Evaluation and management of shoulder pain in skeletally immature athletes
Introduction
Chronic, intermittent or recurrent shoulder pain in young athletes is a common concern for which athletes seek medical attention. Such pain has been more prevalent in sports that involve repetitive and excessive overhead movements of the shoulder joint complex. These include baseball, cricket, volleyball, swimming, gymnastics and racquet sports. Intrinsic causes of shoulder pain are listed in Table 1 (1-11). Selected and significant conditions that cause shoulder pain in young athletes are reviewed here.
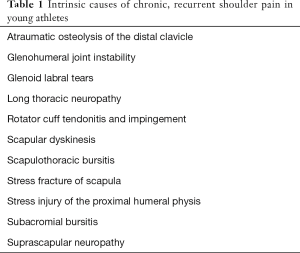
Full table
Proximal humerus physeal stress injury
The head of the humerus develops from 2 ossification centers that fuse into one at 7 years of age (1). The proximal physis of the humerus closes between 19 years and 22 years of age; most fuse by 17 years of age (1). Epiphysiolysis of the proximal humerus occurs primarily in young baseball players; however, has also been reported in cricket (fast bowlers), volleyball, swimming, gymnastics, and racquet sports (1,2). The proximal humeral physis accounts for 80% of the longitudinal growth of the humerus. In sports involving overhead throwing, the physis is subjected to significant amount of stress, resulting in repetitive microtrauma that leads to injury of the unossified cartilage, throwing related pain, and characteristic changes seen on radiographs (2,10,11). It is unclear whether the underlying changes represent inflammation due to overuse or stress fracture through the physis. The mechanism is believed to be repetitive, high intensity, rotational stress to the physis during throwing and other overhead activities (1,2,12-14).
This injury pattern is most common during rapid growth, and occurs most often in adolescent boys, between the ages of 11 years and 16 years, with a peak at 14 years (1). In baseball pitchers, throwing a curve ball and higher pitch counts have been shown to be associated with a higher rate of stress injury to the proximal humeral physis (14). Most throwers demonstrate excessive external rotation at shoulder, whereas the internal rotation is relatively restricted, accompanied by acquired contracture of the posterior capsule, a maladaptation referred to as the glenohumeral internal rotation deficit (1,2,14).
Clinical presentation
The athlete typically presents with gradual onset of shoulder or proximal arm pain associated with throwing. The average duration of symptoms ranges from 7 to 8 months (1,3,8). Often the symptoms are mild lasting for several weeks to months. Because of the pressure to continue to play, athletes often delay seeking medical help. Tenderness over the lateral aspect of the proximal humerus is the most common finding on examination, and may be present in almost 70% of athletes (2-4). Some athletes may have weakness of external rotators of shoulder. Usually the active and passive range of motions of shoulder are normal, until later in the course, when a relative decrease of internal rotation develops (2).
The radiographic findings are characteristic and seen in almost all athletes at the time of presentation. Radiographs with shoulder in external and internal rotation, as well as antero-posterior (AP) and lateral views should be obtained. Comparison views of the opposite shoulder should also be obtained. The classic finding is a widening of the proximal physis, which may or may not be associated with fragmentation, calcification, sclerosis, and demineralization (4,8).
Management
Treatment of proximal humeral physeal stress injury is rest, modification of throwing patterns, and appropriate training and conditioning (3,8,10,15,16). Gradual progression to athletic activities is allowed after symptoms abate. The best treatment is advice and counseling to the parents, the child and the coach to avoid overuse injury in the future. Most of these young athletes will on an average undergo 6 weeks of rest from throwing (15,16). Once pain free, the athlete then undergoes an interval throwing program and return to competition 3–4 months after the injury (12,15,16). All players should be instructed on appropriate limitations on the number and types of pitches, practices and games they may play in (Table 2) (5-10). Current US Baseball Medical and Safety Committee recommendations are summarized in Table 3. Similar treatment principles of rest, activity limitations, and training and conditioning are applied for treatment of players participating in other sports who present with proximal physeal injury.
