were developed for chronic diseases as they have a dramatic impact on health care outcomes and costs (1). To address this healthcare crisis, strategies were introduced to improve care (2). Today, much of what currently exists for chronic care management is based on the chronic care model developed by the MacColl Institute for Healthcare Innovation at the Group Health Cooperative. Key components include mobilizing community resources, an emphasis on evidence based care, enabling patient self-management, and focusing on high quality care (3-5). Assessing the impact of applying this model, there is abundant evidence of a positive impact on patient outcomes and healthcare costs. A recent literature review by Davy et al. found that of the 77 papers which met inclusion criteria, all but two reported improvements to healthcare practice or health outcomes for patients with chronic disease (2).
While optimization of the care of patients with chronic medical conditions was improving care and decreasing costs, acute care providers were recognizing the limitations of their current care models. Using the emergency department (ED) as a case example, the 2006 Institute of Medicine (IOM) report, “The Future of Emergency Care”, described emergency medical systems at the time as highly fragmented with numerous obstacles in place for providing high quality health care. That same report provided recommendations for optimizing acute care evidence-based care and collecting data to advance clinical knowledge and to optimize system performance (6-8).
In response to these findings and call to action, Iyer et al. (9) proposed the acute care model as a framework for quality improvement work in emergency care. The acute care model is a strategy for creating a common language and improving the key components of acute care. Through the use of the acute care model, ED can not only improve flow, but also improve care delivery.
Meanwhile, the other relevant parts of the acute care system, i.e., inpatient admission to ward and intensive care unit (ICU) contexts, have continued to operate within silos. While there are many published examples of care optimization within a particular context, the overall care of patients remains fragmented as they transition between various acute care contexts. Are the same standards with regards to resource utilization, consideration of cost, evidence based care being applied uniformly in all contexts? Does the absence of clear risk stratification models and thresholds for escalation of care hamper efficiency in patient flow? To answer these questions, we are unaware of any current model for acute care delivery that has been applied to the entire acute illness episode inclusive of the inpatient care setting.
The absence of an overarching model for the care of patients throughout the acute care system represents a gap in our quest for continual improvement in care delivery to optimize patient outcomes while improving flow and reducing waste. We propose that a unified approach to improve quality of care for acute illness may be achieved by extending the acute care model to the inpatient care setting.
Acute care model
The acute care model has been previously described by Iyer et al. (9) and applied to the ED context. There are four key components: segmentation, therapeutic reliability, diagnostic accuracy, and disposition (Figure 1). Segmentation occurs at the onset of patient care and is repeated through the ongoing care of the patient as new results/outcomes arise. The next two components represent potential pathways for care delivery depending on the diagnostic certainty following segmentation.
In patients where there is minimal diagnostic uncertainty and the patient is appropriate for a standardized therapeutic approach, i.e., an asthma exacerbation in a patient with known asthma, the therapeutic reliability pathway can be applied. The goal of this pathway is to provide safe, effective, and timely care to prevent clinical deterioration. The process starts by placing the patient within an appropriate risk category for severity of illness, potentially taking advantage of a validated scoring system. The risk category subsequently dictates the therapeutic approach, applying evidence based clinical treatment pathways. Finally, response to treatment is assessed in an iterative fashion until disposition to another context is warranted (home, inpatient ward, ICU).
Alternatively, when a patient presents with an undifferentiated illness, the diagnostic accuracy pathway represents a more custom approach to safely, effectively, and efficiently arrive at the correct diagnosis. The process is similar to the therapeutic reliability pathway. Based upon an initial differential diagnosis, the patient is segmented into risk categories for the diagnoses again potentially utilizing a validated scoring system. Testing is then tailored to the risk category utilizing available evidence (prevalence data, available likelihood ratios, etc.) allowing for the implementation of clinical diagnostic pathways. Results are then iteratively interpreted to allow for arrival at a diagnosis or adjustment of the differential until a disposition decision is made.
