Always ready, always prepared—preparing for the next pandemic
Introduction
The need to plan and prepare for potentially overwhelming infectious outbreaks, such as the next influenza pandemic or an Ebola epidemic, has added a whole new set of challenges to the practice of pediatric critical care medicine. Medicine has changed immensely over the past 100 years since the influenza pandemic of 1918–1919. One of the most significant changes has been the development of critical care medicine allowing the care and survival of seriously ill patients that would have been impossible in the past. Current technology and plentiful resources in most developed countries has meant that care for individuals and groups of patients has not had to be rationed even though critical care resources are often the limiting factor during winter peak census periods with time limited natural or man-made disasters (1,2). However, the emergence of the next great pandemic will severely affect our ability to care for massive numbers of patients with the traditional approaches with which we have become accustomed.
Children often are an overrepresented population during both natural and man-made disasters due to both physiological differences and innate social vulnerabilities. During influenza pandemics children are often disproportionately represented in the intensive care unit population, tend to require mechanical ventilation more often than adults, and despite this have been shown to have better survival (3,4). Unfortunately many governmental and hospital system disaster management plans do not fully incorporate pediatric patients into the overall planning process. Despite this, some progress has been made over the past several years through the strong advocacy of pediatric providers and pediatric organizations (5,6).
This chapter provides a brief overview of the history of pandemics as well as the current status of planning for a potential epidemic outbreak. In addition, the US response plans, from the federal to the community health-care level, are reviewed here. The majority of the chapter is devoted to discussing issues specific to hospital planning with a focus on pediatric critical care and strategies to mitigate the potential impact of a future pandemic. Next, the chapter reviews proposed triage and surge plans that would be required under both pandemic conditions as well as unique situations such as an Ebola epidemic and the unique limitations faced by pediatric critical care in both scenarios. Finally, we will introduce the ethical challenges that will arise as a result.
History
The 2009 H1N1 influenza virus produced the first pandemic to test the limits of modern medical care of this era. According to data collected by the World Health Organization (WHO), the virus emerged in Mexico and eventually reached 214 countries (7). The United States alone saw roughly 60.8 million cases with 12,468 deaths (8).
The younger population had no previous immunity to the virus, unlike those >60 years who likely had exposure earlier in their lives, leaving young adults and children most susceptible. Children saw a significantly higher impact from H1N1 with an attack rate nearly 7 times higher than seasonal influenza outbreaks in years past (8). A review of the pediatric deaths in the United States due to H1N1 influenza showed that the majority of children impacted were >5 years of age and that many had previous medical conditions (9). This put significant strain on children’s hospitals as the peak occurred during respiratory viral season when most inpatient units were near capacity.
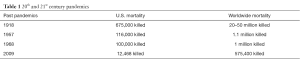
Although the 2009 H1N1 pandemic swept the globe with significant morbidity and mortality, this does not seem to compare with the severity of the 1918 influenza pandemic (Table 1). Often described as the single deadliest event in history, it is estimated that one third of the world’s population was infected with the novel virus with the overall death of roughly 50 million people (10). Children five years of age and less had the highest mortality rate, most resulting from secondary bacterial infections for which there were not yet antimicrobial treatments (11).
Full table
The most recent emerging infection to cause scientists, medical providers and policymakers to reassess current pandemic planning has been the Ebola outbreak of 2014–2015. While it was nearly completely limited to the population of Guinea, Liberia and Sierra Leone in West Africa, this virus infected 28,616 people with 11,310 deaths (12). Previous Ebola outbreaks had occurred in Africa but this outbreak resulted in 36 cases and 15 deaths outside of West Africa with 11 people treated in the United States, 4 of whom contracted the virus outside of West Africa (13). This has prompted local, state, and national agencies to make huge investments into the preparation for pandemics in the future.
Government and international planning and support
The overarching federal pandemic response plan for the United States was released by the Homeland Security Council in November 2005 and was based on three pillars: preparedness and communication, surveillance and detection, and response and containment (14). In 2013 the United States Congress reauthorized the Pandemic and All-Hazards Preparedness Reauthorization Act, Public Law 113-5, which covers public health security and all-hazards preparedness. Included in the reauthorization was important language ensuring that both critical care and pediatric planning were included in national planning and response efforts. The Assistant Secretary for Preparedness and Response is the federal agency responsible for coordinating national efforts in this area. A variety of federal, state, and local response plans have been created along with various international plans. Unfortunately, several of the plans being generated use slightly different terminology and triggers for responses, which can lead to confusion.
As of June 2008, all 50 US states have completed pandemic influenza plans. A Government Accountability Office review at the time identified “major gaps” in 16 of 22 categories. The plans of the 5 most populous states were reviewed closely. Urban and rural community plans from each of those states were reviewed as well (15). Facilitation of medical surge (adequate treatment of vastly increased numbers of patients under mass-casualty or pandemic conditions) and fatality management were among the major gaps identified in the majority of plans. Mass vaccination, distribution of antiviral agents, public health continuity-of-operation plans, and community health-care coalitions were among the major gaps less commonly identified. Medical surge, fatality management, and community containment measures were 3 of the major areas in which state and local officials desired additional federal guidance.
