Improving transitions of care between the operating room and intensive care unit
Introduction
The Institute of Medicine (IOM) released a report in 1999 entitled “To Err Is Human: Building a Safer Health System”, which estimated that as many as 98,000 people die each year due to medical errors (1). Eighteen months after the publication of “To Err Is Human”, the IOM released a second, more comprehensive report entitled “Crossing the Quality Chasm” that heightened awareness about significant quality of care deficits that existed in the US health care delivery system at that time (2). Both reports served as a clarion call for national efforts to improve patient safety, and both reports identified the intensive care unit (ICU) and operating room (OR) suite as potential danger spots in the hospital—areas with the highest risk of potential adverse safety events. For example, the Critical Care Safety Study prospectively gathered data on the number and types of adverse events occurring in the ICU at an academic medical center over the course of 1 year. Potentially life-threatening errors, at least half of which were thought to be preventable, were relatively common, affecting 20% of all patients. Hand-offs were a particularly dangerous time, as many errors occurred during the transition of care from one provider to the next (3). Hand-offs are formally defined as “the exchange between health professionals of information about a patient accompanying either a transfer of control over, or responsibility for the patient” (4).
While all transitions and hand-offs of care (e.g., shift hand-offs) are critical moments of risk to the patient, the OR to ICU hand-off is a particularly dangerous time for the patient. Hand-offs of care between the OR and ICU teams during this key transition period require detailed communication of complete and accurate patient information at a time when the patient is perhaps most vulnerable, the immediate post-operative period. Importantly, the communication of essential clinical information has to occur while the teams continue to provide care. There are a number of important priorities that must occur during this transition that are particularly relevant to preventing harm. Note that these are not necessarily listed in order of importance; rather, these events must occur more or less simultaneously:
- transfer monitoring equipment from the OR system to the transport system and then from the transport system to the ICU system in a relatively short period of time (i.e., less than 10 minutes);
- secure and maintain all vascular access devices, drainage tubes and catheters, and (frequently) the tracheal tube;
- identify and confirm all medication dosages (which also includes ongoing administration of medications and a discussion of ongoing medication treatment plans during the postoperative period);
- maintain adequate levels of sedation and analgesia;
- provide cardiorespiratory and hemodynamic support;
- transition the care of the patient from the OR team to the ICU team.
Unfortunately, the frequency of adverse events from OR to ICU hand-offs is not well documented, perhaps due to malpractice risk concerns. There are, however, a number of studies showing that communication between healthcare providers during hand-offs is poor and frequently leads to error (5-8). For example, a recent review of 146 surgical errors revealed that 28% of the errors were causally related to poor communication during hand-offs (5).
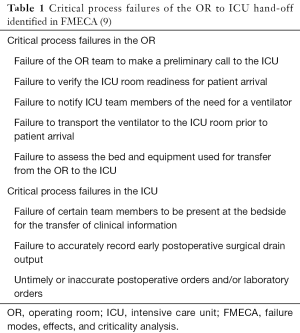
Failure modes, effects, and criticality analysis (FMECA)
FMECA is a technique developed by the US Department of Defense in 1949 and widely used by a number of high-risk industries, such as the nuclear power industry, to define key processes, as well as identify and mitigate risks. Using this technique, one group of investigators (9) conducted a series of ethnographic observations of 5 OR to ICU hand-offs and then followed their observations with several meetings with relevant stakeholders in order to generate a process map describing the OR to ICU hand-off process following liver transplantation. The actual hand-off process could involve up to 12 different clinicians performing multiple simultaneous workflows during a process that required a total of 37 different and unique steps. Working with both the surgical and ICU teams, these investigators subsequently identified the failures associated with each step of the process, as well as the frequency of occurrence, cause, potential effects, and potential safeguards. Using a 10-point scale (a low score of 1 indicates minimal risk to the process or patient, while a high score of 10 indicates maximum risk of patient harm), they calculated a risk priority number (RPN) for each failure (frequency × potential effect × safeguard), which ranged from 1 (least risk) to 1,000 (greatest risk). They defined an RPN >300 as a critical failure of the process. Importantly, 22 of the 37 (59.5%) steps had a failure with RPN >300 and were therefore considered to be critical (Table 1).
