Percutaneous endoscopic treatment for urinary stones in pediatric patients: where we are now
Introduction
Urinary tract stones represents still an emerging problem not only in adult patients, but also in pediatric age. Renal and ureteral calculi seem to present increasing frequency in western countries during the last five decades, if compared to the lower tract urinary stones that are more commonly observed in tertiary world countries (1,2). Dietary factors, malnutrition or hyperproteic alimentation, metabolic abnormalities and environmental changes have been postulated as influencing the urinary stone development in children growing up in different socio-economical situations (3,4).
In the recent three decades, innovative and less invasive urological procedures have been introduced progressively in children affected by urolithiasis, coming from the experience on adult patients. Extracorporeal shock waves lithotripsy (SWL) and endo-urological procedures, as percutaneous nephrolithotomy (PCNL), endoscopic uretero-lithotripsy (ULT) and retrograde intrarenal surgery (RIRS), have almost totally superseded the open surgical treatment in adults and adolescent patients. More recently, these less invasive techniques have been extended in pediatric age (5,6), although not fully adopted in Pediatric Surgery and Pediatric Urology Centers also in developed Countries. The European Association of Urology (EUA) guidelines recommend SWL as first line treatment for pyelo-calyceal stones in pediatric age similarly to adult age patients (7). The endoscopic procedures are a more recent valid alternative to SWL, with higher stone free rate and reduced number of repeated treatments (8,9). PCNL has been demonstrated as highly efficacious for treatment of large or staghorn pyelo-calyceal stones in pediatric patients, with a limited risk of complications, mainly bleeding (10,11). Retrograde endoscopic procedures as RIRS may offer to-day good alternative to percutaneous approaches, with good stone free rate and less complications risk (12,13). Very recently a new percutaneous method has been offered, mainly for lower calyx stones presenting limited dimension (less than 20 mm diameter) utilizing a all-seeing metallic needle and laser lithotripsy under direct vision through a very delicate optic fiber: the micropercutaneous (Microperc) procedure (14).
Not complete agreement exist at the moment on the most efficacious and most safe modality for treatment of renal stone disease in pediatric age patients. We analyzed our recent experience on upper tract stones in children and we reviewed the indications, results and limitations of the newly offered endo-urological approaches, with the aim to give an overview on this specific field of pediatric endo-urology.
Methods
We retrospectively evaluated the records of all the patients admitted to the Division of Pediatric Urology of our Hospital from January 2011 to December 2015. The study was approved by the Institutional Ethics Committee and written informed consent was obtained from all patients. Inclusion criteria were: age younger than 18 years, presence of calculi in the upper urinary tract (pyelo-calyceal system and ureter), unilateral or bilateral, single or multiple. Exclusion criteria were: contraindications to general anesthesia, attendant different illness as oncological disease or coagulation abnormalities, severe mental retardation. Specific informed consent was obtained from parents before any urological treatment.
Preoperative evaluation included familial and personal medical history, urinalysis and urine culture, blood laboratory investigations including blood cells count, coagulation profile, creatinine, protein and electrolytes serum levels. Renal ultrasonography (US) and plain abdomen X-ray (XR) was performed in all patients. Non contrast computerized tomography (CT) was performed in selected cases for quantitative assessment of the stone burden and to better define the stone number and localization. Pre-treatment determination of Hounsfield units on TAC has been used to distinguish the more hard stones as (cysteine, struvite) from other types of calculi and better address the urological lithotripsy treatment.
For any patient, the adopted treatment was chosen between the different options that were available on our center: SWL, ULT, RIRS, PCNL or Microperc. The choose was given considering the stone size, number and position within the urinary tract, metabolic disorders, Hounsfield units if available. Body weight and age of the patients and possible associated abnormalities were also considered. All the percutaneous procedures (PCNL and Microperc) performed in our centre in the last 5 years were analyzed in the present study.