Unfortunately, although progress in pediatric specific planning has been made as mentioned in the introduction, important gaps remain. In 2010, the National Commission on Children and Disasters delivered a comprehensive report with specific recommendations to the United States Congress that examined and assessed the needs of children for preparedness, response, and recovery from all hazards, including major disasters and emergencies (16). A 2015 report by Save the Children found that 79% of the National Commission on Children in Disasters’ recommendations remain unfulfilled as well as demonstrating that less than one cent out of every ten dollars in federal emergency preparedness grants is directed toward activities targeting children’s safety (17). Improvements in funding for pediatric disaster planning is critical in light of the relative lack of day to day pediatric readiness, again improved from earlier studies, that many emergency departments in the United States currently demonstrate (18).
The ability to respond to an increase in demand, which exceeds the normal, is referred to as surge capacity. This includes things such as push-packs (pre-packed supplies held in reserve to meet increased demand), overflow of patients outside of typical care areas such as mechanically-ventilated patients in the post-anesthesia care unit (PACU) in addition to the intensive care unit (ICU), use of personnel typically assigned to other areas transferred to the ICU, and triage of both patient disposition and allocation of resources such as ventilators and neuraminidase inhibitors (19). Integration of other areas of the hospital beyond the emergency department and the pediatric intensive care unit (PICU) into surge planning is vital and should include the neonatal intensive care unit (NICU) as well as other areas (20). Rapid acquisition of local clinical and epidemiologic data during an influenza pandemic may help establish reliable early estimates of critical care resource utilization and guide whether contingency measures will be needed to accommodate the influx of patients (21). An important development in pediatric disaster planning has been the creation of voluntary regional coalitions designed to help healthcare systems prepare and respond using coordinated medical resources during emergencies and disasters. Examples include coalitions that are pediatric focused (Mountain States Pediatric Disaster Coalition) or those where pediatrics is well integrated into the greater coalition (Northwest Healthcare Response Network) (Table 2). There are a wide variety of helpful planning, pediatric specific, guidelines and tools to assist local and regional planning with several useful resources summarized in Table 2.

Full table
Logistics and pediatric critical care planning
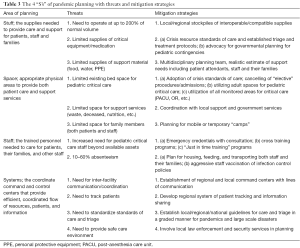
Four tenants of disaster planning have been described as stuff, space, staff and systems (Table 3) (22,23). Stuff is the supply needed to provide care. Space is the appropriate physical space to provide critical care as well as sufficient space to provide other services such as triage, temporary housing, storage and tracking of patient remains, and waste disposal. Staff refers not just to providers and nurses but all support services needed to care for patients, families, and staff. Systems are the coordinated command and control centers and supporting services that provide efficient, coordinated flow of resources, patients, and information. This section will focus on these 4 areas as well as considerations for direct patient care in the management of critically ill children in pandemics. As we cover the 4 S’s of logistics it is important to remember pediatric pandemic preparedness, while improving, is still lacking, and therefore requires significant involvement and advocacy from those dedicated to the care of children (5,6).
Full table
Crisis standards of care
Prior to discussion of the medical care of pediatric patients in a pandemic it is important to consider crisis standards of care (CSC). CSC were defined by an Institute of Medicine working group as “a substantial change in usual healthcare operations and the level of care it is possible to deliver, which is made necessary by a pervasive (e.g., pandemic influenza) or catastrophic (e.g., earthquake, hurricane) disaster.” (24). Their recommendation is that this declaration come from a state or federal agency under emergency circumstances. This declaration should enable specific legal and regulatory protections for health care providers when having to operate under conditions of limited medical resources and alternate models of care. It is reasonable to incorporate this concept into local facility plans as well to provide similar guidance and protections for staff in the absence of a formal declaration. Examples of medical operations under these standards are discussed below but design and implementation of these standards for each agency should be planned prior to a crisis and remain flexible based on each situation.
Stuff
When considering stuff it is important to remember under most circumstances that hospitals will retain only enough supplies for 3–5 days of normal operations. In the setting of a pandemic hospital operations may need to run at 100% to 200% above normal for a pandemic response (25). In the ICU this pace is likely to be sustained for weeks to months (26-29). Those items that require special attention are non-substitutable items such as ventilators and their circuits, N95 masks, and certain medications. In addition to local facility stockpiling with a 5–10 day supply of these items, dual sourcing of the same items should also be considered (30).
Both the Chest Consensus Statement and European Society of Intensive Care statement on pandemics recommend a regional approach to the management of critical supplies (31,32). A regional approach requires interoperable and compatible critical care supplies for hospitals in a given region (32). This approach requires that planning involve coordination within local hospital systems as well as government agencies to be effective. As will be discussed below, planning for the provision of food and shelter, not just for patients and their families but for staff members and their families, should be considered as part of this multidisciplinary approach.