One of the critical process failures that occurred in the OR prior to transport involved a failure of the OR team to make a preliminary call to the ICU (9). Other studies have identified the importance of advance notification (a “heads up”) from the OR team prior to transport (4,10,11), which allows the ICU team to adequately prepare the ICU room to receive the patient (in terms of having the necessary equipment) and to recruit the appropriate personnel to be immediately available for the hand-off. The designated person to receive this call should be identified in advance and by protocol (ideally it should always be the same individual, e.g., the ICU charge nurse). More than one call is desirable, with advance notification occurring at minimum at 30 minutes prior to anticipated arrival and upon departure from the OR (4,9).
Ideally, the number of transports and hand-offs should be kept to a minimum (4). For example, in order to avoid transferring monitors and equipment more than twice (i.e., OR to transport, transport to ICU) and keep the number of information exchanges to a minimum, critically ill children at Cincinnati Children’s Hospital Medical Center are transported directly from the OR to the ICU without going to the post-anesthesia care unit (PACU) (Wheeler, unpublished data). One of the other critical process failures identified in the FMECA (9) was the failure of certain team members to be present at the bedside for the transfer of clinical information. The importance of having all of the key personnel present cannot be emphasized enough. At Cincinnati Children’s Hospital Medical Center, the minimum personnel that have to be present at the OR to ICU hand-off include the ICU physician (either the attending or fellow level trainee), the bedside ICU nurse, the ICU respiratory therapist, the surgeon (either the attending or fellow level trainee), the anesthesiologist (either the attending or fellow level trainee), and the OR nurse. A number of studies have demonstrated the importance of having all of the key personnel present at the hand-off (4,9-11). An important caveat to keep in mind, however, is that the surgical schedule must accommodate the time required between cases to transport the patient from the OR to the ICU, be present at the hand-off, and return back to the OR with any of the equipment that was taken to the ICU (Wheeler, unpublished data).
Finally, an additional critical process failure identified in the FMECA involved untimely or inaccurate postoperative orders (9). The clinical team in this particular study revised all of their postoperative order sets with additional representation and input from the ICU team. Ideally, the ICU physician should review and verify all of the postoperative orders with the surgeon at the bedside (4,9-11). In addition, areas of particular concern regarding decision points of the “treatment plan” and guidance on “when to call” should be discussed, clarified, and agreed upon.
Communication during hand-offs
Several studies suggest that improving hand-offs through standardized protocols and the use of checklists will reduce medical errors and potential complications (5,6,12-16). Good communication is absolutely essential to running a smooth hand-off. The information that is shared must be succinct, accurate, and complete. One of the best methods for assuring that the information is succinct involves using a standardized script. As an example, the US navy regulations prescribe the proper sequence of events to be followed during a change of command ceremony (e.g., when a new commanding officer takes over the command of a ship). All of the sailors and marines on the ship (collectively referred to as “all hands”) assemble at the quarter deck (traditionally, the part of the ship, usually at the rear or stern of the ship where the officers stood, which in modern times has become the part of the ship reserved for ceremonies) and are inspected by the departing commanding officer and the new commanding officer. The departing commanding officer usually gives a short speech and then reads his or her orders, stating that he or she is no longer to be the commanding officer of the ship. The departing commanding officer then turns to the new commanding officer, and with a salute says, “I am ready to be relieved.” The new commanding officer salutes back and states, “I relieve you.” The new commanding officer then reads his or her orders and then tells the executive officer (second in command) to continue with the ship’s routine. Every sailor and marine on the ship therefore know the exact moment in time when the new commanding officer is in charge of the ship. The hand-off is complete. Following a prescribed script assures that the exchange of information is succinct and defines the specific point in time that the care of the patient is transferred from the OR team to the ICU team.