PCNL technique
All procedures were performed with the patient in the supine Valdivia modified Galdakao position (15), under general anesthesia by oro-tracheal intubation (Figure 1). Contrast material was injected through an occluding open tip ureteral catheter for opacification of the pyelo-calyceal system. Calyceal puncture was performed under fluoroscopic and US combined guidance. Dilation of the nephrostomy access was obtained by Amplatz dilators up to 24 Fr. A 22 Fr nephroscope (Karl Storz, Tubingen, Germany) was used in all cases. Ballistic energy was used for stone fragmentation, by a 1.9 Fr probe. Flexible nephroscope or ureteroscope (Karl Storz, Flex-x-2 Tubingen, Germany, and Olympus 8–4.8 Fr, Germany) were utilized indifferently for extraction of residual stone fragments by basket and for ancillary lithotripsy using Holmium:YAG laser energy by 220–335 micron fibers. A nephrostomy tube was placed for 2 to 5 post-operative days and a 4.7 Fr double-J ureteral stent was removed cystoscopically at 3–5 weeks after the PCNL procedure. Alternatively, a 5 Fr open tip indwelling ureteral catheter was left with a transurethral Foley catheter during the 2–3 post-operative days.

Microperc technique
The patient was placed in the supine Valdivia modified Galdakao position under general anesthesia, similarly to the PCNL procedure (15,16). An open end 5 Fr ureteral catheter was placed trans-urethral till the uretero-vesical junction. The proper calyceal access was carefully selected by ultrasonographic and fluoroscopic guidance. A 4.85 Fr metallic needle was used to perform the percutaneous puncture of the selected calyx, usually on the lower calyceal group through the lower pole of the kidney. When the collecting system access was achieved, the inner stylet was removed and a three-way connector was attached to the sheath. A 0.9 mm high resolution optic flexible wire was connected with the telescope (Polydiagnost, Germany). Intermittent saline irrigation was done through the other side port by manual control. Attention must be payed to avoid any bleeding in the access to the pelvis and calyx, by very delicate and precise maneuvers and avoiding to repeat the calix puncture. A 200 micron laser fiber was passed through the central port of the connector. Stone lithotripsy was performed under direct vision using Holmium: YAG laser with high frequency and low dose (0.6–0.8 Joule) energy (Sphinx 30 W laser machine, USA Laser, Pleasanton, California, United States). Complete stone clearance was assessed by fluoroscopy before removal of the needle. No nephrostomy tube was left. The transureteric catheter and the Foley bladder catheter were removed within 18–36 hours, if no significant bleeding or pain was observed.
Post-operative evaluation and follow-up
Renal US and plain abdominal (kidneys, ureters and bladder) X-ray were performed at 1 and 3 months post-operatively. Stones clearance was defined as no residual calculi or asymptomatic fragments less than 4 mm diameter, considered as clinically insignificant residual fragments (CIRF).
Demographic data, stones characteristics (number, dimensions, position), metabolic evaluation, operative technique were recorded. Post-operative pain assessment was detected by the “face-legs-activity-cry-consolability” scale (FLACC) or the “visual analogic scale” (VAS) and by Paracetamol requirement (15 mg/kg body weight, at 6-hour intervals, if needed). Hemoglobin decrease and complications according to the Clavidien-Dindo classification (17) were detected. The need of ancillary procedures was recorded on a specific prospective data base.
Statistical analysis was performed using the Chi-square test to compare categorical data and the Mann-Withney U-test to compare continuous data, as appropriate.
Results
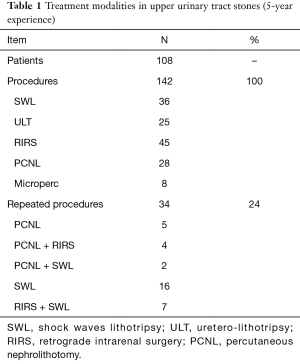
A total number of 108 patients (56 males and 52 females) presenting symptomatic upper tract urinary stones were included in the data base from January 2011 to December 2015. Metabolic disorders were present in 6 patients (3 hypercalciuria and 3 cystinuria). Body mass index was higher than normal in 4 patients, 3 treated by PCNL and 1 by Microperc. The overall number of procedures was 144, as 56 patients (25%) received more than one procedure during the study period of time (Table 1). The distribution of the different treatment modalities is shown in Figure 2.
