Surgical approaches for varicocele in pediatric patient
Introduction
Varicocele is an abnormal dilation of pampiniform plexus and internal spermatic veins leading to increased temperature in the seminiferous tubules, reflux of toxic adrenal and renal metabolites through the renal vein, decreased sperm quality and testicular growth arrest (1,2).
With an incidence of approximately 15%, varicocele represents one of the most common surgically correctible urologic anomalies in adolescent males (3). While varicoceles are identified in up to 35% of men with primary infertility (4), approximately 80% of adults with varicoceles are asymptomatic and fertile (5). Therefore, one of the major challenges in management of adolescent varicoceles is determining which patients would benefit most from varicocelectomy and at what age (5). While the indications for surgical intervention in these patients are controversial, many experts advocate varicocele repair in patients with a persistent testicular size discrepancy of greater than 20%, abnormal semen analysis if obtainable, and pain attributable to the varicocele (5).
The ideal surgical approach for adolescent varicocelectomy represents another area of debate. The cornerstone of varicocele treatment is to block the reflux in the internal spermatic vein while preserving the internal spermatic artery, lymphatics and vas deferens. Over the past 50 years, many reports showed an increase in number and motility of sperm in patients with varicocele after surgery (6). Therefore this was an important incentive in improving surgical techniques to find an effective method able to reverse testicular damage.
Currently, the best procedure for the treatment of adolescent varicocele has not been established, but multiple methods exist for the treatment of varicocele, that include an open or laparoscopic abdominal (Palomo) approach, with high ligation of spermatic vascular structures; alternatively, inguinal (Ivanissevich) and subinguinal approaches may be utilized, with or without the use of microsurgical techniques (3,5).
While the subinguinal microsurgical approach appears to have become the gold standard for varicocele ligation in adult males with infertility due to lower postoperative recurrence and complication rates compared to other techniques (4), this approach has not been widely adopted in the adolescent population. With recent advances in minimal access surgery, there have been many reports praising the safety and efficacy of laparoscopy and retroperitoneoscopy for the surgical correction of varicocele in adolescent (7-9).
The aim of this review is to compare the results of Palomo’s technique, with retroperitoneoscopic and transperitoneoscopic approaches in adolescent, analyzing recurrence, testicular growth and complications.
Methods
A literature search on PubMed and Cochrane Database was conducted with regard to management of varicocele in adolescent population.
The following key words were used: “adolescent varicocele”, “surgical treatment of varicocele”, “laparoscopic Palomo”, “retroperitoneoscopic Palomo”.
Twenty two English language studies published in the last years were considered in our study.
Randomized controlled trials comparing outcome of different minimally invasive treatments or comparing outcome of minimally invasive and traditional surgical treatments for adolescent diagnosed with varicocele are included.
Exclusion criteria were about articles that reported outcomes in adulthood, and about studies published before 1990. In particular we have analyzed randomized controlled trial, review article and case series about this pathology.
Surgical technique
Transperitoneoscopic approach
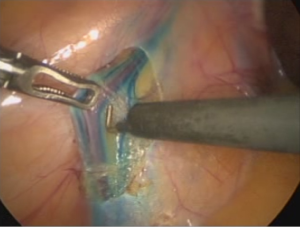
The patient is placed supine on the operating table, and generally a urinary catheter is introduced, which is removed at the end of the procedure. The surgeon stood on the patient’s right side and the assistant opposite the surgeon. Each port side is first infiltrated with bupivacaine 0.25%. First a 10 mm primary port, for 0° operative telescope, is placed at the umbilicus, under direct vision. The peritoneum cavity is insufflated with CO2 until the intra-abdominal pressure is 10–12 mmHg. Two further 5 mm ports are introduced, in the left iliac fossa and the sovrapubic side. Tilting of the table in Trendelenburg and to the right promoted exposure of left-sided varicocele. The internal inguinal ring is identified. Using dissecting shears the peritoneum is incised over testicular vessels a few centimeters above the internal ring. The spermatic vessels are elevated from the posterior pelvic wall, coagulated with bipolar electrocautery and then divided (Figure 1).
