Kickboxing power hour: case report of fifth metatarsal apophysitis (Iselin disease) and its magnetic resonance imaging features
Introduction
Iselin disease is traction apophysitis of the fifth metatarsal base and clinically presents with tenderness and pain overlying the lateral aspect of the midfoot. First described in 1912 by H. Iselin, a German physician (1), this disease entity is often underdiagnosed mostly due to lack of familiarity with the diagnosis. Differential diagnoses for lateral midfoot pain include Jones fracture, avulsion fracture and diaphyseal stress fracture. Iselin disease is treated conservatively and thus it is important to distinguish this condition from fractures that may require cast and/or internal fixation.
Case presentation
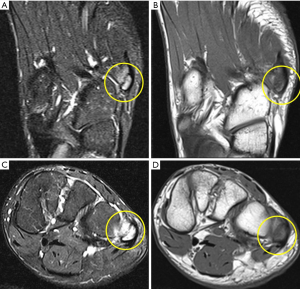
A 15-year-old boy presented with complaints of a painful lump on the lateral left foot for a few weeks. The patient denied prior history of trauma or significant medical history. The patient reported progressive worsening of pain since the onset of the symptoms. The patient was actively involved in mixed martial arts (kickboxing) and was an active runner for a past few months. The patient reported aggravation of pain during running and during his kickboxing practice sessions especially while performing sidekicks or round kicks. On physical examination, there was point tenderness and minimal swelling at the base of the fifth metatarsal. No associated ecchymosis was seen. The clinical concern at the time of presentation was a fracture at the base of the fifth metatarsal or tendinopathy. Radiographic images showed normal appearance of the fifth metatarsal apophysis, with no fracture (Figure 1). MRI of the foot demonstrated severe bone marrow edema in the unfused apophysis and mild to moderate bone marrow edema in the adjacent base of fifth metatarsal, consistent with apophysitis (Figure 2). Additionally there was bone marrow edema seen within the second and third metatarsal, which is a typical location for stress reaction. No associated ligament or tendon injuries were identified. The patient was treated conservatively with rest and nonsteroidal anti-inflammatory drugs, with resolution of pain after 1 month.

Discussion
Iselin disease is classified as osteochondrosis in growing children and has been widely accepted as an overuse injury (2-5). This pathologic entity is most common in children/young adults who are actively involved in sports activity, particularly running, jumping or dancing. The proposed mechanism of apophyseal injury is repeated traction by peroneus brevis tendon which inserts at the fifth metatarsal base. A typical presenting symptom is lateral midfoot pain exacerbated by physical activities. The patient may report difficulty in wearing shoes. On physical exam, there is tenderness overlying the fifth metatarsal base. Localized swelling may also be noted. Radiographic imaging in Iselin disease demonstrates apophyseal fragmentation and irregularity. Radiographs may be negative early in the course of the disease, as in our case. The magnetic resonance imaging (MRI) features of Iselin disease include bone marrow edema within the fifth metatarsal base apophysis, widening of physis and muscle edema. Adjacent muscle edema is a non-specific finding which can be seen in association with any process causing myo-tendinous strain (6). Additionally it is of utmost importance to look for additional stress related injuries in these patients including addition metatarsal stress fractures, as seen in our patient. MRI findings precede the radiographic epiphyseal fragmentation and are thus useful in early detection of the disease (1). Early initiation of anti-inflammatory medications shortens the disease course.
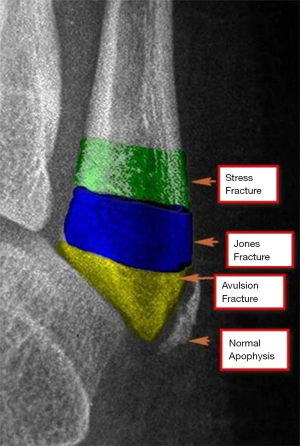
The differential diagnoses of lateral foot pain in the pediatric population include avulsion fracture of the fifth metatarsal base, Jones fracture, diaphyseal stress fracture as well as os vesalianum pedis (Table 1). Lack of history of prior trauma and crepitus on physical exam also favor apophysitis over a fracture. The apophysis of the fifth metatarsal base on radiograph appears at 10 years in girls and 12 years in boy (7). The fusion usually occurs over the following 2–4 years (3,4). Normal apophysis on radiograph is always oriented parallel to the longitudinal axis of the fifth metatarsal and does not extend proximally into the joint; however the fracture does show intra-articular extension (Figure 3). The orientation of the fracture is transverse as opposed to normal growth plate. An avulsion fracture occurs through the tip of the proximal fifth metatarsal and can occasionally reach the articular surface (metatarsocuboid). A Jones fracture extends through the metadiaphyseal junction and is often more distal to the avulsion fracture. Diaphyseal stress fractures typically occur within 1.5 cm of the metadiaphyseal junction, slightly distal to the site of a Jones fracture (Figure 3). Os vesalianum pedis is an accessory bone located adjacent to the fifth metatarsal base, embedded in the peroneus brevis tendon. Os vesalianum pedis appears as a well-corticated ossicle that articulates with adjacent cuboid on radiograph, which is usually detected incidentally but may sometime be a source of pain (8).

Full table
Iselin disease is treated conservatively with rest and nonsteroidal anti-inflammatory drugs. Pain usually resolves within 3–4 weeks. In addition, it is important to educate the parents and child with the mechanism of injury and to avoid over indulging in activities causing the symptoms.
In conclusion, Iselin disease should be suspected in children and adolescent patients of 10–15 years age who are involved in physical activities such as running and kickboxing and presenting with lateral foot pain. Careful physical examination and radiographic evaluation is helpful in differentiating other causes of lateral foot pain in this age group. MRI is extremely useful in early diagnosis and initiation of appropriate treatment. It is vital to correctly diagnose this disease entity and to avoid misdiagnosis of a fracture.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient’s parent for publication of this manuscript and any accompanying images.
References
- Deniz G, Kose O, Guneri B, et al. Traction apophysitis of the fifth metatarsal base in a child: Iselin’s disease. BMJ Case Rep 2014;2014. pii: bcr2014204687.
- Ralph BG, Barrett J, Kenyhercz C, et al. Iselin’s disease: a case presentation of nonunion and review of the differential diagnosis. J Foot Ankle Surg 1999;38:409-16. [Crossref] [PubMed]
- Canale ST, Williams KD. Iselin's disease. J Pediatr Orthop 1992;12:90-3. [Crossref] [PubMed]
- Lehman RC, Gregg JR, Torg E. Iselin's disease. Am J Sports Med 1986;14:494-6. [Crossref] [PubMed]
- Schwartz B, Jay RM, Schoenhaus HD. Apophysitis of the fifth metatarsal base. Iselin's disease. J Am Podiatr Med Assoc 1991;81:128-30. [Crossref] [PubMed]
- Kumar Y, Wadhwa V, Phillips L, et al. MR imaging of skeletal muscle signal alterations: Systematic approach to evaluation. Eur J Radiol 2016;85:922-35. [Crossref] [PubMed]
- Sanal HT, Chen L. Lateral Foot Pain. Skeletal Radiol 2015;44:1687-8. [Crossref] [PubMed]
- Köse Ö. The accessory ossicles of the foot and ankle; a diagnostic pitfall in emergency department in context of foot and ankle trauma. JAEM 2012;11:106-14. [Crossref]