Full table
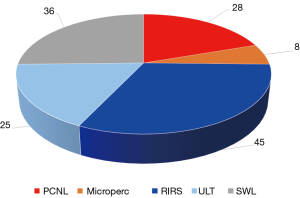
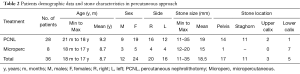
Percutaneous procedures were 36 (25%) performed in 32 patients (4 bilateral procedures): 28 were PCNL and 8 were Microperc. The demographic data of the treated patients and the stone characteristics are resumed in Table 2. Patient age was moderately higher in PCNL (mean age 9.2 years) versus Microperc (mean age 8.7 years). The difference was not significant. Female sex was significantly more affected than male in both groups (PCNL and Microperc) of patients treated by percutaneous endoscopic access (P>0.05). The stone size was higher in the PCNL group (mean diameter =19 mm), if compared to Microperc (mean stone diameter =15 mm). The distribution of the stone location within the pyelo-calyceal system is shown in Table 1: the distribution was pyelic and multiple calyceal (staghorn stone) in 11 PCNL treatment and pyelic in 14 PCNL, whereas lower calyx stones were more frequent in Microperc procedures.
Full table
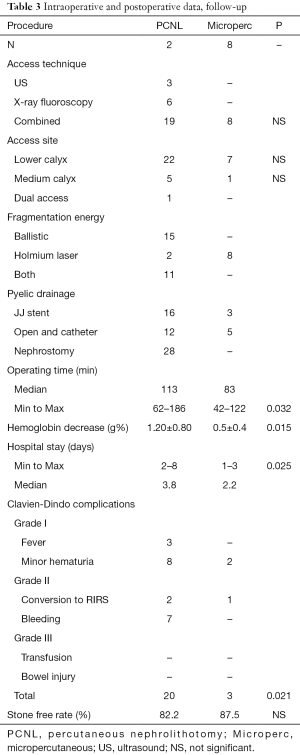
The main intra-operative data are resumed in Table 3. The calix for percutaneous access was selected by combined technique (US and fluoroscopy) an all the Microperc cases and in 19 out of 28 PCNL procedures (67.8%). One of the lower calyceal system was mostly used as access site, but medium calyx was selected in 5 PCNL and in 1 Microperc, depending to the stones position. In a case, 2 access were necessary. The energy for fragmentation was ballistic in PCNL, combined with laser during flexible nephroscopy in 11 procedures (39.3%). Holmium: YAG laser was the only energy utilized in Microperc.
Full table
A nephrostomy tube was left for 2–6 days (median 3.6 days) in all the PCNL procedures and in no one Microperc. The operative time was significantly longer in PCNL (62–186 min, median 113 min) than in Microperc (42–127 min, median 83 min). Patients who underwent Microperc presented very little or no hemoglobin decrease, compared to patients to patients treated by PCNL, who had 1.20±0.80 mg% hemoglobin dropdown. No transfusions were needed in all our series. Patients in the PCNL group presented significantly gross hematuria, compared to Microperc group (15 versus 2 cases, P=0.030), and fever in the immediate post-operative period. Anyway, complications have been minor or minimal, corresponding to the grade I and grade II of the Clavidien-Dindo classification (17). Conversion to RIRS was necessary in three cases: one Microperc procedure, due to stone mobilization in a middle calyx, and two PERC for difficult management of upper and lower pole stone residuals.
All the eight cases of Microperc were stone free at 3 months follow-up, whereas the stone free status was achieved in 24 out of 28 PCNL procedures. In 4 cases, all staghorn calculi (2 cysteine and 1 struvite), significant residual stones were left in lower pole calyx, requiring further procedures.
Discussion
Renal lithiasis is still a significant problem in pediatric age patients, for the uncertain urological approach and for the higher risk of recurrence long life, if compared with adults. The open procedures, as nephrolithotomy, pyelolithotomy, ureterolithotomy or cystolithotomy that were currently used till the 80’ in pediatric age patients, are classically associated with considerable morbidity and long hospital stay with lengthy convalescence (8). These invasive procedures have been progressively abandoned during the last three decades, mimicking the experience of endo-urological techniques in adult patients (18). In fact, surgical management of urolithiasis has evolved dramatically, as consequence of the advent of SWL in adult patients and its following gradual application in pediatric age (8,18).
