Under 5 mortality rate and its contributors in Zhejiang Province of China from 2000 to 2009
Childhood mortality is a prominent public health issue. Reducing childhood mortality (mortality before the age of five) is the fourth goal of the Millennium Development Goals agreed at the United Nations Millennium Summit in September 2000 (1). Globally, mortality in under-five age children is about 9 million deaths per year and 70% are preventable which makes this an important public health problem to investigate (2). While childhood mortality in developing countries remains higher: it has been estimated that about 10.8 million children die each year (1,3-5). However, the mortality of children under five years of age has decreased worldwide from 10.8 million deaths per year in 2000 to 8.8 million deaths in 2008 (6).
The first 4-week of life - the neonatal period - carries one of the highest risks of death of any 4-week period in the human lifespan (7). In high-income countries, neonates are now a major focus of child health both for mortality and morbidity reduction (8). Compared with the most advanced urban or developed coastal areas in China, neonatal mortality rates (NMR) in remote and poor rural areas is unacceptably high and shows remarkable disparities between the rural areas and urban areas (9). Therefore, the under 5 mortality rate (U5MR) is recognized and used as a robust indicator of children’s health in a country, and also a key basis for government authorities to improve and expand their programs, plans, and policies on maternal and children health care (10). Currently, studies on U5MR in China are mainly focused on the figures, trends, and rank of causes of death, while studies with continuity, large sample, and multiple perspectives are still lacking.
The purpose of the study was to assess the mortality rates for children of all ages and the leading causes of death among infant and children, as well as comparison of U5MR between the floating population and local residents and between rural areas and urban areas, in children under 5 years. In this article, by analyzing the U5MR and its contributors in Zhejiang Province of China from 2000 to 2009, we tried to understand the trend of U5MR change in Zhejiang Province and thus propose strategies to improve child survival.
Subjects and methods
Subjects
In this stratified cluster sampling design, 1-3 cities/counties/districts were randomly selected from the 11 administrative regions of Zhejiang Province based on their locations and socioeconomic levels. Totally 30 cities/counties/districts were selected, with a sample coverage rate of 100%. The subjects were all children under five years who met the following criteria: had a gestational age of 28 weeks; exhibited any sign of life (i.e., heartbeat, breath activity, funic pulse, and contraction of voluntary muscle); and died.
Data collection
A three-tier death reporting network (street-district-city in urban areas and village-town-county in rural areas, with maternal and child health care institution as the core organization) and its corresponding monitoring system was established. Dedicated personnel is assigned at each tier to collect, review and transfer the data, which were finally summarized and analyzed by the provincial maternal and child health care institutions.
Quality control
A tier-wise quality inspection system was established: the maternal and child health care institutions at the county level were responsible for the collection, verification, and tracing of the data and those at the county and city levels carried out quality control activities every six months. Furthermore, a province-level quality control expert group, comprised of clinicians and public health experts, was established in the maternal and child health care institutions at the province level; the expert group carried out supervision and quality control activities in some randomly sampled areas annually and adjusted the data using the quality control results.
Statistical analysis
A database was established using Microsoft Excel software. All data were analyzed using the SPSS 13.0 software. Rates were compared using Chi square test. P<0.05 was considered significantly different.
Results
U5MR in Zhejiang Province from 2000 to 2009
Totally 819,538 children died in the sampled areas from 2000 to 2009, among whom 7,602 (9.28‰) were children under 5 years old, among which 5,637 were infants (74.15%). In 2009, the population number in the sampled areas accounted for 34.9% of the total population of Zhejiang Province. Also in 2009, the U5MR and infant mortality rate were 9.49‰ and 6.73‰, respectively, reaching historic low levels. The U5MR showed a declining trend from 14.83‰ in 2000 to 9.49‰ in 2009 (Figure 1), while the infant mortality rate declined from 11.61‰ in 2000 to 6.73‰ in 2009.
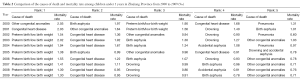
Chi square test showed that the mortality rates for children of all ages were significantly higher in the floating population than in local residents and in rural areas than in urban areas (all P<0.05) (Table 1).

