A survey of neonatal births in the maternal departments in urban China 2005
Introduction
The morbidity and mortality of neonates varies by location. In 2002, a survey was sponsored by the subspeciality group of Neonatology, China Pediatrics Association to collect the data of preterm births. It was reported that the incidence of the preterm births was 7.8% of the neonates born in the department of obstetrics from 77 urban hospitals in 16 provinces. According to the reports from Hamilton and Slattery (1,2), the frequency of preterm births is about 12.7% in the USA and 5-9% in Europe and many other developed countries in 2005. There has no data on newborn births in a large scale investigation in China. Based on the results of 2002, a retrospective survey was performed for deliveries of live birth in maternity departments in 2005. We aimed to offer detailed data on number and characteristics of births in urban China and to present the epidemiology results of newborn infants born in the cities around China. This work was sponsored by the subspeciality group of neonatology, China Pediatrics Association.
Methods
Investigation subjects
Data shown in this report are based on the births registered. It includes detailed data on numbers and characteristics of births in 2005 from six geography areas of China such as northeast, north China, east China, northwest, southwest and central south. Live birth infants born in the maternity department from 72 tertiary public hospitals (mainly teaching hospitals) in 47 cities of 22 provinces in the above areas between Jan 1, 2005 to Dec 31, 2005 were enrolled into the investigation. Near 1,000 infants were investigated for each hospital.
Investigation methods
All characteristics of pregnant women in each area were documented before delivery and subsequently births were recorded by an enumerator resident in that hospital. Data were collected and filled in the standard forms designed by the sponsors to provide uniformity data and were input in the EpiData program set up by computer experts. All the investigators were trained before working. Statistical analyses were performed with SPSS version 11. Chi-square tests were used to identify possible associations between preterm and term infants. Logistic regression model was also used to identify possible risk factors for preterm labor.
Results
A total of 45,722 infants were delivered in the investigation period.
The distribution of gestational age and birth weight
Of all the infants, 91.9% of them were born at term gestation and 8.1% were preterm. The ratio of male to female was 1.13:1. The percentage of births delivered at all gestational age (<28, 28-31, 32-36, 37-41 and >42 weeks) was 0.3%, 0.9%, 6.9%, 91.4% and 1.5%, respectively. Whereas the percentage of birth weight (<1,000, 1,000-1,499, 1,500-2,499, 2,500-3,999 and >4,000 g) was 0.2%, 0.5%, 5.2%, 88.8% and 5.2%, respectively. The proportion of birth weight for preterm infants was 1.6% (weighing below 1,000 g), 6.6% (1,000-1,499 g), 40% (1,500-2,499 g), 51% (2,500-3,999 g) and 0.8% (weighing over 4000 g), respectively. The percentages of preterm deliveries before 37, 32, 28 weeks were 85.2%, 11.4% and 3.4%, respectively.
The social class of the parents
Fathers were aged 18-57 years (mean 30), 7.3% were under 25, 73.4% aged 25-34, 1.3% over 45. As for their social class, 23.9% were unskilled, 14.1% were professional, 11.1% were managerial, 15.4% were partly skilled, 22% were skilled non-manual and 13.5% were not stated. Information on educational attainment, 23.3% had bachelor’s diploma or higher, 67.9% had completed a high school education, 8.2% had primary education and 0.6% had no any education.
All fertility women were aged 17-48 years (mean 27 years). 69.5% aged 25 to 35, 0.8% under 20, 21.9% aged 20-24, 44.7% aged 25-29, 24.8% aged 30-35, 6.9% aged 35-40 and 0.9% aged over 40. The proportion (7.7%) of preterm delivery for women over 35 was significantly higher than that (5.1%) of term delivery for women of the same ages, P<0.01. Women’s occupations had a different distribution from those of men. 40% of them were unskilled, 16% were professional, 10.2% were managerial, 9.7% were partly skilled, 14% were skilled non-manual and 9.7% were not stated. Information on educational attainment, 18.8% had bachelor’s diploma or higher, 67.6% had completed a high school education, 13.3% had primary education and 1.1% had no any education.
Our data also presented that 0.1% parents were consanguineous. There was no significant difference of gestational age in parents who were related marriages. Family hereditary diseases were noted in 0.6% infants.