SWL is currently considered the procedure of choice in treating most upper tract calculi of small dimension, in children similarly to adult patients, offering tremendous advantages over the open surgical procedure (5). SWL is considered as low-risk procedure, requiring no general anesthesia and no hospitalization in adults and grown-up children. The European Association of Urology (EAU) guidelines still recommend SWL as first line treatment for pyelo-calyceal stones in pediatric similarly to adult age patients (19). However, SWL has high re-treatment rate and high incidence of residual fragments in calyx and pelvis, with a risk of ureteral secondary obstruction (“stein-strasse”), despite many advancements in technology (20).
Not all the stones are amenable to SWL, especially in children, who often require general anesthesia with short hospitalization for pain control and adequate immobilization during the extracorporeal treatment (5,8). The advent of minimally invasive endoscopic treatments in adult patients has been revolutionized by the introduction of endoscopic techniques and by the more recent improved technology with miniaturization of the instrumentation (20,21). These mini-invasive endoscopic techniques, as PCNL and RIRS, have been very recently proposed and progressively adopted in pediatric patients, also in young age in an increasing number of Urology centers (5,9). RIRS has been adopted for small volume nephrolithiasis, especially as the risk of injury to the abdominal viscera and significant bleeding is much lower when compared to PCNL (21,22). However, flexible ureteroscopy often requires the placement of a Double J stent before or after the procedure, with a not marginal risk of a second endoscopic procedure for ureteral stent removal in children (21).
The introduction of PCNL offered a new approach for difficult cases of large or staghorn pyelo-calyceal calculi in adult and pediatric age. PCNL has established as an effective technique with high stone free rate, often with a single treatment and short time. The biggest limitation of PCNL is its relatively higher morbidity, with serious complications as significant bleeding and viscera trauma, if compared with SWL and RIRS (20,23,24). Concerns regarding PCNL in children raised from the size of the instruments in relation to the patient’s body weight and the characteristics of the pediatric kidney (small size and hypermobility) with higher risk of kidney injury and blood loss (21,23,25). Anyway, a well conducted PCNL is regarded as more efficacious and less invasive than open surgery in large or staghorn renal stones. Consequently, PCNL should be offered more often in children (10,11). A reduced tract size has been demonstrated as associated to a reduction in morbidity from PCNL (24,26). Recent developments in PCNL have been addressed to create a reduced tract size in the attempt to reduce the complication rate of this procedure. Various minimally invasive percutaneous approaches have been proposed very recently: mini-percutaneous nephrolithotomy (mini-PCNL) and smaller (ultra-mini-PCNL), micro-percutaneous nephrolithotomy (micro-PCNL) (27-30).
The mini-perc uses a 12–14 F size nephroscope through a 15–18 F Amplatz sheath, instead of the 22–26 F endoscopes within a 24–30 F size Amplatz sheath, to reduce the invasiveness of the procedure. A recent prospective randomized controlled trial on 70 patients showed that Mini-perc presented high free stone rate (85.7%) and low complications rate, compared to RIRS (97% stone free rate) for stones larger than 10 mm in diameter, with similar operative time, hemoglobin decrease and hospital stay (31). Interestingly, the visual analogue score (VAS) for pain assessment showed higher pain and analgesic requirements were higher in the RIRS group of patients than in the mini-perc, evaluated at 1 hour postoperatively (31,32). More recently, a further advancement has been proposed by the Ultra-Mini-Percutaneous (UMP) nephrolithotomy, utilizing a 3 F telescope (1 mm) with a special 7.5 F nephroscope introduced through a 11–13 F sheath (20). In a recent study, Authors reported that UMP was an effective and safe procedure for managing stones up to 20 mm in a series of 120 adult patients, offering an attractive alternative to SWL and to RIRS for managing small stones (20).
A further significant step towards miniaturization, now at the end of the spectrum of diameters of percutaneous access, is represented by the Microperc procedure (29-31). The technique utilizes a 4.8 F “all-seeing” needle, that is introduced percutaneously under US and/or fluoroscopy guidance into the selected calyx without any working sheath. Stone fragmentation is carried out utilizing laser energy through a 220 micron fiber. As consequence of the lake of using an Amplatz sheath, the outlet of the irrigation fluid and the stone fragments clearing can be obtained through the pyelo-ureteric way, through an open tip transureteric catheter (14). Microperc seems to be effective in lower pole intra-calyceal calculi, less than 20 mm in diameter (31-34). These conclusions were confirmed in a recent randomized controlled trial comparing Microperc to RIRS in management of small renal calculi (35).