Full table
Comparison of the causes of death and mortality rates among children under 5 years in Zhejiang Province
Comparison of the causes of death among children under 5 years from 2000 to 2009
The leading causes of death among children under 5 years remarkably changed since 2000. The mortality rates of congenital anomaly, birth asphyxia, and pneumonia have dramatically fallen: “other congenital anomalies” was the first leading cause of death in 2000, but fell to the 5th in 2009, with a mortality rate declined from 2.05‰ to 0.71‰. The “other congenital anomalies” refers to birth deformities such cheilopalatognathus, anal atresia, limb deformities, and esophageal atresia except congenital heart disease (CHD), Down’s syndrome, and deformity of neural tube. Although the mortality rates of preterm birth/low birth weight and CHD have somehow declined, they became the first and second leading causes of death in 2009 (Table 2).
Full table
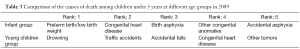
Comparison of the causes of death among children under 5 years at different age groups in 2009
The leading causes of death among infants (younger than 1 year) were preterm birth/low birth weight and congenital anomalies, while that among young children (1-4 years) was mainly due to accidents (Table 3).
Full table
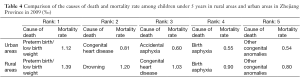
Comparison of the causes of death among children under 5 years with different “migration status of mother” in 2009
The U5MR was significantly higher in rural areas than in urban areas, and the ranks of the death causes were also different (Table 4).
Full table
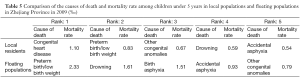
The mortality rate was remarkably low among children from local families than from floating families. Meanwhile, the rank of death causes also showed certain differences: the leading cause of death was CHD among children from local families, while the top three causes of death were preterm birth/low birth weight, drowning, and birth asphyxia for the floating populations (Table 5).
Full table
Discussion
As shown in our survey, the U5MR and infant mortality rate showed declining trends in Zhejiang Province from 2000 to 2009. Although there was a slight rise from 2002 to 2003, the rates gradually fell after 2004 and were kept at certain levels; notably, they remained stable at a relatively low level after 2007. This change may be explained by the fact that Zhejiang Province formally initiated its county-wide monitoring for all populations in 2007, which overcame the relatively wide fluctuation due to small sample size before 2006. Therefore, the mortality rates in recent years can more accurately reflect the real-world situations in Zhejiang Province. Literature review shows that the U5MR in Zhejiang Province was slightly higher than that in Beijing, very close to Guangdong Province, and lower than Heilongjiang, Gansu, Liaoning, and some other provinces (11-15), and therefore is at a comparatively low level nationwide. Although the U5MR has shown a declining trend in Zhejiang Province, it still shows remarkable disparities between the rural areas and urban areas and among children born to families with different “migration status of mothers” (or known as “Hukou” in China). The child mortality rate was still higher in rural/floating children than in urban/local children. Since the overall mortality rate has become relatively low, more efforts should be taken to bridge the gaps in quality of life between urban and rural areas and between floating populations and local residents.
Our survey also showed the leading cause of U5MR in Zhejiang Province has become “preterm birth/low birth weight”, which was “other congenital anomalies” in 2000. CHD, although its mortality rate has dramatically fallen, has become the second largest contributor to the U5MR. Actually, the rise of CHD in the death cause ranking suggests that birth defects including CHD has increasingly became the key risk factors of deaths among children under 5 years. Second, infectious diseases such as pneumonia are not the key contributors to U5MR, while accidents such as accidental asphyxia become increasingly important. In fact, along with the rapid improvement of medical technology and the increase of health care awareness, infectious diseases usually can be timely prevented and efficiently managed and therefore have less important roles in death cause ranking; meanwhile, prevention of “unintentional injuries” and “preterm birth/low birth weight” may further reduce U5MR.
Our survey also found that the death causes differed between infants (<1 years) and young children (1-4 years). The infants were mainly died of “preterm birth/low birth weight” and “congenital anomalies”, while the main death cause of young children were accidents including drowning, traffic accidents, and accidental falls. Therefore, the interventional priority for infants should be focused on the impact of preterm birth/low birth weight on death. Some other relevant studies have shown that “preterm birth/low birth weight” is closely associated with the mother’s age, gestational age-related complications, frequency of antenatal examination, premature rupture of membranes, fetal position, and some other factors (16,17). Therefore, perinatal care, antenatal examination, management of complications, and monitoring of high-risk pregnancies are important to reduce infant mortality rate. For young children aged 1-4 years, the priority will be the prevention of accidental injuries. Unintentional injury has already become the leading cause of death in the developed countries, and most of them are preventable (18,19). The feasible interventions include: urge the parents to take care of their children more carefully and to educate their children to stay far away danger; carry out routine safety lectures; and teach basic first aid knowledge. Meanwhile, a multi-sector strategy participated by the whole society should be established and implemented: the securities in communities, schools, kindergartens, and public places should be strengthened, and the regulations on road and traffic should be strictly implemented, so as to prevent the accidental deaths of children.