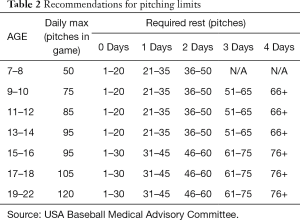
Full table

Full table
Proximal humeral osteochondrosis
Proximal humeral osteochondrosis is a rare problem in children of unknown etiology, exacerbated by overuse in a throwing athlete with a genetic predisposition (5,7,10). These athletes will present similarly to stress injury of the proximal humeral physis. Imaging studies reveal fragmentation of the proximal humeral epiphysis. Treatment of nondisplaced fragments is rest and a reduction of stresses about the shoulder. Throwers should refrain from throwing until completely asymptomatic, and then should undergo appropriate conditioning before return to full time play.
Shoulder impingement syndrome
The rotator cuff muscles (supraspinatus, infraspinatus, teres minor, subscapularis) are predominantly involved in the pathophysiology of this syndrome, hence the condition is also referred to as rotator cuff impingement syndrome (1,3). External (anterior) impingement refers to a lesion of the supraspinatus tendon due to its impingement under the undersurface of the acromion; whereas internal (posterior) impingement refers to a lesion of the glenoid labrum—specifically superior labrum anterior-posterior or superior labrum anterior-posterior (SLAP) lesion due to impingement of the articular surface of the rotator cuff (5-7,17). Shoulder impingement syndrome is a common cause of shoulder pain in swimmers (swimmer’s shoulder), tennis players, gymnasts, and most overhead throwing sports.
The rotator cuff muscles help stabilizing the head of the humerus in the glenoid. The rotator cuff muscles along with the long head of biceps prevent the head of the humerus from moving upward when the arm is abducted. Impingement occurs when the tendons of long head of biceps and supraspinatus, the subacromial bursa, and the greater tuberosity pass underneath the coraco-acromial arch, when the arm is abducted, elevated or externally rotated (1,2). Gleno-humeral instability, tendon overload, muscle weakness, and strength imbalance mainly contribute to impingement in young athletes (2,4). Repetitive overuse in overhead activities as seen in pitchers, swimmers, and tennis players, can lead to chronic inflammation and micro trauma of the rotator cuff tendons leading to edema and swelling, which will compromise the subacromial space (2). On the other hand, in weight lifters and gymnasts the mechanism seems to be sustained isometric muscle contractions leading to tendon overload (2). Either way with continued activity, a vicious cycle of impingement, edema and swelling, and further impingement sets in. The natural course of untreated condition has been described as a continuum progressing from acute inflammation and swelling (stage I), to chronic inflammation, scarring, and tendinitis (stage II), eventually leading to rotator cuff tear (stage III) (2,3,5,7,17). Other factors believed to contribute to the development of impingement, especially in older age group, are decreased vascularity, degeneration, and calcification of the rotator cuff tendons (5).
Swimmers and other overhead athletes will often have significantly weak scapular stabilizer muscles as well, and many will demonstrate scapular winging on exam, with a weak serratus anterior and other periscapular muscles, as well as poor overall coordination of the periscapular muscle groups.
Clinical presentation
The athlete presents with progressively worsening, insidious onset shoulder pain of several days or weeks duration, exacerbated with activity. Some athletes will have discomfort at rest as well as nocturnal pain, especially when associated with glenohumeral instability. The pain is usually diffuse in most athletes, described as deep in the shoulder; however, sometimes it is noted predominantly superolaterally or posteriorly. The pain is exaggerated by overhead movements of the arm. Pain is felt specifically upon abduction between 70 and 120 degrees (2,5). The athlete notices that his or her performance has deteriorated. Pain associated with shoulder impingement syndrome is often described in three stages (2,5,6,10). Stage I is described as stiffness with pain occurring during aggravating movements. In baseball players, this is during the late cocking and early acceleration movements of throwing. Stage II is described as significant posterior joint line pain with athletic movement. Stage III is described as a lack of noticeable improvement following conservative treatment.