In our 5-year experience, we performed 142 procedures in 108 pediatric patients presenting upper urinary tract stones, with a 24% rate of repeated procedures, mostly after SWL. Percutaneous treatments were 36 (25%), 28 perc or mini-perc and 8 Microperc (Table 1). The youngest patient who received PCNL was 21 and 18 months old in the Microperc group. Very few patients have been treated by PCNL or Microperc under the age of 2 years and published in literature, till now (6,9,10,11,13,14,18,19,21,33,35,36). The risk of complications, including abdominal viscera injury, renal trauma, urine leakage and mainly significant bleeding was reported as up to 27% (26). We adopted Microperc in 8 children, 7 presenting stone in a lower pole calyx and 1 in renal pelvis. We consider the ideal indication for Microperc procedure the stone in the lower calyceal system, with a diameter less than 20 mm. The pure pyelic stones have the risk of migration in a calyx during lithotripsy, especially if pelvis is dilated. This complication happened in 1 case, a 7-year-old girl, who presented 13 mm lower calyx stone and mild pyelo-calyceal dilation, requiring conversion to RIRS procedure to obtain the free stone status.
The Valdivia modified Galdakao position allows contemporaneous antegrade approach by percutaneous access and retrograde approach by ureteroscopy or RIRS, without mobilizing the patient on the operative table (14). Figure 1 shows the patient position that we adopted in all our percutaneous procedures. A combined approach may be used as procedure of choice to better define the selected calyx for percutaneous puncture by initial retrograde uretero-renoscopy (14). In our experience, a Microperc procedure was converted easily in a RIRS for migration of the stone in a different calix, not suitable for the percutaneous mini-invasive procedure (Table 3).
The operative time was shorter in the Microperc procedures, compared with the PCNL (median time 83 versus 113 min, P=0.032), but the stone size was smaller in the Microperc group (mean 15 mm) than in PCNL (19 mm) (Tables 2,3). Intraoperative complications are almost frequent in percutaneous procedures, especially in pediatric age patients, referred from 5% up to 27% (22,26). The most serious complication is the bleeding risk from the renal access, referred as 5–12% (26). In our series, the hemoglobin decrease was evaluated 1.20±0.80 g% in the PCNL, and 0.5±0.4 g% in the Microperc group of patients. Bleeding was referred as significant in seven PCNL patients (grade II of Clavidien-Dindo classification). Interestingly, no patient of our series required blood transfusion. The stone free rate was 82.2% in the PCNL group and 87.5% in the Microperc group after a single procedure (Table 3). These results are slightly lower than in other series of the literature (6,10,11,13,31,32), but it could be related to a particular attention to avoid endoscopic maneuvers excessively aggressive or invasive, especially in young children, in the attempt to reduce the risk of severe urological complications.
In conclusion, the treatment of renal and ureteral lithiasis still represents a significant problem worldwide in pediatric urological and nephrological units, as consequence of the increasing prevalence, the high risk of recurrence long life and the difficulty to choice the right therapeutic option (8,13). In the recent three decades, surgical management of urolithiasis in children has evolved dramatically. In fact, minimally invasive endo-urological procedures have progressively superseded the open surgical procedures for the treatment of upper urinary tract stones. SWL, being noninvasive, remains the treatment of first choice for most upper tract calculi in children. However, the recent significant improvements in endo-urological techniques and in miniaturization of the urological instruments are making minimally invasive endoscopic (percutaneous and retrograde) procedures as effective and attractive options (10,13,22). Nevertheless, it is necessary to stress that PCNL and RIRS are both less invasive procedures if compared to open surgery, but are not free of risks especially in very young children, for the reduced size and high mobility of the pediatric kidney and the small diameter of the ureter and the uretero-vesical junction (10,23).