Retroperitoneoscopic approach
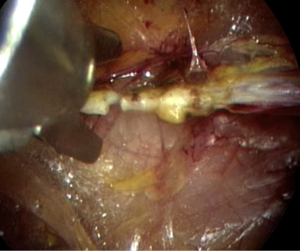
The patient is positioned in a right lateral decubitus position, with a sand bag underneath the lumbar region and a bend in the table at the same level in order to widen the space between the 12th rib and the iliac crest. The surgeon stood behind the patient and the monitor was in front. A 10 mm transverse incision is made between the 12th rib and the iliac crest, after local injection of bupivacaine 0.25%. A muscle-splitting dissection is used to gain access into the retroperitoneal space and a ballooned 10-mm trocar is introduced into the retroperitoneal space under visual control. Carbon dioxide pneumoretroperitoneum is induced to a pressure of 15 mmHg. A 10-mm, 0° operative telescope is used. The working space, already created by the gas, is progressively enlarged by moving the tip of the telescope, used as a palpator to free retroperitoneal fibrous tissues, behind the kidney. The spermatic vessels are identified after visualization of the ureter and psoas muscle. Manual traction of testicle may help to identify them. The testicular vessels are dissected, coagulated with bipolar electrocautery and then divided (Figure 2).
Results
In 1992 Hagood et al. reported that the laparoscopic camera during a varicolectomies provided a microscopic view, the arteries were easily observed, and the internal spermatic veins were not difficult to clip and divide, and that postoperatively overall patients had less pain than other procedures (10). Donovan and Winfield had a similar experience with laparoscopic varicocelectomies and, in addition, they reported improvement in the postoperative semen parameters (11).
About intraoperative complications after laparoscopic Palomo techique Ralph et al. reported a vasal injury that required a vasovasostomy and Jarow et al. reported a genitofemoral nerve injury (12,13). Despite these complications of the early cases, Peters reviewed the status of laparoscopy in pediatric urology and predicted that these procedures would become more efficient with experience and they would continue to increase in number (14).
About postoperative complications Esposito et al. reported 19 complications among 211 children (9.0%) which included 14 hydroceles, 3 with scrotal emphysema, 2 with umbilical granulomas, and 5 with recurrences (15).
Reports have shown a wide range of variability for incidence of postoperative hydrocele for different techniques from 1% to 40.4% (16-20).
The hydrocele occurred because of no sparing of lymphatic vessels and probably closure of veins and arteries involves closure of many lymphatics. In retroperitoneoscopic approach recurrence of hydrocele reported for this technique varies from 2.2% to 25%, while the results of laparoscopic approach showed very low recurrence because allows better vision of collateral veins (21).
About the ways to avoid hydroceles Oswald et al. (22) introduced the idea of preoperative dye injections into the subdartos space before Palomo procedures in adolescents. They injected 2 mL of isosulfan blue, and the lymphatics were clearly stained in 24 of 28 patients. There were no hydroceles or recurrences among those who were stained successfully. Methylene blue was avoided because this dye may cause local tissue reactions. Ishibashi et al. (23) used Indigo carmine because there has been extensive experience with this dye in cases of lymphatic mapping and sentinel node identification in cases of breast cancer. If 1–2 lymphatic channels were preserved during a varicocelectomy, there were no postoperative hydroceles.
In 2014 Esposito et al. have described a technical standardization of laparoscopic lymphatic sparing varicocelectomy in children using isosulfan blue with an intra-dartos/intratesticular injection that have showed to be significantly better than the previously described intra-dartos injection (Figure 3), permitting to identify lymphatic vessels in 100% of cases in our series, without evidence of allergy to isosulfan blue (24).
Recent papers have justified the increase of testicular volume for intratesticular interstitial edema, but other follow-up reveal this is because of a real growth of testis that improves with time (25,26). Many cases in the literature showed improvement in sperm quality after varicocelectomy; however, the data are few because spermiogram analysis cannot be obtained at pediatric age (27).