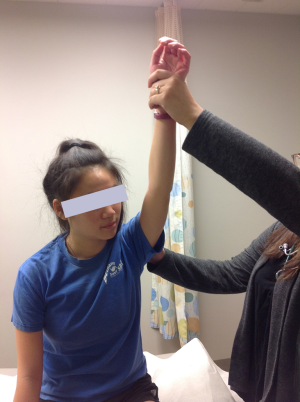
Initially the range of motion is not affected, however, later in the course there may be limitation of abduction and internal rotation. Palpation may reveal tenderness under the acromion process and over the long head of biceps tendon as it traverses the bicipital groove anteriorly if it is also inflamed. Supraspinatus is tested for pain on resisted movement, and for weakness. Resistance is applied to arm abducted to 90 degrees, forward flexed at 30 degrees, and internally rotated (empty can sign) (Figure 1) (5). Pain is also elicited with abduction, internal rotation, flexion of the arm (Figure 2), and forward flexion of the internally rotated arm (Figure 3) (impingement signs) (5). Glenohumeral stability should be assessed by moving the humeral head in anterior, posterior and inferior directions in relation to the glenoid (load and shift test). With anterior instability, pain and discomfort can be elicited when the shoulder is abducted and externally rotated, and improves when the humeral head is moved in a posterior direction (relocation test) (Figure 4). Laxity in other joints should also be assessed, because generalized laxity is not an uncommon finding in adolescents. Pain can be temporarily relieved by injection of xylocaine into the subacromial bursa.



Plain radiographs are normal in most young athletes and magnetic resonance imaging scan is not indicated unless rotator cuff tear, or glenoid labral tear is suspected and surgical intervention is a consideration. Tear of the rotator cuff, especially the supraspinatus, is uncommon in young athletes.
Management
Treatment consists of pain control, modification of activities, and progressive rehabilitation (3,8,10,15,16). Initially, complete rest from offending activities may be necessary for a short period of time. A progressive rehabilitation program will help restore full range of motion, strength, balance, and endurance of the rotator cuff muscles. Rehabilitation is followed by sport specific training and conditioning. Training errors must be identified and corrected. Prognosis for resolution of symptoms and full return to sports is excellent in young athletes, although, it may take several weeks to months before the athlete may return to his or her previous level of participation.
Surgical treatment is rarely a consideration in young athletes. Failure to respond to the conservative treatment should prompt reevaluation and careful consideration of any other underlying cause for the pain. If a cuff or labral tear is suspected orthopedic consultation should be obtained.
Chronic, atraumatic glenohumeral joint instability
Glenohumeral instability refers to excessive motion of the glenohumeral joint associated with relatively greater laxity of the joint stabilizers that result in either acute (traumatic) or chronic (non-traumatic) clinical symptoms and signs (11). The spectrum of instability can range from microinstability to subluxation to dislocation of the glenohumeral joint (18). Although shoulder instability has been described based on the degree, frequency, acuity, etiology, and direction, for practical purposes, it is useful to consider two broad clinical presentations, namely acute traumatic dislocation (anterior, posterior, inferior) and chronic non-traumatic symptomatic instability (anterior, posterior, inferior, and multidirectional). (5,10,18)
The main static stabilizers of the glenohumeral joint are the head of the humerus and the glenoid, the glenohumeral ligaments, and the glenoid labrum, whereas the main dynamic stabilizers are the rotator cuff muscles. The major mechanisms underlying the chronic atraumatic shoulder instability involve repetitive and excessive motions of the shoulder complex. These include overhead arm and shoulder movements such as seen in throwing sports, swimming, volleyball or tennis.
Clinical presentation
Multidirectional instability is a common problem, particularly in young female athletes, and can be one cause of rotator cuff tendonitis. Psychological factors should be explored in the history. Most athletes with atraumatic instability are asymptomatic. The athlete with symptomatic instability will present with shoulder pain associated with overhead movements, a sense of weakness, and deterioration in sport performance. There may be a positive family history of the shoulder laxity.