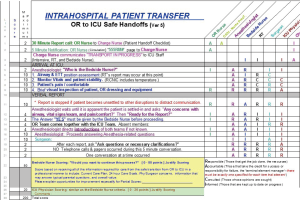
One of the best methods for assuring that the information is complete involves using a checklist. Most studies suggest that checklists improve communication and reduce errors (4-6,9-16). An additional consideration, just as important, is to minimize distractions and interruptions during the hand-off itself. The concept of the “sterile cockpit” is yet another concept borrowed from outside health care, in this case, the commercial aviation industry (17,18). The “sterile cockpit rule” is a Federal Aviation Administration regulation that states that aircraft pilots have to refrain from non-essential activities and conversations during the critical phases of flight, typically below 10,000 feet (i.e., during take-off and landing). Translated to the practice of OR to ICU hand-offs, the “sterile cockpit rule” means that only one individual is talking at a time, according to the prescribed sequence of communication and according to the previously agreed upon script. There should be no other conversations or activities during the hand-off. OR to ICU hand-offs at Cincinnati Children’s Hospital Medical Center follow a prescribed sequence that begins with the anesthesiologist’s report, followed by the surgeon’s report, and ending with a summary and recap by the intensivist (Table 2). Another advantage of the scripted dialogue was that it allowed for clarifying questions to be raised regarding the postoperative treatment plan. Each physician speaks in turn, and there are no “side-bar” conversations (Wheeler, unpublished data).

Full table
There is one last and very important issue in regards to communication, which is perhaps related more to elements of safety culture and teamwork, but is absolutely essential for a high quality OR to ICU hand-off. Communication should be respectful and professional at all times. All team members should encourage a questioning attitude—if something doesn’t sound right or if there are concerns that have not been addressed, individuals, regardless of discipline or position of authority, should be free to speak up.
How effective are pediatric OR to ICU hand-offs?
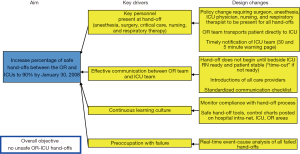
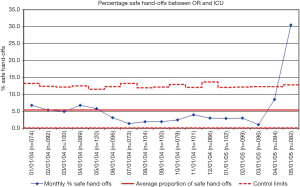
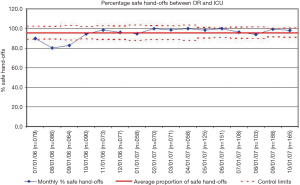
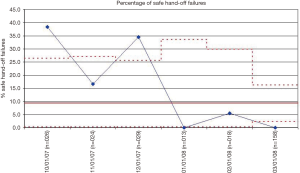
There have been a number of efforts directed at improving the quality of communication and reducing medical errors during OR to ICU hand-offs in the pediatric literature. The majority of the work has been performed in the pediatric cardiothoracic surgery population (13,15,16,19-22). There are a couple of potential reasons why this may be the case. First, compared to the overall population of individuals working in the OR and ICU of a pediatric hospital (i.e., all of the surgeons, anesthesiologists, OR and ICU nurses, and pediatric intensivists working in the hospital), there are a relatively smaller number of individuals focused on pediatric cardiothoracic surgery. Establishing consensus and getting buy-in is much easier when there are a smaller number of stakeholders involved. Second, and for similar reasons, one of the foundational principles for quality improvement is to start with small, limited tests of a change using Plan-Do-Study-Act cycles (23). Starting with a well-defined, standardized population such as children undergoing cardiothoracic surgery makes intuitive sense in this respect. For example, an organization-wide quality improvement initiative was launched at Cincinnati Children’s Hospital Medical Center with the global aim of improving communication and safety during OR to ICU hand-offs. The team came up with a key driver diagram (Figure 1) and initially conducted PDSA’s in the cardiothoracic surgery population. After developing a standardized hand-off process with a script and checklist, improvements were spread by design to the other surgical teams and ICU’s (Figures 2-4). The team used a scoring sheet in order to assess the quality of the hand-off that was completed by the bedside nurse during all phases of the initiative (Figure 5). The collective experience (13,15,16,19-22), including the experience at Cincinnati Children’s Hospital Medical Center demonstrates that efforts directed at improving the OR to ICU hand-off improve communication and reduce errors.
Conclusions
The OR to ICU hand-off is a particularly dangerous time for critically ill children. Hand-offs of care between the OR and ICU teams during this key transition period require detailed communication of complete and accurate patient information at a time when the patient is perhaps most vulnerable from a physiologic standpoint. While hand-offs, particularly OR to ICU hand-offs remain an active area of inquiry, there are a few notable best practices that seems to be utilized in a number of centers. These best practices include having the appropriate personnel at the bedside for the hand-off, the use of scripts and the “sterile cockpit rule,” the use of checklists, double verification of post-operative orders, and maintaining an overall safety culture.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kohn LT, Corrigan JM, Donaldson MS. editors. To Err is Human: Building a Safer Health System. Washington DC: National Academy Press, 1999.