The final step of the model consists of decisions around disposition, and represents the key metric for efficient and timely care. Providers must assess the outcomes of the pathway they undertook, whether that is clinical changes following the therapeutic reliability pathway or clarity of diagnosis following the diagnostic accuracy pathway. Interpretation of those outcomes allows the provider to reassess patient status and risk of clinical deterioration, allowing for a decision regarding the most appropriate context for the patient’s disposition, i.e., discharge to home, remain in the ED for continued care, transfer to the general inpatient ward, or transfer to the ICU. Again, validated risk assessment systems and clinical treatment pathways can aide with disposition decisions.
Extension to the inpatient admission
We submit that adapting the acute care model to include the inpatient care setting can provide an overarching model applicable to the entire continuum of an acute illness episode. Slight adaption of the final step of the model, disposition, is required for viewing this step as a branch point for re-entering the model back at segmentation if a patient’s care is going to continue into the inpatient context (Figure 2). Similarly, the same approach can be utilized when a patient requires escalation of care from a ward unit to an ICU unit, as well as with de-escalation of care from the ICU to the ward.
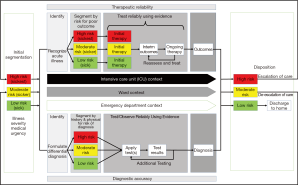
A common theme in the current acute care model is the importance of patient stratification. This is predominantly based upon patient severity or likelihood of a diagnosis, and ideally performed through the use of validated scoring systems. That same approach can be extended to the disposition phase of the acute care model. Currently, patient disposition decisions are made by individual providers’ decisions regarding continued care needs and risk for decompensation. Through application of validated scoring systems, health care systems can work towards enhancing patient flow by optimizing timely transitions of care. In addition, standardized clinical criteria for disposition could also help limit the occurrence of unsafe transfers by ensuring patients are admitted to the appropriate care context based upon their risk of decompensation.
Key to the effectiveness of this approach is the continuation of the same standards of care and agreed upon processes to ensure safe, effective, and timely care. This can be attained through the development of institutional care pathways or algorithms that apply to patients as they traverse the acute care system, as opposed to the traditional, isolated guidelines meant to be applied only in a specific care setting.
While the separation of the acute care model into separate pathways for diagnostic accuracy and therapeutic reliability is helpful for conceptually structuring the care delivery approach, in the practice of pediatric medicine it is rarely feasible for these two pathways to occur in isolation once a patient is admitted. It is rare that a patient presents to the acute care setting and require admission purely for the purpose of establishing a diagnosis. The field of medicine has focused of transitioning much of the diagnostic work-up for stable patients to the outpatient setting, limiting inpatient admission for those who require an escalated level of care. Subsequently, concurrent management of patient’s symptoms and pathophysiology (therapeutic reliability) is required while a definitive diagnosis is being reached (diagnostic accuracy). The true test of the application of the acute care model to the inpatient context is allowing the concurrent pursuit of a diagnosis throughout an inpatient admission (diagnostic accuracy) spanning care contexts while providing safe and effective care (therapeutic reliability) in the appropriate context based upon patient severity status and risk of decompensation.
A case example of application of the acute care model to the entire acute care context
Following the path of a patient presenting with respiratory distress can illustrate the applicability of the acute care model to not only the ED but the inpatient context as well. Additionally, the process will highlight how this structured approach allows for critical assessment of the care delivery system and can lead to areas of standardization of care and optimization of flow.
Figure 3A demonstrates the use of the acute care model for our case example starting with the ED context. In this example, the patient presents to the ED and is brought to triage for initial segmentation and identification. Both the therapeutic reliability and diagnostic accuracy pathways are activated through a screening history and physical. The clinical findings of this patient, poor aeration, hypoxia, severe work of breathing, and altered mental status, segment the patient to high risk. This high risk designation activates additional care providers to allow for efficient care delivery and mobilization of resources. Concurrently, a brief history identifies this presentation as likely a severe asthma exacerbation but the differential diagnosis also includes foreign body aspiration, pneumonia, and myocarditis given the severity of presentation. Validated screening tools can be applied at this point to increase the efficiency of this initial segmentation. As demonstrated in Figure 3A, both pathways continue forward in the ED context, assessing response to initial therapies while applying tests to narrow or adapt the differential diagnosis. A clinical care algorithm that pairs treatment strategies with severity of presentation can allow for standardization of therapies and a thoughtful approach to testing focusing on providing quality care.