More recently, significant advances have been offered in endoscopic instruments, with the development of smaller endoscopes and effective energy sources, as laser-tripsy for stone disintegration. Retrograde ureteroscopic treatments have become increasingly applicable in children of low body weight presenting upper tract stones (12,13). Similarly, small size percutaneous access, as mini-perc, UMP or Microperc, have been very recently presented as safer than classic PCNL in children (19,35) and more effective than SWL (36). But the risk of iatrogenic lesions on the ureter or of other severe complications as significant bleeding from the percutaneous intrarenal access must be not underestimated (23,37). The urological surgeon, who desire to face with pediatric upper tract lithiasis, must be familiar with the endoscopic equipment and must act with prudence and experience, because the consequences of a wrong endo-urological maneuver can be severe in young patients (18,38). Complete instruments availability, specific expertise in pediatric endo-urological procedures and adequate nephrological and anesthesiological support are needed in a coordinated multidisciplinary organization, as in a “Pediatric Stone Center”, offering the facilities needed to any child presenting stone disease (2,24). In this quickly evolving panorama, percutaneous treatments are still reducing invasiveness and increasing efficacy and safety, and present a specific role in the urological armamentarium of any pediatric canter dealing with upper tract stones.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Ethics Committee (CE/279/10) and written informed consent was obtained from all patients.
References
- Granberg CF, Baker LA. Urolithiasis in children: surgical approach. Pediatr Clin North Am 2012;59:897-908. [Crossref] [PubMed]
- Caione P, Matarazzo E, Battaglia S. Stone treatment in children: where we are today? Arch Ital Urol Androl 2010;82:45-8. [PubMed]
- Saxena A, Sharma RK. Nutritional aspect of nephrolithiasis. Indian J Urol 2010;26:523-30. [Crossref] [PubMed]
- Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol 2004;15:3225-32. [Crossref] [PubMed]
- D'Addessi A, Bongiovanni L, Racioppi M, et al. Is extracorporeal shock wave lithotripsy in pediatrics a safe procedure? J Pediatr Surg 2008;43:591-6. [Crossref] [PubMed]
- Raza A, Turna B, Smith G, et al. Pediatric urolithiasis: 15 years of local experience with minimally invasive endourological management of pediatric calculi. J Urol 2005;174:682-5. [Crossref] [PubMed]
- Tekgul S, Radmayr C, Dogan HS et al. Urinary stone disease. In: Guidelines on Paediatric Urology. Amhem: European Association of Urology and European Society for Paediatric Urology, 2015:51-9.
- Salerno A, Nappo SG, Matarazzo E, et al. Treatment of pediatric renal stones in a Western country: a changing pattern. J Pediatr Surg 2013;48:835-9. [Crossref] [PubMed]
- Desai M. Endoscopic management of stones in children. Curr Opin Urol 2005;15:107-12. [Crossref] [PubMed]
- Kumar R, Anand A, Saxena V, et al. Safety and efficacy of PCNL for management of staghorn calculi in pediatric patients. J Pediatr Urol 2011;7:248-51. [Crossref] [PubMed]
- Desai MR, Kukreja RA, Patel SH, et al. Percutaneous nephrolithotomy for complex pediatric renal calculus disease. J Endourol 2004;18:23-7. [Crossref] [PubMed]
- Kim SS, Kolon TF, Canter D, et al. Pediatric flexible ureteroscopic lithotripsy: the children's hospital of Philadelphia experience. J Urol 2008;180:2616-9; discussion 2619. [Crossref] [PubMed]
- Unsal A, Resorlu B, Kara C, et al. Safety and efficacy of percutaneous nephrolithotomy in infants, preschool age, and older children with different sizes of instruments. Urology 2010;76:247-52. [Crossref] [PubMed]
- Caione P, De Dominicis M, Collura G, et al. Microperc for pediatric nephrolithiasis: technique in valdivia-modified position. Eur J Pediatr Surg 2015;25:94-9. [PubMed]
- Valdivia Uría JG, Valle Gerhold J, López López JA, et al. Technique and complications of percutaneous nephroscopy: experience with 557 patients in the supine position. J Urol 1998;160:1975-8. [Crossref] [PubMed]