Ventilators will be of critical importance and are an item that has limited surge capacity in most locations. The strategic United States national stockpile was estimated to have only around 5,000 ventilators, most of which are not effective for infants (22). Many regions rely on ventilator contracts with 1 or 2 contractors with a central repository to supply local surges. In the setting of a pandemic, all local ICUs are likely to be operating at capacity and this may limit supply. With the H1N1 pandemic, a study comparing outcomes in Mexico and Canada found up to 97% of patients in the ICU required mechanical ventilation and a higher mortality in Mexico. Less ventilator availability was postulated to be one of the possible causes of the difference in mortality (33). Hospitals and systems should establish protocols both amongst facilities and amongst patients in a given facility regarding triage and critical supply allocation (including ventilators) prior to a pandemic while developing CSC.
Critical pharmaceutical availability should also be considered and planned for in a multidisciplinary manner. Critically ill children with influenza treated with neuraminidase inhibitors early in their course had improved outcomes in California in the 2009 H1N1 outbreak (34). While it is difficult to predict which medications will be effective or needed in a pandemic, partnering with pharmacy services in planning is essential to developing an informed and adaptive system. When developing a list of critical medications to stockpile or allocate, the planners should consider a narrow group of broadly applicable critical care medications such as vasopressors, sedatives and selected antimicrobials for stockpiling (23).
Personal protective equipment (PPE) should not be overlooked when planning for a pandemic. N95 masks or powered air purifying respirators as well as appropriate gowns and gloves will be critical and require ongoing training or “just in time” training programs to be used effectively (35). Notably, during the care of just 2 patients with Ebola, each patient created over 1,000 pounds of solid waste, most of which was PPE (36). This highlights that not just the volume of acquisition of PPE potentially needed but that proper planning for both its use and disposal is critical during the planning phase.
Space
Planning for the care of patients in pandemics or large scale disasters suffers from a lack of existing evidence as well as barriers to future and real time study (37,38). This paucity of data is even more evident when planning for the care of critically ill children. There are roughly 80,000 adult ICU beds and 357 pediatric intensive care units with a median of 12 beds in the US with significant regional variation in per capita beds and PICU trained staff (39-41). The low relative number of dedicated pediatric beds coupled with high variability in pediatric care specialist density could lead to significant shortage of specialty care in a pandemic setting. In New York City, a simulation of a disaster found inadequate PICU capacity for a moderate disaster without CSC and in a large scale disaster even with CSC there was not adequate capacity to meet the demands (42).
Several strategies are possible to augment PICU capacity. The use of CSC including limiting care to “essential” interventions only and controlling distribution of patients, in a quantitative model led to a 47% reduction in predicted mortality and an increase in ability to meet the care needs of children in separate pandemic simulations (2,43). Both Chest and European pandemic Task Forces recommended several strategies to include in CSC to improve care and resource management in pandemics such as remote expert consultation, dedicated pediatric surge personnel including pediatric hospitalists and others, utilization of all monitored beds, emergency credentialing and “just in time” consultation for pediatric care (25,31,32,44). In practice, this would utilize facilities that typically do not care for critically ill pediatric patients to do so. A small community or critical access hospital would utilize regional expert consultation to augment emergency credentialing for local adult intensivists, respiratory therapists, pediatric hospitalists, and nurses to care for critically ill pediatric patients.
In conjunction with the above strategies, expansion of services at established pediatric centers can augment capacity. With the H1N1 pandemic, the increase in need for critical care services proportionally exceeded the need for traditional hospital services (45). This would also likely be the case with future pandemics. Facilities that traditionally care for critically ill children could expand services by allocating non-traditional monitored spaces for PICU care such as the post-anesthesia recovery unit, operating rooms, or other suitable monitored settings (23,31). Additionally these facilities could set up “satellite” units in the alternative locations to care for critical patients not effected by the pandemic to group contagious patients, cohort staff, and protect non-infected patients (23).
The incredible volume of waste with just 2 highly infectious patients with Ebola (36) demonstrates the need for consideration of ancillary service directed thinking while planning for space in a pandemic. Allocation of adequate space for safe, respectful care of the deceased should also be addressed when looking at systems and space (46). Additionally, consideration should be given to locations and facilities to shelter and feed families of ill patients, staff members, and potentially families of staff members (32).
Staff
Another limiting factor in caring for critically ill pediatric patients is trained staff. There are 1,976 pediatric critical care diplomates in good standing in the US with significant variability in density state to state from zero to 1:30,000 children (41). A strategy to augment these regional potential shortages should include utilization of emergency credentialing and either local or telephonic consultation for non-pediatric critical care trained providers as mentioned above (31,32,44). Equally important is preparation for nursing care. Regular cross training of nursing staff as well as “just in time” training should be in place and has demonstrated effectiveness (32,47). Local database tracking of training and skill sets of all nursing staff would augment the ability to “flex” appropriately cross-trained staff. Comprehensive ongoing training and documentation of legal protection of staff working outside their normal domains should be in place within institutional CSC and should not be overlooked (31). Reduction of in-efficiencies typically encountered in hospital care should be considered for elimination. Examples of such reduction which have demonstrated effectiveness would be recall of trainees from off-site or non-clinical rotations and elimination of educational rounds (23,48).