- Reid PP, Compton WD, Grossman JH, et al. editors. Crossing the Quality Chasm: A New Health System for the Twenty-first Century. Washington DC: National Academy Press, 2005.
- Rothschild JM, Landrigan CP, Cronin JW, et al. The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med 2005;33:1694-700. [Crossref] [PubMed]
- McElroy LM, Macapagal KR, Collins KM, et al. Clinician perceptions of operating room to intensive care unit handoffs and implications for patient safety: A qualitative study. Am J Surg 2015;210:629-35. [Crossref] [PubMed]
- Gawande AA, Zinner MJ, Studdert DM, et al. Analysis of errors reported by surgeons at three teaching hospitals. Surgery 2003;133:614-21. [Crossref] [PubMed]
- Greenberg CC, Regenbogen SE, Studdert DM, et al. Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg 2007;204:533-40. [Crossref] [PubMed]
- Mazzocco K, Pettiti DB, Fong KT, et al. Surgical team behaviors and patient outcomes. Am J Surg 2009;197:678-85. [Crossref] [PubMed]
- Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and attending physicians’ handoffs: A systematic review of the literature. Acad Med 2009;84:1775-87. [Crossref] [PubMed]
- McElroy LM, Collins KM, Koller FL, et al. Operating room to intensive care unit handoffs and the risks of patient harm. Surgery 2015;158:588-94. [Crossref] [PubMed]
- Segall N, Bonifacio AS, Barbeito A, et al. Operating room-to-ICU patient handover: A multidisciplinary human-centered design approach. Jt Comm J Qual Patient Saf 2016;42:400-14. [Crossref] [PubMed]
- Mukhopadhyay D, Wiggins-Dohlvik KC. Implementation of a standardized handoff protocol for post-operative admissions to the surgical intensive care unit. Am J Surg 2018;215:28-36. [Crossref] [PubMed]
- Sorokin R, Riggio JM, Hwang C. Attitudes about patient safety: A survey of physicians-in-training. Am J Med Qual 2005;20:70-7. [Crossref] [PubMed]
- Thiagarajan RR, Bird GL, Harrington K, et al. Improving safety for children with cardiac disease. Cardiol Young 2007;17:127-32. [Crossref] [PubMed]
- Patterson ES, Roth EM, Woods DD, et al. Handoff strategies in settings with high consequences for failure: Lessons for health care operations. Int J Qual Health Care 2004;16:125-32. [Crossref] [PubMed]
- Catchpole K, Sellers R, Goldman A, et al. Patient handovers within the hospital: Translating knowledge from motor racing to healthcare. Qual Saf Health Care 2010;19:318-22. [Crossref] [PubMed]
- Catchpole KR, De Leval MR, McEwan A, et al. Patient handover from surgery to intensive care: Using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth 2007;17:470-8. [Crossref] [PubMed]
- Gleicher Y, Mosko JD, McGhee I. Improving cardiac operating room to intensive care unit handover using a standardised handover process. BMJ Open Qual 2017;6. [Crossref] [PubMed]
- Rosinski DJ. Sterile cockpit or not: It’s all about team and effective communication. J Thorac Cardiovasc Surg 2010;140:10-1. [Crossref] [PubMed]
- Joy BF, Elliot E, Hardy C, et al. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med 2011;12:304-8. [Crossref] [PubMed]
- Agarwal HS, Saville BR, Slayton JM, et al. Standardized postoperative handover process improves outcomes in the intensive care unit: A model for operational sustainability and improved team performance. Crit Care Med 2012;40:2109-15. [Crossref] [PubMed]
- Zavalkoff SR, Razack SI, Lavoie J, et al. Handover after pediatric heart surgery: A simple tool improves information exchange. Pediatr Crit Care Med 2011;12:309-13. [Crossref] [PubMed]
- Craig R, Moxey L, Young D, et al. Strengthening handover communication in pediatric cardiac intensive care. Paediatr Anaesth 2012;22:393-9. [Crossref] [PubMed]
- Niedner MF. Pediatric quality improvement: Practical and scholarly considerations. Pediatr Clin North Am 2016;63:341-56. [Crossref] [PubMed]