On examination, the shoulder often will be unstable in several planes, with the athlete able to demonstrate multiple lax joints. On load and shift test, the athlete will demonstrate relatively greater than normal motion of the humeral head anteriorly and posteriorly on the glenoid. The most accurate way to assess this is to have the athlete supine, with the arm in neutral rotation and grasp the proximal humerus, translating it anteriorly on the glenoid.
The sulcus sign is also positive with inferior instability. In a normal shoulder this may be present as well but usually will disappear with the arm in external rotation which will tighten the rotator interval and eliminate the sulcus sign. Athletes with multidirectional instability often can and will spontaneously and voluntarily subluxate or dislocate their shoulder(s). Athletes presenting with glenohumeral instability should be evaluated for generalized joint and ligamentous hyperlaxity. There is often associated capsular laxity and shoulder instability demonstrated in the asymptomatic shoulder as well. Laxity of the shoulder does not always correlate with symptoms.
Management
Athletes with symptomatic atraumatic instability must undergo a prolonged course of monitored comprehensive rehabilitation, followed by long term home physical therapy for up to a year or more (3,5,9,10,18). Most athletes are not candidates for any surgical reconstruction or intervention, unless they prove to have a labral tear or other similar problems such as a significant capsular injury or they have failed non-operative treatment. It takes a great deal of patience on the part of the young athlete, the family and the surgeon to allow prolonged course of rehabilitation therapy to work.
Disorders of long head of biceps brachii
The long head of the biceps brachii muscle can be injured or inflamed resulting in pain or dysfunction. Disorders of the long head are uncommon in adolescent athletes but have been reported with acute trauma or repetitive overhead activities (19). The tendon originates from the post-erosuperior labrum and the supraglenoid tubercle in the glenohumeral joint (20). It traverses out of the joint encased within the synovial sheath of the joint. It occupies the bicipital groove and is mainly restrained in position during shoulder movements by the surrounding soft tissue (20). The biceps brachii traverses both the shoulder and the elbow joints. It acts as a flexor and supinator of the elbow joint, but its role in shoulder movements has not been clearly elucidated (20). Biceps tendonitis may occur generally associated with rotator cuff tendonitis. Acute trauma is associated with glenoid labral injuries. The tendon may also subluxate or dislocate from the bicipital groove.
In case of acute rupture or dislocation, the athlete will present with acute pain, localized tenderness and soft tissue swelling. Injury can occur during activities such as throwing or heavy weight lifting. Biceps tendonitis is generally associated with rotator cuff tendonitis and impingement sings. The pain is exacerbated with arm in abduction, extension and internal rotation. There will be localized tenderness over the bicipital groove and the Speed test (Figure 5) may be positive. Evaluation of the tendon can be done with ultrasound or MRI scan if indicated.

Acute or chronic inflammation is treated with rest, ice, and NSAIDs. Rupture generally do not affect function and is treated conservatively with rehabilitation exercises. Surgical treatment has been reported for dislocating tendon.
Atraumatic osteolysis of the distal clavicle (AODC)
AODC is characterized by chronic changes seen in the lateral end of the clavicle. It is seen most commonly in those engaged in body building and competitive weight lifting (21). Less commonly such lesions have been reported in athletes involved in basketball, volleyball, swimming, football, and baseball pitchers (21). Most cases occur in males, but the condition has been described in females. Athletes participating in sports that require overhead activity as well as supplemental weight training are at a higher risk. AODC is believed to be due to repetitive excess load and associated microtrauma to the distal end of the clavicle (21).