In addition to a baseline limitation in critical care trained staff, the circumstances of a pandemic would likely further limit staffing. Illness, fatigue, fear, and care giver duties would all limit staff availability (23). Staff absenteeism will likely at least reflect the attack rate of the pandemic and may be as high as 60% particularly with closure of schools as would likely be seen in a pandemic (49). To mitigate staff shortages hospitals may have to provide for the rest, shelter, nutrition and transportation needs of staff as well as their families (32). Staff training on appropriate infection control procedures as well as rigorous vaccination and staff health monitoring plans should also be considered to limit staff loss due to illness.
Systems
Multidisciplinary planning with pharmacy, nutritional, janitorial, security, respiratory, and local government services and community leaders in “table top” exercises is critical in identifying vulnerabilities. Planning with this multi-disciplinary approach is key not only for preparing for a pandemic but in developing the relationships that will enable critical communications in a pandemic. A command structure with clearly defined roles and lines of communication should be defined prior to a pandemic and can be part of these exercises (31,50). These structures should have the ability to coordinate expansion or restriction of critical care resources (i.e., CSC implementation) in conjunction with local medical directors, help coordinate “just in time” training as well as regional expert consultation (i.e., tele-consultation with pediatric specialists), facilitate the flow of critical equipment and patients, and communicate CSC on both a local and regional level.
Along with the establishment of local and regional command centers to coordinate, it is vital that clear lines of communication exist for dissemination of critical information. This requires: (I) the ability to maintain power, particularly at austere or atypical sites of care; (II) the ability to rapidly download a transferrable version of clinical information; (III) that the systems exist to efficiently share this information with staff; (IV) that the communication be consistent and the information be trusted by staff (30,48,51).
The 2014 Chest Task Force also recommended that these command centers consider transfer of assets rather than patients in the setting of a pandemic (32) which may have particular impact on the care of specialized patients such as children. These local and regional command centers should also help plan and coordinate a system for patient tracking, identification, and the ability to communicate with family members and next of kin regarding status and location of loved ones (30). Local government resources may be able to assist in this as well as security for facilities, staff, patients, and families. Given high levels of stress, limited resources, potentially crowded living conditions, and considerable anxiety surrounding pandemic disease, coordination with security both for a facility and the ICU should be included in the planning process.
Critical care considerations
Ventilators are likely to be a major limiting factor for care in a pandemic. Eighty percent of children admitted to a PICU with H1N1 in Australia and New Zealand required mechanical ventilation (3). In a study of mostly young adults in Canada and Mexico 97% of those admitted to an ICU required mechanical ventilation and 26.7% required “rescue” oxygen therapy [nitric oxide, oscillatory ventilation, prone ventilation, or extra-corporeal membrane oxygenation (ECMO)]. In order to mitigate this threat, establishment of CSC, review of these standards in the setting of a specific pandemic, and thoughtful and ethical allocation of ventilators and other advanced support will be necessary. Additionally utilization of non-invasive ventilation or use of anesthesia machines to augment traditional ventilator supplies should be considered while developing CSC and local policies. Specification of procedures with high risk for aerosolization of potentially infectious fluids, e.g., disconnection from a vent, with suctioning, or Bag-valve mask ventilation among others, should be defined, mitigating protocols established, and training disseminated (31).
Protocols for allocation of other critical resources such as antimicrobials, vaccines, other medications as well as advanced life support measures such as ECMO, inhaled nitric oxide, and continuous veno-venous hemofiltration should be established and undergo regular review in the setting of a pandemic. One center during the H1N1 pandemic described the effective use of a trauma ECMO program providing surge resources for a broad spectrum of patients, including children, with 60% overall survival (52). The authors describe a multi-disciplinary approach utilizing staff mentoring and “just in time” training to achieve good outcomes. The decision to offer these resource intensive modalities should be considered in the planning phase and throughout a pandemic and be based on need, local resources, and experience. When establishing antimicrobial and vaccine utilization, inclusion of healthcare staff in the pool of those eligible to receive these limited resources should not be overlooked.
Triage and surge planning
Hospital resource utilization clearly could be overwhelmed should a pandemic occur. Although it is impossible to predict the exact number of patients and to what severity they would be affected, it is important to have a basic, initial triage plan in place to permit the most efficient use of limited resources to deliver care to the most patients possible (19). This concept results in a significant paradigm shift from normal healthcare operations to CSC. When CSC are implemented, the goal is to improve population outcomes by distributing resources to those most likely to survive (53).