- Ibarluzea G, Scoffone CM, Cracco CM, et al. Supine Valdivia and modified lithotomy position for simultaneous anterograde and retrograde endourological access. BJU Int 2007;100:233-6. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Saad KS, Youssif ME, Al Islam Nafis Hamdy S, et al. Percutaneous Nephrolithotomy vs Retrograde Intrarenal Surgery for Large Renal Stones in Pediatric Patients: A Randomized Controlled Trial. J Urol 2015;194:1716-20. [Crossref] [PubMed]
- Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol 2016;69:475-82. [Crossref] [PubMed]
- Agrawal MS, Agarwal K, Jindal T, et al. Ultra-mini-percutaneous nephrolithotomy: A minimally-invasive option for percutaneous stone removal. Indian J Urol 2016;32:132-6. [Crossref] [PubMed]
- Ozden E, Sahin A, Tan B, et al. Percutaneous renal surgery in children with complex stones. J Pediatr Urol 2008;4:295-8. [Crossref] [PubMed]
- Unsal A, Resorlu B. Retrograde intrarenal surgery in infants and preschool-age children. J Pediatr Surg 2011;46:2195-9. [Crossref] [PubMed]
- Goyal NK, Goel A, Sankhwar SN, et al. A critical appraisal of complications of percutaneous nephrolithotomy in paediatric patients using adult instruments. BJU Int 2014;113:801-10. [Crossref] [PubMed]
- De S, Autorino R, Kim FJ, et al. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol 2015;67:125-37. [Crossref] [PubMed]
- Childs MA, Rangel LJ, Lingeman JE, et al. Factors influencing urologist treatment preference in surgical management of stone disease. Urology 2012;79:996-1003. [Crossref] [PubMed]
- Onal B, Dogan HS, Satar N, et al. Factors affecting complication rates of percutaneous nephrolithotomy in children: results of a multi-institutional retrospective analysis by the Turkish pediatric urology society. J Urol 2014;191:777-82. [Crossref] [PubMed]
- Ganpule AP, Bhattu AS, Desai M. PCNL in the twenty-first century: role of Microperc, Miniperc, and Ultraminiperc. World J Urol 2015;33:235-40. [Crossref] [PubMed]
- Desai M, Mishra S. 'Microperc' micro percutaneous nephrolithotomy: evidence to practice. Curr Opin Urol 2012;22:134-8. [Crossref] [PubMed]
- Bader MJ, Gratzke C, Seitz M, et al. The "all-seeing needle": initial results of an optical puncture system confirming access in percutaneous nephrolithotomy. Eur Urol 2011;59:1054-9. [Crossref] [PubMed]
- Desai MR, Sharma R, Mishra S, et al. Single-step percutaneous nephrolithotomy (microperc): the initial clinical report. J Urol 2011;186:140-5. [Crossref] [PubMed]
- Sabnis RB, Ganesamoni R, Ganpule AP, et al. Current role of microperc in the management of small renal calculi. Indian J Urol 2013;29:214-8. [Crossref] [PubMed]
- Lee JW, Park J, Lee SB, et al. Mini-percutaneous Nephrolithotomy vs Retrograde Intrarenal Surgery for Renal Stones Larger Than 10 mm: A Prospective Randomized Controlled Trial. Urology 2015;86:873-7. [Crossref] [PubMed]
- Tepeler A, Armagan A, Sancaktutar AA, et al. The role of microperc in the treatment of symptomatic lower pole renal calculi. J Endourol 2013;27:13-8. [Crossref] [PubMed]
- Silay MS, Tepeler A, Atis G, et al. Initial report of microperc in the treatment of pediatric nephrolithiasis. J Pediatr Surg 2013;48:1578-83. [Crossref] [PubMed]
- Sabnis RB, Ganesamoni R, Doshi A, et al. Micropercutaneous nephrolithotomy (microperc) vs retrograde intrarenal surgery for the management of small renal calculi: a randomized controlled trial. BJU Int 2013;112:355-61. [Crossref] [PubMed]
- Hatipoglu NK, Sancaktutar AA, Tepeler A, et al. Comparison of shockwave lithotripsy and microperc for treatment of kidney stones in children. J Endourol 2013;27:1141-6. [Crossref] [PubMed]
- Akman T, Binbay M, Sari E, et al. Factors affecting bleeding during percutaneous nephrolithotomy: single surgeon experience. J Endourol 2011;25:327-33. [Crossref] [PubMed]
- Smaldone MC, Docimo SG, Ost MC. Contemporary surgical management of pediatric urolithiasis. Urol Clin North Am 2010;37:253-67. [Crossref] [PubMed]