Mancini et al. in 2014 have also to analyzed the volume of testis and the quality of semen in patients treated with both minimally invasive approaches (transperitoneal approach and retroperitoneoscopy approach) (21). They have showed that all patients showed a progressive increase in volume of left testis until this reached equal size to the right testis. This is very important because it showed the excellent catch-up growth of affected testes after removal of the deleterious effect of varicocele.
Sautter et al. reported a prospective randomized comparison of laparoscopy versus antegrade sclerotherapy, and they raised the question of costs. The disposables were 316 euros for the laparoscopic procedures which were twice as high as the 160 euros for sclerotherapy, but Friedersdorff et al. recently reported laparoendoscopic single-site varicocelectomies with reusable components. The costs were lower with these procedures, and the outcomes were similar to conventional laparoscopies (28,29).
Borruto et al. presented a review of the literature and a meta-analysis that compared laparoscopic versus open varicocelectomy in children and adolescents. They retained 11 studies for statistical analysis. Overall, they concluded that there were no differences between the procedures for recurrence and postoperative hydrocele rates. However, among the laparoscopic group, the recurrences were higher for patients who had artery ligation, but the rate of hydrocele formation was less among patients who had dye injections before their procedures. The authors concluded that with specific planning, the results of laparoscopic surgery are comparable to other surgical procedures, but the laparoscopic approach has the advantage to simultaneously treat bilateral varicoceles (8).
Another recent survey of pediatric urologists found that the most common surgical approach to adolescent varicocelectomy was laparoscopic (38%), for better view and easier training (30).
Discussion
Laparoscopies were first used for the diagnosis of intra-abdominal pathology but, over time, most hospital had laparoscopic instruments that were used for a variety of procedures, like laparoscopic varicocelectomy that was introduced in Spain in 1988 and produced a new minimally invasive surgical approach by Palomo’s technique for treatment of varicocele (31).
In 1996, Gaur proposed retroperitoneoscopic surgery in adults, and in 1999 Valla introduced retroperitoneoscopic surgery to a pediatric population (32,33).
The anesthetic risk is similar in both approaches, while the difference between the two w minimally invasive methods is significant; whereas transperitoneal laparoscopy offers a large operative space through three incisions that improves the surgical time and magnifies the vision of abdominal cavity, retroperitoneoscopy decreases the injury to the abdominal wall because of one incision that allows physiological access to the spermatic vessels, does not use bladder catheterization and does not cause postoperative ileus, but it requires more surgical experience for a smaller operative space (34). The most commonly reported complications for any varicocelectomy technique include varicocele recurrence and hydrocele formation, and it occurred because of no sparing of lymphatic vessels and closure of veins and arteries involves closure of many lymphatics, and in retroperitoneoscopic approach, where the surgeon make a virtual space in which CO2 is introduced and so the operating area is very limited, it may happen most probably the closure of lymphatic ducts. With a standardization of laparoscopic lymphatic sparing technique during varicocelectomy using an intra-dartos/intratesticular injection it was showed that can be simple to identify lymphatic vessels in 100% of cases, and to avoid the occurrence of postoperative hydrocele.
Actually, the ideal surgical technique for adolescent varicocelectomy remains controversial and is usually dependent on surgeon preference. While a subinguinal microsurgical approach has become the gold standard for varicocele ligation in adult males with infertility, a microsurgical approach was reported in only 2% of children and adolescent patients.
Several concerns have been raised regarding the application of subinguinal microsurgical varicocelectomy to pediatric patients. Inexperience or lack of familiarity with the microscopic technique is perhaps the most significant obstacle to more widespread adoption of this approach among pediatric urologists (35,36).
Furthermore, complex entanglement of smaller vasculature in pediatric patients is another potential challenge. While testicular atrophy has not been reported after spermatic vein ligation above the internal ring, this rare complication has been associated with inguinal and subinguinal approaches (37).
In a recent survey of 131 pediatric urologists, Pastuszak et al. in 2014 reported that the preferred surgical approaches were laparoscopic (38%), subinguinal microsurgical (28%), inguinal (14%), and open Palomo (13%). The authors note that management of pediatric varicocele appears to have remained stable over the past decade, with a shift toward increasing use of a laparoscopic technique (30).