Although the primary focus of this chapter is pandemic preparation in the ICU setting, triage typically occurs prior to PICU admission. Thus, it is imperative that triage planning include local outpatient clinics and emergency departments to prevent overuse of higher levels of care during the initial phase of a pandemic. Ideally, there would be a triage algorithm to validate a patient’s need for scarce ICU resources while CSC are in place. Integration of the multi-disciplinary approach including the ICU is important during the planning phase.
As previously discussed, for a variety of reasons children tend to represent a disproportionate patient population during epidemics. Despite this knowledge, current literature on triage planning has predominantly focused on the adult population. The Task Force for Mass Critical Care recommended the Sequential Organ Failure Assessment score (SOFA) for triage of critically ill adult patients (22,54). Application of adult triage guidelines to children is limited in many ways. Primarily, adult algorithms such as the SOFA score, focus on mortality. However, the specific risk factors for death in adults do not inherently apply to children. In general, children admitted to a PICU have an overall low mortality rate relative to adults, so triage tools that exclude patients based on high risk of death are thus unlikely to actually decrease demand of limited resources when applied to pediatric patients (27).
A pediatric-specific pandemic triage plan was developed by Gall and colleagues to guide admission to the PICU during periods of CSC (27). This retrospective study used VPS data (Virtual PICU Systems, a widely used PICU database) to simulate critically ill patient volumes and outcomes during a pandemic. The data was used to describe mortality and resource utilization based on probability of death and days on mechanical ventilation. Use of the proposed triage model described in the article resulted in greater population survival compared to a “first come first served” distribution model of resources. Though there are limitations to the use of simulation data, this tool provides an evidence based, ethical framework for pediatric triage in disaster situations and hopefully will promote further work in this field.
Pandemic planning committees will need to use such triage tools in the context of their own staffing and resource availability to establish straightforward triage criteria for the utilization for critical care resources. Current day-to-day practices are rarely affected by the need to ration resources. However, the threat of the next pandemic will require dramatic changes in the practices we have habituated. The necessity for some patients to transition to palliative care is an ethically challenging decision for providers and an overwhelming emotional burden to families and would require appropriate support for all involved. It is vital that facilities establish ethically sound triage policies both for entry into an ICU and for advanced care once patients arrive to the ICU to mitigate emotional distress of staff as much as possible. When establishing triage protocols it is also important to involve legal services to provide input and coverage for clinicians implementing the policies decided upon by the institution.
Special cases
In September 2014, the first case of Ebola virus disease (EVD) to be diagnosed on American soil revealed multiple gaps in preparedness of healthcare systems to handle outbreaks of highly infectious pathogens (55). Lack of awareness resulted in misdiagnosis on initial presentation and when the patient returned severely ill two days later, staff were underprepared and ill-equipped to uphold optimal isolation precautions. Two healthcare workers were unfortunately secondarily infected (56).
The highly infectious and lethal nature of EVD along with the lack of proven therapy, make it a unique threat. Such pathogens are rare and are often not considered in the initial differential diagnosis. To allow for appropriate triage and identification of at risk patients, pediatric emergency clinicians and intensivists need to maintain working relationships with infectious disease and epidemiologic specialists to maintain awareness of active threats and to permit rapid dissemination of reliable information released by agencies such as the Centers for Disease Control, World Health Organization and the Infectious Disease Society (55) Additional education measures taken at a pediatric specific care center during the 2014 EVD outbreak included hospital wide grand rounds, mandatory online training courses, and frequent education seminars for clinical staff and families (57).
Heightened awareness can ultimately support the primary objective of preventing further spread of infection. For such virulent pathogens, “enhanced infection control” measures should be implemented (58). Proactive coordination with nearby facilities should be arranged to ensure procurement of adequate supply of appropriate PPE with stockpile established in the planning phase (57). In addition, training is required to educate staff on appropriate donning/doffing of PPE. “Just in time” training should always be part of preparation during epidemics but having a protocol with periodic rehearsals may permit maintenance of proficiency particularly when preparing for highly infectious or lethal outbreaks (55). Staffing is also an important component of infection control. Recently derived care models recommend teams of 5 nurses, 1 as the designated PPE adherence monitor with the other 4 divided into pairs alternating in two hours shifts to avoid fatigue while working in full PPE (57). This altered staffing model for highly infectious pathogens greatly exceeds the traditional and CSC staffing models as mentioned above and should be considered in planning for staff. Logistical actions to provide a supportive framework for the clinical care team are also necessary. A primary logistical concern is the handling of infectious waste. For EVD, category A waste, defined as an infectious substance regulated as a hazardous material under the U.S. Department of Transportation (DOT) Hazardous Materials Regulations (HMR; 49 CFR, Parts 171–180), precautions should be taken until the patient’s infection status is confirmed (59).
It is certain that outbreaks of this type will continue to occur. Although the timing is unpredictable, past experiences with other unique infectious threats such as EVD, Middle Eastern Respiratory Syndrome coronavirus (MERS-CoV), and Severe Acute Respiratory Distress Syndrome (SARS-CoV) have demonstrated the need for improved preparedness with proactive education and training.