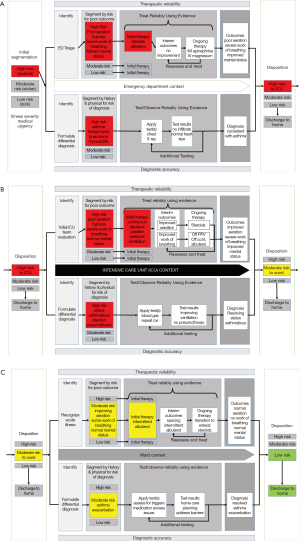
For this example patient, initial testing is consistent with asthma as the clinical condition, and initial therapies have led to improvement in mental status with ongoing severe respiratory distress. Given these outcomes, the most appropriate disposition for this patient is the ICU. This determination can again be based on a risk stratification tool to allow efficient determinations regarding disposition and timely activation of resources.
Figure 3B continues the acute care model to the ICU context where the ICU team evaluates the patient and continues down both the therapeutic reliability pathway through escalation of asthma specific therapies. In this context, the diagnostic accuracy pathway also applies, having a high suspicion of new complications if therapies do not lead to the appropriate result, i.e., development of a pneumothorax or new clinically apparent infectious etiology. The ICU team will cycle through iterations of the acute care model until the patient has improved enough for transition to the general inpatient ward.
Figure 3C completes our multi-context scenario extending the care of the patient to the ward. Again, the team will assess the patient and continue to tailor therapies based on the patient’s symptoms, working towards discharge to home. Meanwhile the diagnostic accuracy pathway focus has transitioned to exploring the etiology of the patient’s asthma exacerbation and home care planning to minimize the likelihood of future admissions. This case example demonstrates the utility of an overarching model for characterizing the entire continuum of care for an acute illness episode.
Call for application of the acute care model to care delivery systems
The medical system continues to grow in its complexity in parallel with the increasing complexity of patient care needs. A thoughtful and direct approach is required to bring stability to the system and thus allow for optimization of care delivery and patient outcomes. The example above demonstrates that application of the acute care model to the entire inpatient context is not only theoretically beneficial but practically possible.
The acute care model provides a framework for standardization of care to meet high quality standards. Through iterative tracking of performance and measurement of outcomes, institutions can work to reduce waste and high costs that are ultimately passed onto patients (10). Additionally, standardization can allow for enhanced efficiency of care—vital to a medical system that is already overtaxed to meet the needs of patients. We challenge institutions to take a global approach at the care they provide and breakdown the silos separating different care contexts, utilizing the acute care model as a roadmap for that important work.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Alwan A, Maclean DR, Riley LM, et al. Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries. Lancet 2010;376:1861-8. [Crossref] [PubMed]
- Davy C, Bleasel J, Liu H, et al. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res 2015;15:194. [Crossref] [PubMed]
- Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag 2003;6:63-71. [Crossref] [PubMed]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA 2002;288:1909-14. [Crossref] [PubMed]
- Rea H, Kenealy T, Wellingham J, et al. Chronic Care Management evolves towards Integrated Care in Counties Manukau, New Zealand. N Z Med J 2007;120:U2489. [PubMed]
- Institute of Medicine Committee on the Future of Emergency Care in the US Health Care System. Hospital-based emergency care: at the breaking point. National Academies Press, 2006.
- Institute of Medicine Committee on the Future of Emergency Care in the US Health Care System. Emergency medical services: at the crossroads. National Academies Press, 2006.
- Institute of Medicine Committee on the Future of Emergency Care in the US Health Care System. Emergency care for children: growing pains. National Academies Press, 2006.
- Iyer S, Reeves S, Varadarajan K, et al. The Acute Care Model: A New Framework for Quality Care in Emergency Medicine. Clin Pediatr Emerg Med 2011;12:91-101. [Crossref]
- Margolis P, Provost LP, Schoettker PJ, et al. Quality improvement, clinical research, and quality improvement research--opportunities for integration. Pediatr Clin North Am 2009;56:831-41. [Crossref] [PubMed]