The pain is of gradual onset, dull aching, unilateral or bilateral, over distal clavicle and acromioclavicular area, experienced soon after exercise. Pain is elicited or exacerbated by adduction of the arm across the chest at horizontal flexion at 90 degrees. There may be localized tenderness over the acromioclavicular joint area. The diagnostic features on plain films include microcysts, loss of subchondral bone detail, and osteolysis of distal clavicle. An increased uptake on Technetium-99-m labeled phosphate scintigraphy is considered diagnostic by some experts. MRI scan demonstrate distal clavicular edema often with subchondral fracture and/or subchondral cystic change.
The athlete must make the difficult and often personally unacceptable choice to give up weight lifting or other inciting activity. In some cases, a modification of weight lifting technique or training regimen can alleviate symptoms. In most cases, surgical resection of distal clavicle has been shown to be quite effective.
Neuropathies around shoulder
Long thoracic nerve neuropathy
Compression or direct injury of the long thoracic nerve can result in serratus anterior paralysis. Long thoracic nerve injury has been reported in many sports including basketball, bowling, discus throwing, football, gymnastics, hockey, tennis, weight lifting, wrestling, and soccer (22).
In sports, long thoracic neuropathy can result from direct blow or repetitive trauma.
The patient may present with diminished forward elevation of the shoulder, pain in the posterior shoulder and the trapezius, with apparent winging or winging with attempted wall pushups or similar exercises (22). There also is often spasm of the trapezius and trigger point pain over the posterior superior scapula related to overuse of the trapezius muscle in an attempt to stabilize the scapula and elevate the shoulder. Electromyography and nerve conduction studies are diagnostic.
Many younger and adult athletes will regain full shoulder function after several weeks of scapular muscle and rotator cuff closed chain exercises and focused rehabilitation (22). Others will benefit from a longer term physical therapy, some up to 2 years for full recovery (22).
Suprascapular nerve neuropathy
Compression or direct blow to the suprascapular nerve can result in partial or complete paralysis of either infraspinatus and/or supraspinatus muscles (23,24). Suprascapular neuropathy has been reported in throwing sports, volleyball, tennis, weight lifting, and swimming (24). Repetitive trauma, direct blow, traction, or compression can result in suprascapular neuropathy in athletes. Suprascapular nerve compression is commonly associated with backpack straps or other straps or protective devices which place pressure on the nerve as it exits above the scapula through the suprascapular notch (23). Compression of the nerve can also result from a ganglion or cyst.
The compression may cause infraspinatus and supraspinatus muscle atrophy and weakness, and insidious onset of dull, sometimes burning shoulder pain, limited range of motion and overall shoulder dysfunction (23). There is weakness of external rotation and abduction of the shoulder. Asymptomatic muscle wasting may be the only initial presentation. EMG and nerve conduction studies are diagnostic. MRI scan may be indicated to evaluate the specific cause of compression such as a ganglion or a cyst in some cases.
A compression or traction injury often will resolve with cessation of the irritating factor, such as discontinuing use of a backpack for several weeks (23,24). Injuries which are persistent may require an arthroscopic or open release of the suprascapular nerve, which is effective in relieving pain, and may allow return of muscle mass and strength depending upon the length of time the injury has been present (23,24). The athlete may also present with primarily pain in the suprascapular region, with EMG showing delayed conduction in the suprascapular nerve, but not necessarily demonstrate any muscle wasting (24). These cases usually will require open or arthroscopic release of the ligament which is compressing the nerve in the suprascapular notch. Patients with suprascapular neuropathy have good prognosis for resuming normal activity without pain at the end of either conservative or surgical treatment (23,24).
Acknowledgements
Authors thank Anna, Skye and Allison for their help with the manuscript preparation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: Adapted with permission from: Patel DR, Lyne ED. Overuse injuries of shoulder. In: Patel DR, Greydanus DE, Baker RJ, editors. Pediatric Practice: Sports Medicine. NY: McGraw Hill, 2009:245-57.