Ethics
As we prepare for the next pandemic or disaster, we are forced to alter our medical decision making to that of a system with limited resources, which is not something we are routinely accustomed to in developed areas. Although every effort should be made to deliver care that is equal to standard practice, this may not be possible due to limited resources (60). It is imperative that planning how scarce resources will be allocated to a population be completed prior to a pandemic, as these decisions cannot be made fairly on an individual basis at the time of presentation. In 2009, the Institute of Medicine published guidelines to aid in establishing CSC for disaster planning (61). Determining the criteria for allocating resources must be clear and easily attainable. Applying an ethical framework to preparedness plans rely on taking either a utilitarian or egalitarian model. The utilitarian model focuses on providing care to the highest number of patients, while the egalitarian model centers on providing resources to those who need them most. Most have created plans with a hybrid approach, delineating out those that will not survive even with aggressive treatment and those that will survive even without any treatment. The remainder of the patients can then be triaged based on utilitarian guidance (62). No ethical model or framework is perfectly suited to delineate allocation of resources in times of scarce resources which places high priority on eliciting provider and community involvement during disaster planning.
Conclusions
History as well as population expansion and rapid global transit make the emergence of a pandemic a virtual certainty. History also shows us that children are likely to be disproportionately affected and that planning for children in pandemics and disasters, while improving, is still lacking. While the exact nature of the next pandemic cannot be predicted, careful attention to planning in a multi-disciplinary manner engaging national, regional and local agencies can help mitigate both morbidity and mortality. Focus on stuff, space, staff, and systems in the planning phase can focus protocols and stockpiling. Careful attention to triage and surge planning with a sound ethical and legal framework can help maintain an agile and effective system. Consideration of potentially very highly infectious and lethal pandemics makes planning and eventual response more robust and flexible. In the words of Dwight D. Eisenhower, “In preparing for battle I have always found that plans are useless, but planning is indispensable.” Any plan for pediatric care in a pandemic will be imperfect but should afford the relationships, flexibility and knowledge to adapt to an ever changing threat.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: LTC Hamele and CPT Neumayer are officers in the United States Army. The views in this article are their own and do not reflect the views of the United States Army, Department of Defense, or the United States Government.
References
- Hick JL, Rubinson L, O’Laughlin DT, et al. Clinical review: Allocating ventilators during large-scale disasters - Problems, planning, and process. Crit Care 2007;11:217. [Crossref] [PubMed]
- Kanter RK. Pediatric mass critical care in a pandemic. Pediatr Crit Care Med 2012;13:e1-4. [Crossref] [PubMed]
- Yung M, Slater A, Festa M, et al. Pandemic H1N1 in Children Requiring Intensive Care in Australia and New Zealand During Winter 2009. Pediatrics 2011;127:e156-63. [Crossref] [PubMed]
- Fowlkes AL, Arguin P, Biggerstaff MS, et al. Epidemiology of 2009 pandemic influenza A (H1N1) deaths in the United States, April-July 2009. Clin Infect Dis 2011;52 Suppl 1:S60-8. [Crossref] [PubMed]
- AAP Disaster Preparedness Advisory Council Committee on Pediatric Emergency Medicine. Ensuring the health of children in disasters. Pediatrics 2015;136:e1407-17. [Crossref] [PubMed]
- Dziuban EJ, Peacock G, Frogel M. A Child’s Health Is the Public’s Health: Progress and Gaps in Addressing Pediatric Needs in Public Health Emergencies. Am J Public Health 2017;107:S134-7. [Crossref] [PubMed]
- World Health Organization. Pandemic (H1N1) 2009. Weekly Update. August 6, 2010. [Internet]. [cited 2018 May 5]. Available online: http://www.who.int/csr/disease/ebola/en/
- Shrestha SS, Swerdlow DL, Borse RH, et al. Estimating the burden of 2009 pandemic influenza a (H1N1) in the United States (April 2009-April 2010). Clin Infect Dis 2011;52 Suppl 1:S75-82. [Crossref] [PubMed]
- Cox CM, Blanton L, Dhara R, et al. 2009 Pandemic influenza A (H1N1) deaths among children - United States, 2009-2010. Clin Infect Dis 2011;52:S69-74. [Crossref] [PubMed]
- Centers for Disease Control and Prevention. Past Pandemics. [Internet]. Available online: https://www.cdc.gov/flu/pandemic-resources/basics/past-pandemics.html
- Kilbourne ED. Influenza pandemics of the 20th century. Emerg Infect Dis 2006;12:9-14. [Crossref] [PubMed]
- World Health Organization. Ebola outbreak 2014-2015. Available online: http://www.who.int/csr/disease/ebola/en/
- CDC. 2014-2015 Ebola Outbreak in West Africa [Internet]. 2017 [cited 2018 Aug 29]. Available online: https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html
- Homeland Security Council. National strategy for pandemic influenza. [Internet]. [cited 2018 Mar 28]. Available online: https://www.cdc.gov/flu/pandemic-resources/pdf/pandemic-influenza-strategy-2005.pdf
- Government Accountability Office. Influenza pandemic:federal agencies should continue to assist states to address gaps in pandemic planning [report]. [Internet]. [cited 2018 Mar 28]. Available online: https://www.gao.gov/new.items/d09909t.pdf
- National Commission on Children and Disasters. 2010 Report to the President and Congress. [Internet]. 2010 [cited 2018 Mar 28]. Available online: https://archive.ahrq.gov/prep/nccdreport/nccdreport.pdf
- Save the Children. Still at Risk: U.S. Children 10 Years After Hurricane Katrina. 2015 National Report Card on Protecting Children in Disasters. 2015.