Pregnancy history
Data in this report presented that 99.7% of pregnancy women for term delivery were conceived pregnancies, whereas 0.3% were assisted reproduction. In pregnancy women at preterm delivery, 98.4% of them were natural conceived, 1.6% accepted assisted reproductive technology. In pregnancy women from assisted reproductive technologies, the proportion of preterm delivery (1.6%) was significantly higher than that of term delivery (0.3%) (χ2=138, P<0.01). Women who were at their primary pregnancy accounted for 43.3%, 30.6% were at their second pregnancies and 20.1% at least three previous pregnancies. The first birth rate was 67.9%, whereas the second- and third-order birth rates were 14.4% and 17.7%, respectively. In all the pregnancy women, 3.2% of them had a history of threatened abortion before 12 weeks of pregnancy, 4.2% developed pregnancy-associated hypertension with 57.4% of them were severe or eclampsia. Pregnancy associated hypertension was at a rate of 4.0% for women aged under 35 years and had increased to 8.5% for those aged over 35 years (χ2=113.22, P<0.01). The incidence of preterm pre-labor rupture of the membranes (pPROM) was 13.4%, and 48.6% of them were 6 hours before delivery, 21.7% between 7-12 hours and 12.9% over 24 hours before delivery.
Women who had a history of abortions were 3.3%, and 9.6% of them were spontaneous abortions, whereas 0.7% of women had the history of preterm labor with 45.1% of infants delivered at 28-32 weeks, 39.9% at 33-36 weeks and 1.5% under 28 weeks.
History of delivery
As with all births, most of the infants (94.6%) were singletons, 5.4% were multiple births. The total vaginal delivery rate was 50.8% including using of forceps or breech extraction (1.1%). Total cesarean delivery rate was 49.2%, most of it (38.1%) was due to non-clinically indicated cesarean delivery (maternal requesting for).
Apgar score and the outcomes of newborn infants
The percentage of infants who had an Apgar score of less than 7 at 1 minute was 4.8%, 1.0%of them were less than 3. Infants with an Apgar of less than 7 at 5 minute were 1.6% and 0.6% were less than 3. Infants had an Apgar of less than 7 at 10 minute were 1.1% and 0.5% were less than 3.
For all infants born in the maternal departments, 3,265 infants (7.14%) were admitted to neonatal units due to preterm births (27.5%), asphyxia (16.4%), hyperbilirubinemia (14.1%), high risk infants (10.7%), VLBW (4.4%), pneumonia (4.0%), meconium aspiration syndrome (3.3%), congenital anomalies (2.7%), macrosomia (2.3%) and multiple births (1.9%). Death rate was 0.74% for all admitted infants.
Comparison of preterm to term infants
Our data showed that the incidences for assisted reproduction, drug treatment during pregnancy, threatened abortion, pPROM, vaginal bleeding, history of spontaneous abortion or stillbirth, multiple births, fetal intrauterine distress and neonatal asphyxia in women born preterm births were much more common in mothers aged over 35 compared to those under 35 (Table 1).
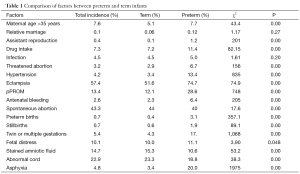
Full table
Analysis of risk factors in preterm births
Logistic regression analysis was performed to evaluate each factor for preterm births. In all factors for preterm births, the incidences of women aged 35 and over, use of fertility-enhancing therapies, drug treatment during pregnancy, history of threatened labor, pregnancy-associated hypertension, pPROM, pre-labor bleeding, history of spontaneous abortion as well as still births, preterm labor, multiple births and fetal distress were all higher than those for term births. pPROM (28.6% vs. 19.8%, 2002), multiple births (17.1% vs. 19.8%, 2002), pregnancy-associated hypertension (13.4% vs. 12.6%, 2002), history of spontaneous abortion (11.9% vs. 36.8%, 2002), fetal intrauterine distress (11.1%), abnormal fetal position (10.4% vs. 5.3%, 2002), women aged 35 and over (7.7%) and previous history of preterm labor (3.1% vs. <2%, 2002). Table 2 showed more factors affected preterm birth.
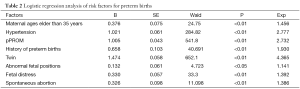
Full table
Comparison the data of preterm infants in 2002 and 2005
Data from the survey of preterm births between 2002 and 2003 by the same methods was used to comparing the results of 2005. It showed that the percentages of preterm births (8.1% vs. 7.8%, P>0.05), pregnancy-associated hypertension (13.4% vs. 12.6%), history of abortion (40.4% vs. 36.8%, P<0.01) and pPROM (28.6% vs.19.8%, P<0.01) had risen in 2005 compared to 2002-2003 whilst the rate of recovered infants in 2005 was higher than that in 2002 (Table 3).
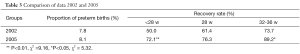
Full table
Discussion
The morbidity and the mortality of neonates are related to the economic status, medical levels and the health care for both newborn and maternal conditions. The mortality of neonates declines with the development of economics and the advance of technology. According to the Statistic Bulletin of Chinese Health Service in 2006, the neonatal mortality of the whole country was 22.8% in 2000, 20.7% in 2002, 15.4% in 2004 and 13.2% in 2005, whilst neonatal mortality in our report was 7.4% in 2005. The different results were due to being not generalizable to the country as a whole and they are not a sample of all births. The data presented that the percentage of premature delivery was 8.1% in urban China, which was lower than the report for America 2007 (12.7%) (3), but higher than that of China in 2002-2003 (7.8%). Indicating an increasing of premature delivery in China. The low birth weight (LBW) rate (40%) and the percentage of very low birth weight (6.6%) in our data were largely different from those for America in 2007 (8.2% and 1.49%, respectively) (4).