References
- Hutchinson MR, Ireland ML. Overuse and throwing injuries in the skeletally immature athlete. Instr Course Lect 2003;52:25-36. [PubMed]
- Meister K. Injuries to the shoulder in the throwing athlete. Part one: Biomechanics/pathophysiology/classification of injury. Am J Sports Med 2000;28:265-75. [PubMed]
- Meister K. Injuries to the shoulder in the throwing athlete. Part two: evaluation/treatment. Am J Sports Med 2000;28:587-601. [PubMed]
- Altcheck DW, Levinson M. The painful shoulder in the throwing athlete. Orthop Clin North Am 2000;31:241-5. [Crossref] [PubMed]
- Ryu RK, Dunbar WH 5th, Kuhn JE, et al. Comprehensive evaluation and treatment of the shoulder in the throwing athlete. Arthroscopy 2002;18:70-89. [Crossref] [PubMed]
- Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc 2001;33:1803-10. [Crossref] [PubMed]
- Sciascia A, Kibler WB. The pediatric overhead athlete: what is the real problem? Clin J Sport Med 2006;16:471-7. [Crossref] [PubMed]
- Paz DA, Chang GH, Yetto JM Jr, et al. Upper extremity overuse injuries in pediatric athletes: clinical presentation, imaging findings, and treatment. Clin Imaging 2015;39:954-64. [Crossref] [PubMed]
- Smucny M, Kolmodin J, Saluan P. Shoulder and Elbow Injuries in the Adolescent Athlete. Sports Med Arthrosc 2016;24:188-94. [Crossref] [PubMed]
- Tisano BK, Estes AR. Overuse Injuries of the Pediatric and Adolescent Throwing Athlete. Med Sci Sports Exerc 2016;48:1898-905. [Crossref] [PubMed]
- Shanley E, Thigpen C. Throwing injuries in the adolescent athlete. Int J Sports Phys Ther 2013;8:630-40. [PubMed]
- Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med 2002;30:463-8. [PubMed]
- Popchak A, Burnett T, Weber N, et al. Factors related to injury in youth and adolescent baseball pitching, with an eye toward prevention. Am J Phys Med Rehabil 2015;94:395-409. [Crossref] [PubMed]
- Rauck RC, LaMont LE, Doyle SM. Pediatric upper extremity stress injuries. Curr Opin Pediatr 2013;25:40-5. [Crossref] [PubMed]
- Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med 2002;30:136-51. [PubMed]
- McFarland EG, Ireland ML. Rehabilitation programs and prevention strategies in adolescent throwing athletes. Instr Course Lect 2003;52:37-42. [PubMed]
- Fessa CK, Peduto A, Linklater J, et al. Posterosuperior glenoid internal impingement of the shoulder in the overhead athlete: pathogenesis, clinical features and MR imaging findings. J Med Imaging Radiat Oncol 2015;59:182-7. [Crossref] [PubMed]
- Walton J, Paxinos A, Tzannes A, et al. The unstable shoulder in the adolescent athlete. Am J Sports Med 2002;30:758-67. [PubMed]
- Wiseman SP, Beran MC, Warahadpande S, et al. Rupture of the Long Head of the Biceps Tendon in a Pediatric Athlete. JBJS Case Connect 2016;6:e33. [Crossref]
- Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg 1999;8:644-54. [Crossref] [PubMed]
- Roedl JB, Nevalainen M, Gonzalez FM, et al. Frequency, imaging findings, risk factors, and long-term sequelae of distal clavicular osteolysis in young patients. Skeletal Radiol 2015;44:659-66. [Crossref] [PubMed]
- Safran MR. Nerve injury about the shoulder in athletes, part 2: long thoracic nerve, spinal accessory nerve, burners/stingers, thoracic outlet syndrome. Am J Sports Med 2004;32:1063-76. [Crossref] [PubMed]
- Safran MR. Nerve injury about the shoulder in athletes, part 1: suprascapular nerve and axillary nerve. Am J Sports Med 2004;32:803-19. [Crossref] [PubMed]
- Hill LJ, Jelsing EJ, Terry MJ, et al. Evaluation, treatment, and outcomes of suprascapular neuropathy: a 5-year review. PM R 2014;6:774-80. [Crossref] [PubMed]