- Gausche-Hill M, Ely M, Schmuhl P, et al. A national assessment of pediatric readiness of emergency departments. JAMA Pediatr 2015;169:527-34. [Crossref] [PubMed]
- Sweney J, Poss WB. Pandemic influenza and pediatric critical care preparedness. In: Curr concepts Pediatr Crit care. Society of Critical Care Medicine. Mount Prospect, IL, USA. 2009.
- Barfield WD, Krug SE. Disaster preparedness in neonatal intensive care units. Pediatrics 2017.139. [PubMed]
- Stockmann C, Ampofo K, Hersh AL, et al. Local health department influenza surveillance estimates and projections of peak pediatric intensive care unit occupancy during the 2009 influenza A pandemic. J Pediatric Infect Dis Soc 2013;2:405-6. [Crossref] [PubMed]
- Christian MD, Devereaux AV, Dichter JR, et al. Definitive care for the critically ill during a disaster: Current capabilities and limitations: From a Task Force for Mass Critical Care Summit Meeting, January 26-27, 2007, Chicago IL. Chest 2008;133:8S-17S. [Crossref] [PubMed]
- Hota S, Fried E, Burry L, et al. Preparing your intensive care unit for the second wave of H1N1 and future surges. Crit Care Med 2010;38:e110-9. [Crossref] [PubMed]
- Stroud C, Altevogt BM, Nadig L. Crisis Standards of Care: Summary of a Workshop Series [Internet]. Washington DC; 2010. Available online: https://www.ncbi.nlm.nih.gov/books/NBK32753/pdf/Bookshelf_NBK32753.pdf
- Hick JL, Einav S, Hanfling D, et al. Surge capacity principles: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014;146:e1S-16S. [Crossref] [PubMed]
- ANZIC Influenza Investigators, Webb SA, Pettilä V, et al. Critical Care Services and 2009 H1N1 Influenza in Australia and New Zealand. N Engl J Med 2009;361:1925-34. [Crossref] [PubMed]
- Gall C, Wetzel R, Kolker A, et al. Pediatric Triage in a Severe Pandemic: Maximizing Survival by Establishing Triage Thresholds. Crit Care Med 2016;44:1762-8. [Crossref] [PubMed]
- Ercole A, Menon DK, O’Donnell DR. Modelling the impact of pandemic influenza A(H1N1) on UK paediatric intensive care demand. Arch Dis Child 2009;94:962-4. [Crossref] [PubMed]
- Stiff D, Kumar A, Kissoon N, et al. Potential pediatric intensive care unit demand/capacity mismatch due to novel pH1N1 in Canada. Pediatr Crit Care Med 2011;12:e51-7. [Crossref] [PubMed]
- Tosh PK, Feldman H, Christian MD, et al. Business and continuity of operations: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014;146:e103S-17S. [Crossref] [PubMed]
- Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mas. Intensive Care Med 2010;36:428-43. [Crossref] [PubMed]
- Einav S, Hick JL, Hanfling D, et al. Surge capacity logistics: Care of the critically ill and injured during pandemics and disasters: Chest consensus statement. Chest 2014;146:e17S-43S. [Crossref] [PubMed]
- Dominguez-Cherit G, De La Torre A, Rishu A, et al. Influenza A (H1N1pdm09)-Related Critical Illness and Mortality in Mexico and Canada, 2014. Crit Care Med 2016;44:1861-70. [Crossref] [PubMed]
- Louie JK, Yang S, Samuel MC, et al. Neuraminidase inhibitors for critically ill children with influenza. Pediatrics 2013;132:e1539-45. [Crossref] [PubMed]
- Tompkins BM, Kerchberger JP. Personal protective equipment for care of pandemic influenza patients: A training workshop for the powered air purifying respirator. Anesth Analg 2010;111:933-45. [PubMed]
- Lowe JJ, Gibbs SG, Schwedhelm SS, et al. Nebraska Biocontainment Unit perspective on disposal of Ebola medical waste. Am J Infect Control 2014;42:1256-7. [Crossref] [PubMed]
- Ortiz JR, Rudd KE, Clark DV, et al. Clinical research during a public health emergency: A systematic review of severe pandemic influenza management. Crit Care Med 2013;41:1345-52. [Crossref] [PubMed]
- Burns KEA, Rizvi L, Tan W, et al. Participation of ICUs in critical care pandemic research: A province wide, cross-sectional survey. Crit Care Med 2013;41:1009-16. [Crossref] [PubMed]
- Wallace DJ, Angus DC, Seymour CW, et al. Critical care bed growth in the United States: A comparison of regional and national trends. Am J Respir Crit Care Med 2015;191:410-6. [Crossref] [PubMed]
- Odetola FO, Clark SJ, Freed GL, et al. A National Survey of Pediatric Critical Care Resources in the United States. Pediatrics 2005;115:e382-6. [Crossref] [PubMed]
- American Board of Pediatrics Inc. American Board of Pediatrics Inc., 2015-2016 Workforce Data. Chapel Hill, NC; 2016.