Conclusions
Literature have showed that laparoscopic varicocelectomy is the most commonly reported surgical approach in adolescent patients, it gained traction, as pediatric urologists have become increasingly facile with laparoscopic techniques, and that the distribution of surgical approaches appeared to have remained relatively stable from 2003 to 2014 (30,36,37).
The reasons for this discrepancy with the other techniques are that it offers a great view of the intracorporeal space; in fact for the surgeons the arteries were easily observed, and the internal spermatic veins were not difficult to clip and divide. It is a minimally invasive technique and then it provides a good postoperative course, with less pain and hospitalization, and it permit to avoid post operative hydrocele that is a principal compliance after Palomo technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics committee of 236/2016.
References
- Dubin L, Amelar RD. Etiologic factors in 1294 consecutive cases of male infertility. Fertil Steril 1971;22:469-74. [Crossref] [PubMed]
- Hopps CV, Goldstein M. Varicocele: unified theory of pathophysiology and treatment. AUA Update Series 2004;23:90-5.
- Diamond DA. Adolescent varicocele. Curr Opin Urol 2007;17:263-7. [Crossref] [PubMed]
- Mehta A, Goldstein M. Microsurgical varicocelectomy: a review. Asian J Androl 2013;15:56-60. [Crossref] [PubMed]
- Diamond DA, Gargollo PC, Caldamone AA. Current management principles for adolescent varicocele. Fertil Steril 2011;96:1294-8. [Crossref] [PubMed]
- Thomas JC, Elder JS. Testicular growth arrest and adolescent varicocele: does varicocele size make a difference? J Urol 2002;168:1689-91; discussion 1691.
- Esposito C, Monguzzi GL, Gonzalez-Sabin MA, et al. Laparoscopic treatment of pediatric varicocele: a multicenter study of the italian society of video surgery in infancy. J Urol 2000;163:1944-6. [Crossref] [PubMed]
- Borruto FA, Impellizzeri P, Antonuccio P, et al. Laparoscopic vs open varicocelectomy in children and adolescents: review of the recent literature and meta-analysis. J Pediatr Surg 2010;45:2464-9. [Crossref] [PubMed]
- Esposito C. Transumbilical open laparoscopy: a simple method of avoiding complications in pediatric surgery Pediatr Surg Int 1997;12:226-7. [Crossref]
- Hagood PG, Mehan DJ, Worischeck JH, et al. Laparoscopic varicocelectomy: preliminary report of a new technique. J Urol 1992;147:73-6. [PubMed]
- Donovan JF, Winfield HN. Laparoscopic varix ligation. J Urol 1992;147:77-81. [PubMed]
- Ralph DJ, Timoney AG, Parker C, et al. Laparoscopic varicocele ligation. Br J Urol 1993;72:230-3. [Crossref] [PubMed]
- Jarow JP, Assimos DG, Pittaway DE. Effectiveness of laparoscopic varicocelectomy. Urology 1993;42:544-7. [Crossref] [PubMed]
- Peters CA. Laparoscopy in pediatric urology. Urology 1993;41:33-7. [Crossref] [PubMed]
- Esposito C, Valla JS, Najmaldin A, et al. Incidence and management of hydrocele following varicocele surgery in children. J Urol 2004;171:1271-3. [Crossref] [PubMed]
- Misseri R, Gershbein AB, Horowitz M, et al. The adolescent varicocele. II: the incidence of hydrocele and delayed recurrent varicocele after varicocelectomy in a long-term follow-up. BJU Int 2001;87:494-8. [Crossref] [PubMed]
- Szabo R, Kessler R. Hydrocele following internal spermatic vein ligation: a retrospective study and review of the literature. J Urol 1984;132:924-5. [PubMed]
- Belloli G, Musi L, D'Agostino S. Laparoscopic surgery for adolescent varicocele: preliminary report on 80 patients. J Pediatr Surg 1996;31:1488-90. [Crossref] [PubMed]