We showed in this report factors such as pPROM, preterm twins, pregnancy-associated hypertension, fetal distress, abnormal fetal position, mothers aged over 35, history of spontaneous abortion or premature delivery were risk for preterm births. Prenatal care provided by a health care professional during pregnancy may enhance newborn and maternal health by assessing risk, providing health care advice and managing pregnancy - related health conditions.
Cesarean sections are common when dealing with high-risk pregnancies. The proportion of births delivered by cesarean section in this report was 49.2%. Most of which was due to women’s preference for CS and their belief in its safety and comfortableness by this method of delivery. In addition, CS is more profitable for the supply side than vaginal delivery, which results in a continued rise in delivery expenditures and an unnecessarily high resource consumption. Proportion as high as 60.8% was reported by some maternity units (5,6). This was mostly due to an inappropriate concept from both pregnancy women and their relatives, as well as obstetricians amplifying indications for cesarean delivery to decrease morbidity and mortality (7). Although caesarean section is a common mode which can save the lives of both mothers and infants, its associated complications could not be ignored. It has been reported that the mortality and the incidence of complications after cesarean sections are 1 to 3 times higher than after vaginal deliveries. Furthermore, they do not decrease neonatal birth asphyxia (5,8). Neonates who have not experienced the contraction in active labor or the absence of vaginal squeeze are more likely to develop wet lung, amniotic fluid aspiration, asphyxia, respiratory distress syndrome, etc. In 1980s, WHO proposed that the proportion of cesarean delivery should not be higher than 15%. The total cesarean delivery rate in America was 31.8% in 2007 and was higher for multiple gestations (3). It was from 5% to 20% in many Western countries, whilst in a global survey report from nine Asia countries (Cambodia, China, India, Japan, Nepal, Philippines, Sri Lanka, Thailand, and Vietnam), the overall rate of caesarean section was 27.3% (9). Therefore, paying more attention to antenatal care and the health information, improving obstetricians’ views and restricting the indication to medical reasons for cesarean delivery may be an important work for the health care department of China.
Our data showed that the incidence of asphyxia neonates was 4.8%. It was even 5-11% in some hospitals, which was much higher than that of most developed countries. The incidence of neonatal asphyxia in Iceland was 0.94% (1997 to 2001) (9) and 0.09% in United Kingdom in 2005 (10). Effective resuscitation combining obstetricians and pediatricians is important to prevent long term outcomes after birth asphyxia (11). What we should do is to be careful with prenatal care for optimum pregnancy outcome and promptly treat pregnancy complications to reduce the morbidity and mortality.
In 2006, a program set by Ministry of Health on neonatal resuscitation guide aimed to train obstetricians and pediatricians throughout China. We are hoping that the incidence of morbidity and mortality and the sequelae following birth asphyxia insults will be declined in future. We are also looking forward to getting more data from most places of rural China.
This work was sponsored by the subspeciality group of Neonatology, Pediatric society, Chinese medical association.
Acknowledgements
The authors thank Dr. Sailesh Kotecha for critical correction of the manuscript and helpful suggestions.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2005. Natl Vital Stat Rep 2006;55:1-18. [PubMed]
- Slattery MM, Morrison JJ. Preterm delivery. Lancet 2002;360:1489-97. [PubMed]
- Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2007. Natl Vital Stat Rep 2010;58:1-85. [PubMed]
- Wei Ke-Lun, Yang Yu-Jia, Yao Yu-Jia, et al. An initial epidemiologic investigation of preterm infants in cities of China. Chin J Contemp Pediatr 2005;7:25-28.
- Lu YQ, Nong WZ. A retrospective analysis of cesarean section rate of ten years. Guangxi Med 2004;26:1001-2.
- Fan ZS. An analysis of cesarean section delivery and social factors of five years. J Med Forum 2007;28:50-1.
- Zhang SX. An analysis of 1724 cesarean section delivery. J Chin MisDiagno 2007;7:306.
- Huang SH, Huang YM. An etiologic analysis of higher cesarean section delivery. Maternal Child Heal Care Chin 2005;20:1813-4.
- Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet 2010;375:490-9. [PubMed]
- Becher JC, Stenson BJ, Lyon AJ. Is intrapartum asphyxia preventable? BJOG 2007;114:1442-4. [PubMed]
- Palsdottir K, Dagbjartsson A, Thorkelsson T, et al. Birth asphyxia and hypoxic ischemic encephalopathy, incidence and obstetric risk factors. Laeknabladid 2007;93:595-601. [PubMed]


