The problems related with primary repair for tetralogy of Fallot, especially about transannular patch repair
Since the initial surgical correction of tetralogy of Fallot (TOF) in 1954, advances in management have helped reduce early surgical mortality to less than 2% (1). During six decades, the surgical approach has shifted from repair via a right ventriculotomy to a transatrial-transpulmonary approach, as many congenital cardiac surgeons consider relieving right ventricular outflow tract (RVOT) obstruction with preserving pulmonary valve competence as important factors to guarantee long term outcomes (2-4). The STS database reported the recent trend in TOF operations, which revealed over 60% surgeries still using transannular patch enlargement (TAPE) (5). These data suggested us to consider the reason of using TAPE. Recent trends revealed many centers used the pulmonary valve annulus (PVA) z-score to determine whether to apply the TAPE procedure, but the cutoff value for this measure varies among studies (−1.3 to −4) (6,7).
In the current issue of Annals of Thoracic Surgery, Choi et al. reported the usefulness of the great artery annulus size ratio [pulmonary valvular annulus size to aortic valve annulus size (GA ratio)] to predict TAPE in patients with TOF (8). Between January 2007 and March 2015, 122 patients who underwent TOF repair by a single surgeon (S.C.S.) at Pusan National University Yangsan Hospital were enrolled. The median age (25th, 75th percentile) at total repair was 6.2 (IQR, 5.1–8.3) months, and the median body weight was 7.1 (IQR, 6.0–8.4) kg. Forty patients (32.8%) required TAPE, and there was no perioperative mortality or reoperation for TAPE of the PVA. Seven patients (5.7%) needed postoperative intervention for left pulmonary artery stenosis, and 4 patients (3.3%) needed reoperations: one for a posterior aortopexy of the descending aorta, one for subaortic fibrous ridge resection, one for pulmonary valve replacement, and one for an infundibulectomy. Postoperative pulmonary regurgitation (≥ moderate) was more frequent in the TAPE group (77.5% vs. 26.8%, P<0.0001). Postoperative pulmonary stenosis (>30 mmHg) was found in 3 (7.5%) in the TAPE group and 7 (8.5%) in the non-TAPE group. The comparison between GA ratio and TAPE to predict TAPE in their institution was shown in Table 1. They revealed the GA ratio to be superior to predict TAPE in patients with TOF patients.
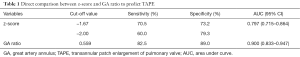
Full table
There are three major operative concerns about primary repair for patients with TOF; the timing of primary repair, palliation, and the detail of surgical methods (9). First, in this manuscript, Choi et al. discussed one of the surgical methodologies in detail. As previously mentioned, we have shifted towards valve-sparing surgery with the transatrial-transpulmonary approach. However, the choice for valve-sparing surgery varies greatly among institutions. For example, there are many more patients with patch repair (17.0% transannular patch; 62.0% right ventricular outflow patch) in Japan (10). On the other hand, in some limited institutions such as Pusan National University Yangsan Hospital, transannular patch repair was avoided whenever judged possible, resulting in a low rate of TAPE (only 32.8%). One of the major reasons not to choose valve-sparing surgery includes residual or late RVOT stenosis after surgery. Although Yoo et al. reported “proper relief of RVOT obstruction with acceptable residual stenosis” to be important, the clear definition of “proper” and “acceptable” has not been fully investigated. We still have to depend on the surgeon’s experience and art-based approach (10). However, using these obscure but practical indications, the reoperation rate due to residual pulmonary stenosis is not high. We usually use z-score, a tricuspid pulmonary valve, and a postoperative RV/LV pressure ratio as references to predict needing TAPE before operation (7). Choi et al. advocated the GA ratio. We should integrate these measures and continue to discuss how to treat patients.
Second, the timing of primary repair should also be discussed. The optimal timing of elective repair of an asymptomatic infant with TOF has been proposed between 3 and 12 months of age (11). Bové et al. suggested complete repair between 3 and 6 months of age, irrespective of symptom status or previous palliation (12). Neonatal primary repair is promoted in many centers. Unfortunately, these early primary repair results have been inconsistent (13,14). Woldu et al. revealed that neonatal total repair was associated with a high rate of TAPE, but with higher weight-for-age scores at 1 year (13). Under these circumferences, we should wait for more results about the primary repair at an early age. The median age at total repair of 6.2 (IQR, 5.1–8.3) months reported by Choi et al. reflects common practice.
Third, palliation should not be ignored. Whether palliation affects the long-term outcome and TAPE is still controversial. In addition to the Blalock-Taussig shunt, palliation includes several other procedures such as balloon pulmonary valvotomy and stenting (11,15). Usually shunt surgery accounts for more than half of all palliation methods. Because balloon palliation is considered by some to be beneficial in avoiding TAPE, it may be preferred to allow for future valve-sparing surgery (16).