- Kanter RK, Moran JR. Pediatric hospital and intensive care unit capacity in regional disasters: expanding capacity by altering standards of care. Pediatrics 2007;119:94-100. [Crossref] [PubMed]
- Kanter RK. Strategies to improve pediatric disaster surge response: Potential mortality reduction and tradeoffs. Crit Care Med 2007;35:2837-42. [Crossref] [PubMed]
- Dries D, Reed MJ, Kissoon N, et al. Special Populations. Chest. 2014;146:e75S-86S. [Crossref] [PubMed]
- Louie JK, Gavali S, Acosta M, et al. Children hospitalized with 2009 novel influenza A(H1N1) in California. Arch Pediatr Adolesc Med 2010;164:1023-31. [Crossref] [PubMed]
- World Health Organization. WHO checklist for influenza pandemic preparedness planning. Epidemic Alert & Response. Switzerland; 2005.
- Zangrillo A, Biondi-Zoccai G, Landoni G, et al. Extracorporeal membrane oxygenation (ECMO) in patients with H1N1 influenza infection: a systematic review and meta-analysis including 8 studies and 266 patients receiving ECMO. Crit Care 2013;17:R30. [Crossref] [PubMed]
- Ratnapalan S, Martimianakis MA, Cohen-Silver JH, et al. Pandemic management in a pediatric hospital. Clin Pediatr (Phila) 2013;52:322-8. [Crossref] [PubMed]
- Wise RA. The Creation of Emergency Health Care Standards for Catastrophic Events. Acad Emerg Med 2006;13:1150-2. [Crossref] [PubMed]
- Dichter JR, Kanter RK, Dries D, et al. System-level planning, coordination, and communication: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014;146:e87S-102S. [Crossref] [PubMed]
- Devereaux AV, Tosh PK, Hick JL, et al. Engagement and Education: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014;146:e118S-33S. [Crossref] [PubMed]
- Michaels AJ, Hill JG, Bliss D, et al. Pandemic flu and the sudden demand for ECMO resources: A mature trauma program can provide surge capacity in acute critical care crises. J Trauma Acute Care Surg 2013;74:1493-7. [Crossref] [PubMed]
- Committee on Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations; Institute of Medicine. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington DC; 2012.
- Christian MD, Sprung CL, King MA, et al. Task force for mass critical care: triage: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014;146:e61S-74S. [Crossref] [PubMed]
- Chertow DS, Palmore TN, Masur H. Critical Care Medicine after the 2014-2015 Ebola Outbreak: Are We Ready if It Happens Again? Crit Care Med 2016;44:457-9. [Crossref] [PubMed]
- Liddell AM, Davey RT, Mehta AK, et al. Characteristics and clinical management of a cluster of 3 patients with Ebola virus disease, including the first domestically acquired cases in the United States. Ann Intern Med 2015;163:81-90. [Crossref] [PubMed]
- DeBiasi RL, Song X, Cato K, et al. Preparedness, evaluation, and care of pediatric patients under investigation for ebola virus disease: Experience from a pediatric designated care facility. J Pediatric Infect Dis Soc 2016;5:68-75. [Crossref] [PubMed]
- Centers for Disease Control and Prevention: Ebola Virus Disease. Guidance on PPE [Internet]. Available online: http://www.cdc.gov/vhf/ebola/healthcare-us/ppe/guidance.html
- Centers for Disease Control and Prevention: Ebola Virus Disease. Guidance on Waste Management [Internet]. [cited 2018 Apr 23]. Available online: https://www.cdc.gov/vhf/ebola/healthcare-us/cleaning/waste-management.html
- Centers for Disease Control and Prevention. Ethical Considerations for Decision Making Regarding Allocation of Mechanical Ventilators during a Severe Influenza Pandemic or Other Public Health Emergency. [Internet]. [cited 2018 May 5]. Available online: https://www.cdc.gov/flu/pandemic-resources/basics/past-pandemics.html
- Altevogt BM, Stroud C, Hanson SL, et al. Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report. The National Academies Press. Washington DC; 2009.
- Tabery J, Mackett CW. Ethics of triage in the event of an influenza pandemic. Disaster Med Public Health Prep 2008;2:114-8. [Crossref] [PubMed]