Our survey also found that children in rural areas tended to have a higher mortality rate due to “accidental deaths”. Drowning has become the second leading cause of death among rural children, behind only “preterm birth/low birth weight”. This is mainly because the rural children usually live in highly decentralized settings. Therefore, the rural children should be listed in the priority populations; meanwhile, efforts should be made to increase public health investment, establish health care manage system for rural children, and increase the parents’ awareness of preventing the accidental death. Meanwhile, analysis on children with different migration status of the mother showed that the leading death cause of local children was CHD rather than “preterm birth/low birth weight”, while “preterm birth/low birth weight” remained the top cause of death among the children of floating families. The mortality rate was remarkably higher among the floating children than the local children. This may be explained by the socioeconomic factors: the local children are more likely to get access to advanced delivery technique, medical technology, and other supporting resources, while the floating children, especially those preterm infants, have limited access to the medical resources needed. The influence of the “migration status of the mother” on child mortality rate suggests that the mothers in the floating populations should be included in the women health care administration system and treated as the priority population in peri-natal health care. Particularly, efforts should be made to increase their awareness and knowledge of antenatal examination and peri-natal health care, so as to lower the impact of preterm birth/low birth weight on the mortality rate of children from floating families.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Escaramís G, Carrasco JL, Aponte JJ, et al. Spatio-temporal analysis of mortality among children under the age of five in Manhiça (Mozambique) during the period 1997-2005. Int J Health Geogr 2011;10:14. [PubMed]
- Children: reducing mortality. World Health Organization; 2012. Available online: [], Ref Type: Online Source.http://www.who.int/mediacentre/factsheets/fs178/en/
- Victora CG, Wagstaff A, Schellenberg JA, et al. Applying an equity lens to child health and mortality: more of the same is not enough. Lancet 2003;362:233-41. [PubMed]
- Bryce J, Boschi-Pinto C, Shibuya K, et al. WHO estimates of the causes of death in children. Lancet 2005;365:1147-52. [PubMed]
- Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year? Lancet 2003;362:65-71. [PubMed]
- Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010;375:1969-87. [PubMed]
- Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet 2005;365:891-900. [PubMed]
- Shiffman J. Issue attention in global health: the case of newborn survival. Lancet 2010;375:2045-9. [PubMed]
- Yi B, Wu L, Liu H, et al. Rural-urban differences of neonatal mortality in a poorly developed province of China. BMC Public Health 2011;11:477. [PubMed]
- Wang YP, Miao L, Qian YQ, et al. Analysis of under 5 years old children mortality and the leading death cause in China from 1996 to 2000. Zhonghua Yu Fang Yi Xue Za Zhi 2005;39:260-4. [PubMed]
- Xu YH, Huang XW, Yang RL. Analysis on the causes of death for the children under the age of 5 in Beijing from 2003 to 2007. Chinese Journal of Health Statistics 2009;26:396-7.
- Li RH, Zhao QG, Li B. Analysis of under 5 years old children mortality and the death cause in Guangdong Province from 2001 to 2005. International Medicine & Health Guidance News 2006;12:147-8.
- Lu M. Monitoring analysis of children death under 5 years old from 2003-2006 in Heilongjiang Province. Chinese Journal of Reproductive Health 2009;20:102-3.
- Liu H, Guo JX, Pu YD, et al. Analysis on trend of under 5 years old children mortality in Gansu Province from 1996 to 2005. Chinese Primary Health Care 2007;21:45-6.
- Li J. Analysis of under 5 years old children mortality rate in Liaoning Province from 2000 and 2004. Chin J Public Health 2007;23:103.
- Terzic S, Heljic S. Assessing mortality risk in very low birth weight infants. Med Arh 2012;66:76-9. [PubMed]
- Koo YJ, Ryu HM, Yang JH, et al. Pregnancy outcomes according to increasing maternal age. Taiwan J Obstet Gynecol 2012;51:60-5. [PubMed]
- Okoye CN, Okoye MI. Forensic epidemiology of childhood deaths in Nebraska, USA. J Forensic Leg Med 2011;18:366-74. [PubMed]
- Feury KJ. Injury prevention. Where are the resources? Orthop Nurs 2003;22:124-30. [PubMed]