Finally, in Japan, surgery with or without minimal right ventriculotomy has been developed in the early 1980s (17). Since then, there is still a high rate of transannular patch repairs with minimal right ventriculotomy. The most common indication for reoperation is not pulmonary regurgitation, but right ventricular outflow obstruction (32%) followed by right ventricular stenosis (29%), which is quite different from other countries (18). We are convinced that we should rather focus on the reason for TAPE and detailed surgical procedures, and find anatomical variables such as z-score and GA ratio reasonable adjuncts for decision-making. We should pay attention to GA ratio, considering this measure might only be applicable in young infants. As Van Praagh advocated, tetralogy of Fallot can be considered a “monology”, that it is just one basic malformation: underdevelopment of the pulmonary infundibulum (19). As the pulmonary valve and RVOT become more hypoplastic, aorta size increases, which results in a decreased GA ratio.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bacha EA, Scheule AM, Zurakowski D, et al. Long-term results after early primary repair of tetralogy of Fallot. J Thorac Cardiovasc Surg 2001;122:154-61. [Crossref] [PubMed]
- Boni L, García E, Galletti L, et al. Current strategies in tetralogy of Fallot repair: pulmonary valve sparing and evolution of right ventricle/left ventricle pressures ratio. Eur J Cardiothorac Surg 2009;35:885-9; discussion 889-90. [Crossref] [PubMed]
- Luijten LW, van den Bosch E, Duppen N, et al. Long-term outcomes of transatrial-transpulmonary repair of tetralogy of Fallot. Eur J Cardiothorac Surg 2015;47:527-34. [Crossref] [PubMed]
- Geva T. Tetralogy of Fallot repair: ready for a new paradigm. J Thorac Cardiovasc Surg 2012;143:1305-6. [Crossref] [PubMed]
- Al Habib HF, Jacobs JP, Mavroudis C, et al. Contemporary patterns of management of tetralogy of Fallot: data from the Society of Thoracic Surgeons Database. Ann Thorac Surg 2010;90:813-9; discussion 819-20. [Crossref] [PubMed]
- Awori MN, Leong W, Artrip JH, et al. Tetralogy of Fallot repair: optimal z-score use for transannular patch insertion. Eur J Cardiothorac Surg 2013;43:483-6. [Crossref] [PubMed]
- Stewart RD, Backer CL, Young L, et al. Tetralogy of Fallot: results of a pulmonary valve-sparing strategy. Ann Thorac Surg 2005;80:1431-8; discussion 1438-9. [Crossref] [PubMed]
- Choi KH, Sung SC, Kim H, et al. A novel predictive value for the transannular patch enlargement in repair of tetralogy of Fallot. Ann Thorac Surg 2016;101:703-7. [Crossref] [PubMed]
- Villafañe J, Feinstein JA, Jenkins KJ, et al. Hot topics in tetralogy of Fallot. J Am Coll Cardiol 2013;62:2155-66. [Crossref] [PubMed]
- Mizuno A, Niwa K. Transannular patch repair remains popular: the reasons for choosing the transannular patch should be discussed. Eur J Cardiothorac Surg 2015;47:1112. [Crossref] [PubMed]
- Mimic B, Brown KL, Oswal N, et al. Neither age at repair nor previous palliation affects outcome in tetralogy of Fallot repair. Eur J Cardiothorac Surg 2014;45:92-8; discussion 99. [Crossref] [PubMed]
- Bové T, François K, Van De Kerckhove K, et al. Assessment of a right-ventricular infundibulum-sparing approach in transatrial-transpulmonary repair of tetralogy of Fallot. Eur J Cardiothorac Surg 2012;41:126-33. [PubMed]
- Woldu KL, Arya B, Bacha EA, et al. Impact of neonatal versus nonneonatal total repair of tetralogy of fallot on growth in the first year of life. Ann Thorac Surg 2014;98:1399-404. [Crossref] [PubMed]
- Tamesberger MI, Lechner E, Mair R, et al. Early primary repair of tetralogy of fallot in neonates and infants less than four months of age. Ann Thorac Surg 2008;86:1928-35. [Crossref] [PubMed]
- Stumper O, Ramchandani B, Noonan P, et al. Stenting of the right ventricular outflow tract. Heart 2013;99:1603-8. [Crossref] [PubMed]
- Sluysmans T, Neven B, Rubay J, et al. Early balloon dilatation of the pulmonary valve in infants with tetralogy of Fallot. Risks and benefits. Circulation 1995;91:1506-11. [Crossref] [PubMed]
- Kawashima Y, Kitamura S, Nakano S, et al. Corrective surgery for tetralogy of Fallot without or with minimal right ventriculotomy and with repair of the pulmonary valve. Circulation 1981;64:II147-53. [PubMed]
- Mizuno A, Niwa K, Matsuo K, et al. Survey of reoperation indications in tetralogy of fallot in Japan. Circ J 2013;77:2942-7. [Crossref] [PubMed]
- Van Praagh R, Van Praagh S, Nebesar RA, et al. Tetralogy of Fallot: underdevelopment of the pulmonary infundibulum and its sequelae. Am J Cardiol 1970;26:25-33. [Crossref] [PubMed]