- Riccabona M, Oswald J, Koen M, et al. Optimizing the operative treatment of boys with varicocele: sequential comparison of 4 techniques. J Urol 2003;169:666-8. [Crossref] [PubMed]
- Nyirády P, Kiss A, Pirót L, et al. Evaluation of 100 laparoscopic varicocele operations with preservation of testicular artery and ligation of collateral vein in children and adolescents. Eur Urol 2002;42:594-7. [Crossref] [PubMed]
- Mancini S, Bulotta AL, Molinaro F, et al. Surgical retroperitoneoscopic and transperitoneoscopic access in varicocelectomy: duplex scan results in pediatric population. J Pediatr Urol 2014;10:1037-42. [Crossref] [PubMed]
- Oswald J, Körner I, Riccabona M. The use of isosulphan blue to identify lymphatic vessels in high retroperitoneal ligation of adolescent varicocele--avoiding postoperative hydrocele. BJU Int 2001;87:502-4. [Crossref] [PubMed]
- Ishibashi H, Mori H, Yada K, et al. Indigo carmine dye-assisted lymphatic-sparing laparoscopic Palomo varicocelectomy in children. J Med Invest 2014;61:151-5. [Crossref] [PubMed]
- Esposito C, Iaquinto M, Escolino M, et al. Technical standardization of laparoscopic lymphatic sparing varicocelectomy in children using isosulfan blue. J Pediatr Surg 2014;49:660-3. [Crossref] [PubMed]
- Greene DR, Shabsigh R, Scardino PT. Urologic ultrasonography. In: Walsh PC, Retik AB, Stamey TA, et al. editors. Campbell's Urology. Philadelphia: W.B. Saunders Company, 1992:340-89.
- Cimador M, Pensabene M, Sergio M, et al. Focus on paediatric and adolescent varicocoele: a single institution experience. Int J Androl 2012;35:700-5. [Crossref] [PubMed]
- McIntyre M, Hsieh TC, Lipshultz L. Varicocele repair in the era of modern assisted reproductive techniques. Curr Opin Urol 2012;22:517-20. [Crossref] [PubMed]
- Sautter T, Sulser T, Suter S, et al. Treatment of varicocele: a prospective randomized comparison of laparoscopy versus antegrade sclerotherapy. Eur Urol 2002;41:398-400. [Crossref] [PubMed]
- Friedersdorff F, Aghdassi SJ, Werthemann P, et al. Laparoendoscopic single-site (LESS) varicocelectomy with reusable components: comparison with the conventional laparoscopic technique. Surg Endosc 2013;27:3646-52. [Crossref] [PubMed]
- Pastuszak AW, Kumar V, Shah A, et al. Diagnostic and management approaches to pediatric and adolescent varicocele: a survey of pediatric urologists. Urology 2014;84:450-5. [Crossref] [PubMed]
- Puleo S, Di Cataldo A, Li Destri G, et al. Microsurgical treatment of varicocele. Int Surg 1989;74:253-6. [PubMed]
- Gaur DD. Retroperitoneoscopic stenting of the ureter. Br J Urol 1996;78:945-7. [Crossref] [PubMed]
- Valla JS, Colomb F, Son S, et al. Mini-invasive surgery of the retroperitoneal space in children. Ann Urol (Paris) 1999;33:328-32. [PubMed]
- Diamond D. Adolescent versus adult varicoceles--how do evaluation and management differ? J Urol 2009;181:2418-9. [Crossref] [PubMed]
- Park K, Cho SY, Kim SW. The surgical difficulty of microsurgical subinguinal varicocelectomy is similar regardless of age. J Urol 2011;186:2397-401. [Crossref] [PubMed]
- Chan PT, Wright EJ, Goldstein M. Incidence and postoperative outcomes of accidental ligation of the testicular artery during microsurgical varicocelectomy. J Urol 2005;173:482-4. [Crossref] [PubMed]
- Fine RG, Franco I. Laparoscopic orchiopexy and varicocelectomy: is there really an advantage? Urol Clin North Am 2015;42:19-29. [Crossref] [PubMed]